Search
-
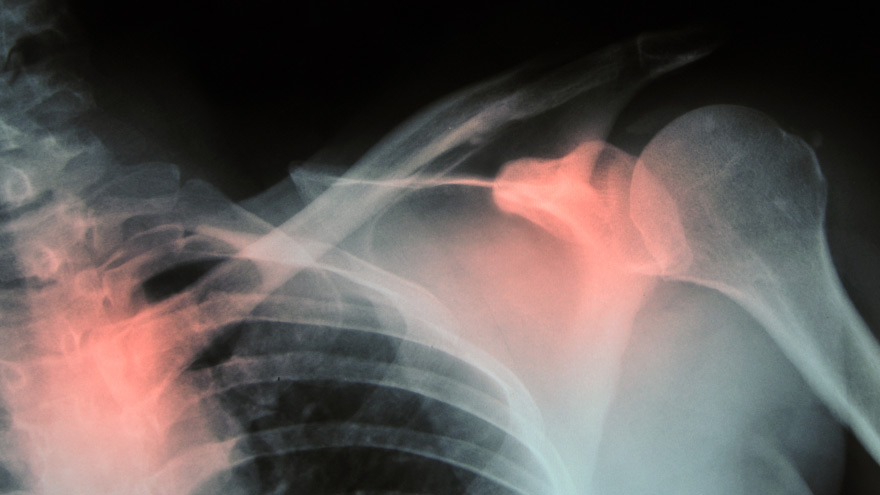
Prevent Osteoporosis: Take Control of Your Bone Health Today
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
Alzheimer’s Disease – How to Spot the Signs
Alzheimer’s disease is not normal forgetfulness as we age. Instead, it is a specific form of mental decline. And according to the Alzheimer’s Association it accounts for nearly 80 percent all dementia cases. Natasa Dragicevic, MD, PhD., behavioral neurologist and Alzheimer’s disease specialist with Renown Institute for Neurosciences, weighs in on diagnosing it and the importance of early medical action. How to Diagnose Alzheimer’s Disease In general, the signs of Alzheimer’s disease occur slowly, getting worse over time. For example, forgetfulness is a daily search – for shoes, keys and other misplaced items. Not only is memory affected, but also speech patterns and behavior. There is no single test for Alzheimer’s disease. “Specifically, a neurologist should be the one to diagnose Alzheimer’s disease given differences in presentation,” clarifies Dr. Dragicevic. “And ideally a behavioral neurologist (Alzheimer’s sub-specialist) will be managing the treatment,” she adds. Brain Imaging Diagnosing Alzheimer’s disease involves multiple approaches and medical providers. In short, medical history is reviewed along with a physical exam, lab tests and other diagnostic testing. “A medical workup includes a variety of tests. These include MRI and other brain imaging, as well as neurological and psychological testing. Furthermore, a lumbar puncture is performed to look for markers of the disease,” she states. What Causes Alzheimer’s disease? Although no one knows the cause, researchers think many factors play a role. Uncontrollable risk factors include your genetics and having a family member with the disease. However, the controllable risk factors include: reducing the risk of head injury and keeping your heart healthy. It’s important to realize that high blood pressure, high cholesterol, stroke and diabetes play a role in brain health. Blood loss to the brain causes vascular dementia, leading to long-term blood vessel damage. Symptoms of Alzheimer’s disease Generally speaking, the signs of this disease differ in each person. Yet noticeable behaviors include: • Losing the way to familiar places • Forgetting to pay bills • Trouble finding the right words when talking • Repeating questions • General confusion • Social withdrawal Alzheimer’s Disease – Benefits of Early Diagnosis Equally important, spotting Alzheimer’s disease early allows more time to benefit from medications and possible clinical trials. Likewise, nutrition and exercise changes can be made, increasing blood flow to the body, and perhaps delaying symptoms. Early diagnosis also allows for personal health decisions and quality-of-life conversations to take place. According to the Alzheimer’s Association, these benefits include: 1. Medical advantage 2. Emotional and social comfort 3. Time to plan ahead 4. Cost savings A Brain Supporting Lifestyle “At the present time, treatment is limited,” explains Dr. Dragicevic. “Usually Alzheimer’s is a progressive ongoing disease – any management at this time is purely symptomatic.” However, she states the following lifestyle changes can help support brain health: • New hobbies such as painting, pottery, music classes or learning a new language • Crosswords, puzzles and playing games, such as Scrabble • Brain challenging mobile apps, such as Luminosity • 30-45 minutes of mild to moderate physical activity per day, such as walking • Eating a Mediterranean diet (primarily plant based foods)
-
Get Moving: How to Exercise with Arthritis
An arthritis diagnosis doesn’t mean your exercise routine has to end. In fact, a consistent routine can actually improve mobility. Although stiff and painful joints can make it difficult to keep moving, staying active is essential for easing pain. October 11 is World Arthritis Day, so we asked Michelle Higgins, MPT at Renown Physical Therapy & Rehab some advice about exercising with arthritis. According to the Arthritis Foundation, arthritis affects one in five adults and 300,000 children. As a matter of fact arthritis is the nation’s leading cause of disability. Your joints certainly don’t need to suffer when you exercise. In general exercise is actually necessary for those with arthritis. Not only does it reduce joint pain, but it also increases strength and flexibility. Furthermore those adopting a regular exercise routine also have more energy, deeper sleep and find it easier to maintain a healthy weight. “Exercise is a necessary component to managing your arthritis,” says Higgins. “Consistent participation in an exercise program has been shown to promote long-term pain relief, increased body function and an improved quality of life. Alternatively, a lack of exercise can actually increase joint pain or stiffness and eventually lead to long term disability and suffering.” Exercising With Arthritis Exercise truly is the most effective non-drug arthritis treatment available for reducing pain and improving movement. And it can even include daily activities like gardening, dancing or walking your dog. Of course talk to your doctor or physical therapist about what exercises fit into your specific treatment plan. With this is mind, the four specific components below are important to an effective arthritis exercise program: Range of motion Moving joints through their full available range of movement is important. This frequently increases function and decreases joint stiffness and pain. For this reason, aim to complete these exercises daily. Examples include bending, straightening, and rotating specific joints, or static and dynamic stretching. Strengthening These exercises target muscles supporting and protecting our joints and bones. Strengthening is also necessary for weight control, so two-to-three sessions per week are recommended. In order to allow your body to adapt, begin with light resistance and start slow. Strength exercises include weightlifting and using resistance bands. Low-impact aerobic exercise Aerobic exercise is certainly necessary for overall well-being, weight management and heart health. Aim for two-to-three sessions a week. Low-impact exercises include walking, swimming, cycling, elliptical machine exercises and water aerobics. Balance Good balance is also vital for an effective arthritis program. On the positive side, solid balance prevents falls by increasing your ability to stay upright whether you are moving or sitting still. Likewise, it improves your confidence with walking and daily activities. In order to keep excellent balance, incorporate daily balance exercises. Examples of balance exercises include the use of an exercise ball, Tai Chi and exercises such as standing on one foot. Start Slow, Finish Strong As you begin your exercise program, remember to listen to your body. Start slowly – it can take several weeks for your body to adjust to exercise. Consult your doctor, or physical therapist, if you experience increasing pain or swelling which doesn’t go away with rest. Above all, incorporate fun and motivating activities so you’ll stick to them long term and improve your results. Renown Physical Therapy & Rehab 775-982-5001 Through outpatient physical, occupational and speech therapy, Renown Physical Therapy & Rehab gives you hands-on, individualized treatment in convenient Reno/Sparks locations. We have the latest, most advanced physical therapy and rehab equipment, specialty services and treatments. Renown Physical Therapy & Rehab is now open on Robb Drive in addition to three additional locations in Reno and Sparks. Call 775-982-5001 or visit us online.
-
Making Patient Safety the Priority It Deserves to Be
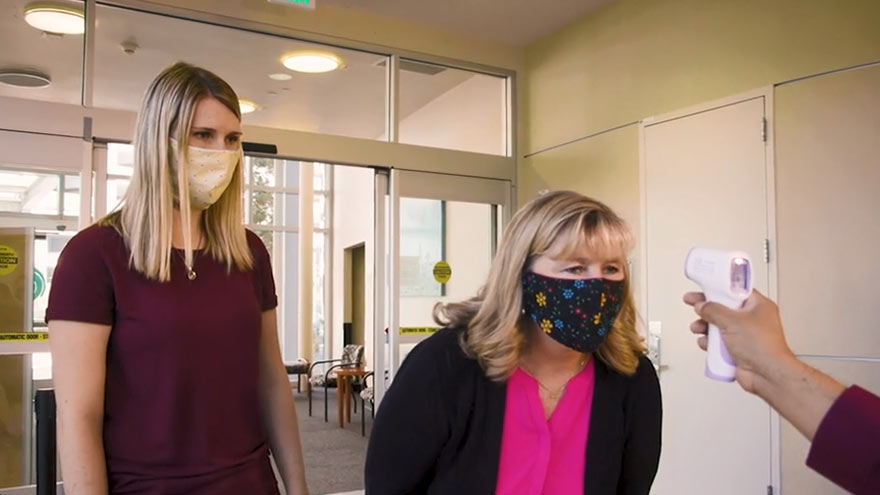
I am regularly amazed by medical advancements and innovation in the United States. However, even as we make significant progress in many areas of medicine, there is still much more work to be done in others. One such area is patient safety. What is Patient Safety? When we talk about patient safety, we are discussing how hospitals and healthcare organizations protect patients from errors, injuries and infections. Anyone can make a mistake at work, but in healthcare these mistakes can result in serious outcomes. In 1999, the Institute of Medicine released a report that estimated 98,000 deaths per year result from medical examination or treatment. The most recent study in 2013 suggested these numbers could range from 210,000 to 440,000 deaths per year. Many of these deaths result from preventable medical errors. This is inexcusable and shows how much more work our industry still needs to do to improve patient safety. Making Patient Safety a Priority Patient Safety is our number one priority at Renown Health. We dedicate a lot of time to establishing, reviewing, and revising our processes to prevent errors. Despite the obvious importance of patient safety, this issue is largely left to individual hospitals and health systems to manage. There is a surprising lack of national attention around this truly important issue. However, a silver lining of the COVID-19 pandemic is that it is igniting interest in hygiene and infection prevention. Patients want to learn more about the processes that are in place to prevent the spread of infections. In addition to the many protocols that guide our treatment of injuries and illness, Renown Health has implemented the following measures to prevent the spread of communicable diseases: Requiring everyone entering Renown sites to wear a mask or face covering. Establishing new processes to help patients and visitors practice social distancing. Limiting the number of visitors in our facilities. Screening all employees and patients for symptoms. Enhancing our already-thorough cleaning and disinfection processes. I hope patient safety and infection prevention remain in the national spotlight long after the COVID-19 pandemic has ended. The healthcare industry must come together to develop stronger systems and regulations to minimize preventable medical errors. We have a responsibility to our patients to do better.
Read More About Making Patient Safety the Priority It Deserves to Be
-
Addressing the Threat of Workplace Violence in Hospitals
In recent years, workplace violence against healthcare workers has been on the rise. According to the Occupational Safety and Health Administration (OSHA), about 75 percent of nearly 25,000 reported annual workplace assaults occur in healthcare and social service settings. Those who don’t work in healthcare may be surprised to learn that violent altercations are so common in our field. Hospital settings can create fear and stress for patients and their families. Pain, mind-altering medications and drugs, and difficult prognoses can amplify these feelings. While inappropriate responses may be understandable, violence cannot be tolerated. As the leader of a health system, protecting our employees is an issue that I take seriously. Reporting Workplace Violence Unfortunately, sometimes employees don’t report dangerous incidents fearing they might be blamed, or not realizing it’s a reportable offense. At Renown Health, we take these events seriously. We have clear, mandatory policies and protocols for reporting and investigating violent incidents. Each incident is investigated to ensure follow through and accountability. We also teach de-escalation skills to our hospital security teams, clinicians, and other frontline employees. As an added layer of protection, Renown Health has a first-rate security team that closely monitors activity on our campuses, addressing potential issues before they escalate. Our organization values our partnerships with community organizations including local law enforcement agencies like the Washoe County Sheriff’s Office and the Reno Police Department. Renown Health maintains a close relationship with these partners, and we alert them when our care teams experience an increase in violent incidents. I also recognize that workplace violence is a national problem that demands collaborative solutions. That’s why I am also proud to serve as a member of the American Hospital Association’s Hospitals Against Violence Advisory Committee. Nurses, doctors, paramedics, and frontline health workers care for us every day. It’s our responsibility to support them by ensuring they feel safe at work.
Read More About Addressing the Threat of Workplace Violence in Hospitals
-
Bone Fractures in Children Honest Expert Advice
Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis, answers some common questions about bone fractures. Is there a difference between broken bones and fractures? No, these are two different names for the same injury. Of course the common term is a broken bone. Using either name will describe your concerns. Medical personnel typically describe a broken bone as a fracture to a specific bone. For example, a broken wrist is also a fractured distal radius. To clarify, this describes the injured bone and the precise location. How do I know if my child has broken their bone? Many times children will fall and complain of their arm or leg hurting. In most cases the pain goes away and the child will return to their activities. When there is a deformity to the limb (curve in arm) and the child is complaining of pain, it is probably a fracture. If the arm or leg looks straight, look to see if there is any swelling or bruising. Both are signs of a possible fracture. Finally, if the limb looks normal but the child continues to complain, gently push on the bone. Likewise if it causes the same pain, then they likely have a fracture and should have an x-ray. My child fractured their growth plate, what does this mean? Growth comes from this area of the bone. In detail, these are located all over the body but typically at the end of the bones. With this in mind, fractures to these areas can result in the bone growing abnormally. Because of potential shortening of the arm or leg, or bones growing crooked, it is important to follow fractures closely (up to 1-2 years or longer). It is better to identify a problem early. Small problems can be treated with small surgeries. What if the bones of the x-ray do not line up? Because children are growing, unlike adults, their bones will remodel and straighten with growth. The amount of remodeling occurring depends on a child’s age, the bone fractured and the location. In many cases an angled bone will grow straight over the course of a year. For this reason, someone with experience in caring for children needs to follow bone growth. How long does it take fractures to heal? Factors deciding when a cast can come off include: Child’s age. Bone fractured. Fracture location. Young children heal faster than teens, teens heal faster than young adults, who heal faster than older adults. In young children most fractures heal in 4-6 weeks. However, teens generally take 6 weeks to heal, and adults can take much longer. Although your child is out of their cast, it may not be healed completely to return to all activities. Placing a splint is during this time is common. This typically gives them added protection for several weeks after their cast is removed - in case they forget their limitations. What if my child is still limping? Whether a child is in a walking or non-weight bearing cast, removing it often leaves them stiff and sore. Therefore many children will walk as though they still have a cast in place. In most cases this resolves in about three weeks. Regardless, if your child is still limping or walking abnormally after three weeks, contact the treating doctor. They may benefit from physical therapy or a repeat evaluation. (This article was original published in the July 2019 issue of South Reno Kids & Sports.)
Read More About Bone Fractures in Children Honest Expert Advice
-
What is Dry Drowning?
Whether you're a parent, grandparent, caregiver or sibling, you should know drowning is the second leading cause of death among children. Yet, while we are vigilant about protecting children from water accidents and drowning, a condition known as dry drowning or delayed drowning can go unnoticed. In fact, most people aren't even aware it exists. Dry drowning defined Dry drowning is a side-effect of a near-drowning experience and includes spasms of the vocal cords and larynx — known as a laryngospasm. This occurs when the body attempts to shut down the passage of any liquid into the lungs. Unfortunately, it can also shut down the passage of air into the lungs and force fluid into the stomach and lungs. Often the condition is not discovered until it's too late — severe cases can cause death within one to 24 hours after a water incident occurs. Who is susceptible? Novice or first-time swimmers are at increased risk, as are children with asthma and known breathing issues. In addition, children who have had pneumonia or experienced acute respiratory distress syndrome are also at greater risk. To reduce these factors, caregivers should be exceptionally watchful of inexperienced swimmers. According to Leland Sullivan, MD, of Northern Nevada Emergency Physicians, children under the age of 5 are most susceptible to drowning and often drown in residential swimming pools. Infants less than 1-year-old most often drown in bathtubs. What are the signs of a dry drowning episode? If your child has a near-drowning incident, a few moments of coughing until they calm down is normal. However, you should know the more severe signs and symptoms to watch for during the 24 hours following the incident, including: Persistent coughing Difficulty breathing and/or shortness of breath Chest pains Extreme fatigue and/or lethargy Change in typical behavior Face becomes pale What is the treatment and prognosis for dry drowning? Dr. Sullivan recommends that all victims of near-drowning incidents seek medical attention, even if they have no symptoms. If caught early, dry drowning can be treated. If you think your child is experiencing a dry drowning episode, go to the nearest emergency room as quickly as possible — do not attempt treatment at home. Healthcare professionals will work to supply oxygen to your child's lungs to restore and regulate breathing.
-
Alzheimer's Safety Tips for Caregivers to Know
November is National Alzheimer’s Disease Awareness Month. At Renown Health, we know that Alzheimer's safety for your loved one is a priority, as the symptoms can sometimes lead to unsafe situations. We asked Dr. Jonathan Artz – a neurology physician with Renown Health and an assistant professor of clinical neurology at the University of Nevada, Reno School of Medicine – for tips on keeping loved ones safe and secure. According to the Alzheimer’s Association, Alzheimer’s disease affects safety in various ways, specifically due to body and brain adjustments. These changes can include: Judgment, including forgetfulness Sense of place – getting lost on the way home Behavior – being suspicious or fearful Body difficulty – losing balance Sensing ability – noticeable sensitivity in hearing, seeing or temperature Dr. Artz gives us four major tips to ensure your loved one’s safety as you both navigate this disease together. Watch for Wandering Those experiencing Alzheimer’s disease tend to wander and get lost. Try the following tips to reduce the risk of wandering: Get your loved one an ID bracelet and have them wear it at all times. You can also enroll your loved one in “Wandering Support.” Install door chimes so you know when exterior doors are open. Ask neighbors to call you if they see your loved one out alone. Go with your loved one when they insist on leaving the house. Don’t argue or yell. Instead, use distraction or gentle hints to get them to return home. Discourage Driving Driving can be unsafe for someone with this disease. With this in mind, ask a doctor whether it’s safe for your loved one to drive. For example, on a case-by-case basis, there are certain situations where doctors are required to report individuals with particular cognitive impairments, wherein a form of a driving assessment will be recommended. Limit access to the car. Keep the keys with you or lock them away. Ask an authority figure, such as an insurance agent or a doctor, to tell them not to drive. Adult-Proof Your Abode A simple living space is a safe living space. This means reducing clutter and removing any issues that may pose a safety concern. You may also want to get advice from an occupational therapist (home safety expert). Keep in mind that some changes may not be needed right away. Focus on major safety concerns first. Try the following tips: Add lighting (or glow-in-the-dark tape) to brighten dark areas, including stairways and halls. Use color contrast or texture indicators for dials, knobs and appliance controls. Remind your loved one not to carry items while walking to avoid a fall. Remove sharp objects from drawers and countertops. Avoid using small throw rugs or doormats, as they are easy to trip on. Move frequently used items so that they are easy to reach. Lock away alcohol and tobacco products, as they are not recommended for dementia patients. Install handrails in the shower, tub and near the toilet. Bathroom falls are especially common. Adjust the setting on your hot water heater so water does not scald. Those with Alzheimer’s can lose their sensitivity to temperature. Move and lock up hazardous chemicals and cleaning supplies, such as bleach and insecticides. Disable and remove guns or any weapons. Supervise any medication taken by your loved one. Promote a Positive & Healthy Lifestyle Continually emphasize the strengths of your loved one by promoting participation in meaningful activities, wellness visits and healthy habits to help them improve their well-being. Here are some ways to keep them physically and mentally active: Maintain regular vision and hearing screenings and make necessary adaptations. Establish a routine for daily activities. Encourage participation in self-care and leisure activities. Work with your loved one’s doctor to establish a healthy diet. Ensure proper hydration. It may help to set reminders for your loved one to drink fluids. Encourage regular exercise. Exercise delivers oxygen to the brain, improving brain health. Promote good sleep habits. Good quality sleep can increase overall brain health and has been associated with improving memory, attention and concentration. Resources and support are available with the Renown Memory Disorders Program. Providers within this program are specifically dedicated to treating several different memory-related disorders. Memory Disorders Resources & Support.
Read More About Alzheimer's Safety Tips for Caregivers to Know
-
Department Spotlight: Security
“Safety is Number One,” isn’t just a saying – it's a fact of life, especially at Renown Health. The safety of all patients, visitors, staff and volunteers is always the top priority, and our Security Department takes that commitment seriously. This team is devoted in their efforts to provide a safe environment for all, building cooperative and proactive security processes leveraging crime prevention techniques and state-of-the-art technology. Renown Security sets the safety and well-being bar high, and they continually exceed that standard day in, day out at all of our hospitals and urgent care, primary care and lab locations. Specially Trained, Continually Present Our Security Department isn’t staffed with your run-of-the-mill Security Officers; these team members surpass security and safety expectations. Think city and state police-level standards. You read that right – many of Renown’s Security Officers come from Nevada Highway Patrol, the Washoe County and Carson City Sheriff’s Offices, the state probation and parole board and more. This team fosters specialized training in a collaborative environment. Every member of the security team has extensive training in compassion, empathy and de-escalation techniques to provide the highest levels of safety and security. They implement this training in all their daily duties, whether they are saying a simple ‘hello’ to a patient passing by or preventing harm to a staff member. Before their shift begins, the team meets to debrief meeting to discuss major incidents that occurred on the previous shift. These meetings ensure the next shift is aware of situations to be on special alert for and individuals to look out for. After, the team members head off to their assignments. “The day could be as mellow as greeting someone at the welcome table, or it could be as chaotic as de-escalating someone in distress,” said Emmanuel Fernandez-Orozco, Supervisor of Security at Renown Regional. “Regardless of the day, every experience is rewarding in its own way. The only thing that is promised is that every day will be different.” While every Security Officer has varying experiences, one aspect of their job always stays the same: they are always on alert for any potential safety issue. Even on the “slowest” days, it is important for this team to stay vigilant in order to mitigate any potential risks. There are several security programs that the team uses to keep everyone at Renown safe and secure: Renown's security operations center team (also known as dispatch) monitors all cameras in real time, with security officers patrolling parking areas 24/7. Security escorts are always available for any employee, patient or guest at every Renown location. Security Officers can escort anyone to their designated site, check surroundings for danger and monitor the person until they safely leave for their next destination. Rescue officers are available for any Renown location where an employee feels unsafe. Security maintains a strong relationship with the Reno Police Department (RPD) and assists with reporting and providing information that aids RPD in pursuing and deterring criminal activity. “In security, we are a counselor, teacher and rule enforcement officer, all rolled into one,” said Bob Stone, Supervisor of Security for Renown Health. Talk about master multitaskers! Protection is only one part of the job. Through positive and meaningful interactions with guests, patients, community and staff, regardless of where they are posted, the Security Department continually helps Renown achieve its mission of making a difference for the people they serve. Devoted Dispatch Speaking of multitasking, no one does this better than the Security Dispatch Center. Security Dispatchers are the “eagle eyes in the sky” at Renown, keeping a close watch on everything that happens within every Renown location, as well as REMSA (including Care Flight). From overlooking the many cameras around campus and administering codes over the PA system to manning the radio and phones to ensure Security Officers are dispatched quickly, our dispatch team helps ensure every safety or security issue at Renown is immediately addressed. When a call comes in, dispatchers like Jessica Fernandez, Security Dispatcher for Renown Health, go through a quick discovery process (sometimes in seconds) to figure out the details of the situation or code and what level of security is needed to assess and de-escalate. According to Jessica, the ability to prioritize is something she values in her work. “80 percent of our duties are on the phone and the radios, and we are skilled in prioritizing concerns based on the sheer volume of calls we get,” she said. Jessica and her teammates are proud of the outcomes from their calls. Their attentiveness to every nook and cranny at Renown and their quick response times to make them not only a valued partner to the Security Department but also a necessity to our health system. Your In-House De-Escalation Experts Being in a hospital environment is undoubtedly stressful for any patient, and many factors can increase these emotions. The Security Department takes these feelings seriously and never hesitates to take appropriate action to ensure the safety of everyone at Renown. With the unfortunate rise of violence against healthcare workers, especially amid the pandemic, our first-rate security team has been crucial in countering violence with specialized de-escalation techniques. The key to de-escalating, according to the Security Department, is to put yourself in the shoes of whoever you are working with. As stated by Bob Stone, the team approaches each situation by asking themselves: How would I want to be treated if I was in the same circumstance? “Being empathetic to their situation and listening to what is going on in their lives is key to re-directing them accordingly,” said Bob. “Applying real-life experience to similar circumstances can make them feel like they are not alone. Educating people on hospital policies can also help them reduce their anxieties and solve the problems.” Jhorddy Lopez, Security Officer at Renown Regional, approaches each situation with the mindset of knowing that each person’s reactions are different. “Different techniques need to be implemented every time,” said Jhorddy. “You have to use your best judgment call.” Quick and effective judgment calls are a task that the Security Department has conquered. Rosie Garcia, Security Officer at Renown Regional, knows that using your best judgment means getting both sides of the story. “Whenever I need to step in and de-escalate a situation, I first speak with whoever is attending to the patient and gather information,” said Rosie. “Then, I always get the patient’s side as well. I want to understand how they’re feeling, so both the staff member and the patient can meet in the middle and come up with a collaborative solution.” An example of the heroism and advanced de-escalation displayed by our Security Officers takes us back to last spring. In the middle of the night, a Care Flight helicopter transporting a patient and their family was about to touch down on the landing pad outside of Renown Regional. Right as the helicopter was about to land, an individual jumped over the safety barricade and onto the landing pad. Alexander Pico, a former Security Officer Lead at Renown Regional (who recently joined the Carson City Sheriff’s Department) immediately communicated with the individual to leave the area. The individual then went under the rear blade, which is the most dangerous part of the helicopter. Knowing that he had to risk his own life at this point to save another, Alexander ran around the back of the helicopter and tackled the individual, preventing catastrophic injury or even death. Steve Perkins now uses this example of a swift judgment call, which was captured on dispatch cameras, as training material for new staff. Exceptional character, compassion and emotional intelligence are the attributes that every member of the Security Department holds. As noted by Steve Perkins, these attributes “allow for a quick assessment of each situation in order to de-escalate and move towards the best possible solution." Securing the Job The Security Department at Renown is actively hiring caring, dedicated team members who are ready to jump in and perform exceptional high-risk healthcare security services for our health system. “We seek people with the right combination of ability and demeanor,” said Steve Perkins. "The training and skills development we provide result in a high caliber of success.” Every team member in the Security Department is passionate about the same thing: helping others. And in a healthcare environment, this is important. “Working a healthcare security job is far different than working any other security job,” said Jhorddy Lopez. “At a hospital, you get the chance to interact with people one-on-one. I get to experience the feeling of, ‘I can make a difference in this person’s life.’” Any interaction can change the course of a person’s day, and the Security Department embraces this fact. “I really do love helping people so much, whether it be an elderly patient who needs help with their wheelchair or a situation where I need to step in and de-escalate,” said Rosie Garcia. In order to succeed in this fast-paced department, being a collaborative team member is crucial. “A good coworker is a team player – someone that loves to work in a team atmosphere,” said Emmanuel Fernandez-Orozco. Jhorddy Lopez reiterates this, adding that “communication and trust are also extremely important. Everyone has to have great communication skills and have each other’s backs.” For people like Bob Stone, having a special connection to Renown inspires him to serve. As someone who experienced two life-saving hospital stays here, he is proud to give back to the organization that gave so much to him. “It was only natural to return to a facility I was familiar with my entire life,” said Bob. “After serving as a paramedic and transporting patients into Renown from Plumas County, I knew I was not done giving back to the community. Renown was the place to do exactly that.” All Genders Welcome A common misconception about the security field is that it is strictly a “man’s job.” In Renown’s Security Department, that couldn’t be further from the truth. As a female Security Officer, Rosie Garcia is a prime example of proving that idea wrong. As a master patroller and de-escalation expert, she ensures everything is running smoothly and that everyone feels safe at all times. “When I first started here, I knew right away that nobody that works here is biased,” said Rosie. “Everyone is equal, and I am treated as an equal in this department. I know I can do the job as well as any man." Both Rosie and her counterparts in the Security Department firmly believe that this line of work is for everyone, and they continually lift each other up and support one another. “No matter your gender, as long as you have confidence and integrity, you will do well,” adds Rosie. The Bottom Line If you are passionate about creating a secure environment to ensure patients get the care they deserve and employees receive the safety they merit, the Security Department is your team to join. “I come into work with pride,” said Jhorddy Lopez. “Knowing that I can change someone’s life – that makes me proud to work here.” “You’re in good hands with us,” closes Steve Perkins.
-
Renown Health Further Expands Visitor Policy to Two Loved Ones
Always listening to the voice of the patient, Renown Health is pleased to welcome any two patient supporters to visit their loved ones during their Renown medical visit, surgery, birthing or hospital stay. Renown continues to have extra safety measures in place to protect the health of patients, visitors and healthcare employees, and as the situation changes with COVID-19, these guidelines are subject to change. Under this updated visitor policy, patients no longer need to identify their supporters ahead of their arrival. Patients may receive more than two visitors per day; however, to help ensure adequate physical distancing, only two guests are asked to visit at a time. All people entering Renown sites must continue bringing and wearing a face mask for their entire visit, including inside patient rooms. Renown’s visitor policy updates were inspired by family members, who requested that the policy be expanded to encourage two family members per day to be able to visit a loved one who was hospitalized at Renown. The request was approved by Dr. Debra Adornetto-Garcia, Chief Nursing Officer and Dr. Paul Sierzenski, Chief Medical Officer, both of Acute Services. With a high percentage of Renown hospital staff now vaccinated against COVID-19, declining hospitalizations of patients with COVID-19, and understanding that the best communication is in-person, as of April 28, 2021, Renown hospitals and medical practices now allow two visitors, instead of one, for all patients and have put extra safety measures in place to protect patients, visitors and healthcare employees. “We are pleased to expand our visitor policy and welcome two healthy adult patient supporters to accompany every patient to their Renown medical visit or hospital stay,” said Tony Slonim, MD, DrPH, President & CEO of Renown. “We are always looking to our patients’ lived experiences to help us address the health needs of our community. Just a few months ago, we were reminded by Darlene Randolph that the best care is ‘person-centered care’, which inspired us to be one of the first healthcare organizations in the nation to expand our visitor policy to all patients, including those with COVID-19. Today, we thank our patients’ family members for voicing the importance of a larger, connected support system to help foster the best healing environment for all patients.” “At Renown, the definition of ‘family’ is defined by the patient,” said Debra Adornetto-Garcia, DNP, RN, NEA-BC, AOCN, Chief Nursing Officer, Acute Services. “Our patients may have anyone they choose as their patient supporters, and these individuals serve as an invaluable extension of our care teams. Patient supporters are asked to partner with the patient’s healthcare team to assist in communicating to other family members and friends, participating in training and education activities and assisting the patient with complying with care and medication instructions.” “Visiting the hospital can be an anxious experience,” said Paul Sierzenski, MD, MSHQS, CPE, FACEP, Chief Medical Officer, Acute Services. “It’s incredible how the company of loved ones can reduce anxiety and promote healing. What we can do together with families to support patient care and excellent outcomes is greater than what any of us can do alone. We are glad to welcome patient supporters to our hospitals to help our patients feel more at ease, so they can focus on their recovery, health and healing.” Two patient supporters per patient are now able to access Renown campuses as noted: Renown Regional Medical Center and Renown South Meadows Medical Center: 8 a.m. to 8 p.m. For Intensive Care Units (ICU): 9 a.m. to 8 p.m. Visitors must be at least 12 years of age or older. Renown Children’s Hospital: Open access. For the Pediatric unit and Pediatric Intensive Care Unit (PICU): Visitors must be at least 12 years of age or older. For the Neonatal Intensive Care Unit (NICU): Visitors must be at least 18 years of age or older. Renown Rehabilitation Hospital: 8 a.m. to 5 p.m. One designated patient supporter is allowed to visit the patient inside their room throughout the duration of their stay. Other loved ones may visit from an exterior window, outside the patient's room. Our care team is also pleased to facilitate bedside virtual visits. In addition to in-person visits, there are many ways to brighten the day of a patient at Renown Hospitals. You can send a personalized message that will be hand-delivered to your loved one, call 775-982-4100 to speak with a patient, or our care team is pleased to facilitate virtual visits via computer or tablet from the bedside. Renown Health reserves the right to limit visitors in the best interests of patients, families, visitors or staff. About Renown Health Renown Health is Nevada’s largest, locally governed, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe and northeast California. With a diverse workforce of more than 6,500 employees, Renown has fostered a longstanding culture of excellence, determination and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network, and the locally owned not-for-profit insurance company, Hometown Health. Renown is currently enrolling participants in a community-based genetic population health study, the Healthy Nevada Project®.
Read More About Renown Health Further Expands Visitor Policy to Two Loved Ones
-
Renown South Meadows Medical Center Earns 'A' For Patient Safety
May 10, 2023 (Reno, NEV.) – Renown South Meadows Medical Center in South Reno has earned an “A” Spring 2023 Hospital Safety Grade from The Leapfrog Group. This national distinction recognizes Renown Health’s achievements in prioritizing patient safety by protecting patients from preventable harm and errors. The Leapfrog Group is an independent, nonprofit, national watchdog organization that upholds the standard of patient safety in hospitals and ambulatory surgery centers. It assigns an “A,” “B,” “C,” “D” or “F” grade to general hospitals across the country. Grades are based on more than 30 national performance measures reflecting errors, accidents, injuries and infections, and systems hospitals have in place to prevent harm. The new grades primarily reflect performance during the height of the pandemic. “We all play a role in protecting the health and safety of our patients,” said Brian Erling, MD, MBA, President and CEO, Renown Health. “As the only locally governed not-for-profit healthcare network in the region, Renown’s success is shared with our patients and community. We celebrate and thank our physicians, nurses, and caregivers for their continued focus on making a genuine difference in the health and well-being of the people and communities we serve.” “At Renown, safety is the number one priority for everyone that comes through our doors,” said Jen Walker, MSN, RN, Vice President, Quality for Acute Services. "The hard-working staff at each facility, who day in and day out provide the best patient-centered care, also demonstrate clinical expertise, service and compassion. This has helped us achieve well-deserved high ratings across the system.” “We work to ensure that the care that our physicians, nurses and caregivers provide is of the highest quality, and safe, effective, people-centered, timely, equitable and efficient,” said Ross Albright, MD, Medical Director of Quality & Patient Safety, and the South Meadows Medical Center Emergency Department. “High-quality health care helps prevent disease and improve the quality of life. That is truly important to everyone on our team, and we are pleased to be nationally recognized for our efforts.” “Every day, we make choices about where we shop, who we bank with, what cars we drive, and what doctors we see. Yet despite our consumer culture, some people aren't aware they can choose what hospital they go to,” said Bret Frey, MD, President of Northern Nevada Emergency Physicians, a 65-physician group at Renown Health. “Your choice of hospital could be a life-or-death decision. Hospitals vary greatly on things like infection rates, surgical errors or patient injuries—and choosing to receive treatment by Board-Certified physicians, ER wait times, patient satisfaction rates, and other measures are important for consumers to know and consider when choosing an ER and a hospital.” “The Leapfrog ratings reflect the staff and system’s commitment to providing the highest quality of care for patients,” said Susan Lee, DO, MBA, Chief Operations Officer, Renown South Meadows. “Earning ‘A’ ratings showcases the commitment both physicians and staff demonstrate every day. We are proud to continue to deliver the best care possible to every patient.” “I applaud the hospital leadership and workforce for their strong commitment to safety and transparency,” says Leah Binder, President and CEO, The Leapfrog Group. “An ‘A’ Safety Grade is a sign that hospitals are continuously evaluating their performance so that they can best protect patients. Your team should be extremely proud of their dedication and achievement.” Developed under the guidance of a national Expert Panel, the Leapfrog Hospital Safety Grade uses publicly available hospital safety data to assign grades to more than 2,700 U.S. acute-care hospitals twice per year. The Hospital Safety Grade’s methodology is peer-reviewed and fully transparent, and the results are free to the public. Renown South Meadows also received a Leapfrog A score in Fall 2021 and Spring 2020. Renown Regional Medical Center received a B score for Spring 2023. For more information on the Leapfrog Group and the Spring 2023 scores, please visit: hospitalsafetyscore.org. About The Leapfrog Group Founded in 2000 by large employers and other purchasers, The Leapfrog Group is a national nonprofit organization driving a movement for giant leaps for patient safety. The flagship Leapfrog Hospital Survey reports hospital performance, empowering purchasers to find the highest-value care and giving consumers the lifesaving information they need to make informed decisions. The Leapfrog Hospital Safety Grade, Leapfrog’s other main initiative, assigns letter grades to hospitals based on their record of patient safety, helping consumers protect themselves and their families from errors, injuries, accidents and infections. About Renown Health Renown Health is the region’s largest, locally governed, not-for-profit integrated healthcare network serving Nevada, Lake Tahoe, and northeast California. With a diverse workforce of more than 7,000 employees, Renown has fostered a longstanding culture of excellence, determination, and innovation. The organization comprises a trauma center, two acute care hospitals, a children’s hospital, a rehabilitation hospital, a medical group and urgent care network, and the region’s largest, locally owned not-for-profit insurance company, Hometown Health.
Read More About Renown South Meadows Medical Center Earns 'A' For Patient Safety