Search
-
Ask the Expert: What is Scoliosis?
Posture is important, but for those children diagnosed with scoliosis (spinal curvature) it can be a difficult issue. The Washoe County School District Student Health Services Department screens 7th grade students for scoliosis as growth spurts often reveal the condition and, if diagnosed early, scoliosis can stop progressing. We asked Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis to answer some frequently asked questions about scoliosis. What is scoliosis? There are many types of scoliosis: early onset (occurs before age 10), congenital scoliosis is when the bones of the spine do not form correctly, neuromuscular scoliosis which is due to children’s neurologic and muscle disease, and the most common is Adolescent Idiopathic Scoliosis. The term “idiopathic “ means the exact cause is unknown, although we do know it runs in families. This type of scoliosis occurs in 2-3 percent of adolescents and is mainly seen during their growth spurt. This is why middle school screenings are recommended. Both genders get scoliosis but girls are 8 times more likely to have their curves progress and become larger. What are the signs that my child may have scoliosis? A few signs for parents to watch for are: One shoulder might be higher than the other. One leg may seem longer. A hip may be higher or look more prominent. The waist may not look the same from side to side (asymmetry). The trunk or rib cage may be more prominent on one side or shifted. When they bend forward they may have a bump on their back. How is scoliosis diagnosed? It can be noticed by a pediatrician at a physical, school screening nurse, PE teacher or parents. Once the curve is suspected the child is usually referred to a pediatric orthopedic surgeon scoliosis expertise. At the initial visit the doctor will perform a thorough physical including a complete neurologic exam to assess the amount of curvature. Once the exam is completed the physician will determine if a spinal x-ray is needed. The curve on the x-ray is measured utilizing the cobb angle (a measurement in degrees) which helps guide the treatment. What are common treatments for scoliosis? The treatment depends on the size of the spinal curve and the amount of growth the child has remaining. An x-ray of the child’s hand is used to determine the amount of growth remaining. This allows the determination of the child’s bone age, and based on the hands growth plates it can determined if the child is in their rapid phase of growth. Treatments include: Observation - For curves less than 20-25 degrees. This entails visits every 6-9 months with a repeat scoliosis x-ray. Since scoliosis curves increase only 1-2 degrees per month, and variations in measurements can be 3-5 degrees, an x-ray is not recommended before 6 months. If the curve remains less than 25 degrees the child is followed until their growth is completed (usually age 16-18). Progressing Curve - If growth is finished and the curve is less than 40 degrees, the risk of more curvature into adulthood is small. If growth is completed and the curve is over 45 degrees, the child is followed for several years as these curves can progress into adulthood. If the patient is still growing and the curve has progressed greater than 25 degrees but still in the non-operative range (less than 45-50 degrees) bracing is used to stop the progression of the curve. Bracing - Indicated for curves over 25 degrees but less than 45 degrees. If a brace is required you will be referred to an orthotist (bracing specialist). The orthotist assesses your child, reviews the x-ray and then fits the brace. (Having a brace made usually takes 2-3 weeks.) Once the brace is fit, your child will visit the scoliosis specialist for an x-ray in the brace to ensure it fits correctly. The primary goal of bracing is to halt progression of the curve and prevent the need for surgery. The brace must be worn for about 16 hours per day to be effective. In a recent bracing study 72% of the patients who wore their braces as prescribed prevented the need for surgery compared to the group who did not wear their brace. Surgery: When a curve reaches 45-50 degrees, and a child is still growing, surgery is usually recommended because the curve is likely to continue progress. If a curve is over 50 degrees and the child is done growing surgery also may be recommended. This is because when curves are over 50 degrees they tend to increase 1-2 degrees per year for the rest of your life. As curves get larger the amount of lung function tends to decrease which could cause breathing problems later in life. The goals of surgery are to stop the progression of the curve and safely correct any misalignment. This is accomplished by attaching implants (rods, screws, hooks and bands) to the spine. Bone graft is then placed around the implants to encourage the spine to fuse (grow together). This then forms a solid column of bone with metal rods in place, preventing the curve from changing. Most patients are back to their regular sports and activities six months post surgery.
-
How to Safely Store Breast Milk
Breast milk. It's often referred to as liquid gold. And fortunately, it can be safely refrigerated or frozen for later use, which can allow you to be a bit more flexible in your new routine with baby. Whether you're getting ready to return to work, planning for the chance date night out or just exclusively pumping, it's crucial to understand the guidelines for proper breast milk storage. Storing Breast Milk Use clean bottles with screw caps, hard plastic cups that have tight caps or nursing bags (pre-sterilized bags meant for breast milk). Be sure to label each container with the date the milk was pumped and your baby's name if the milk is going to childcare providers. You can add fresh, cooled milk to milk that is already frozen, but add no more than is already in the container. For example, if you have two ounces of frozen milk, then you can add up to two more ounces of cooled milk. For healthy full-term infants, milk can be stored as follows: Room temperature - six to eight hours (no warmer than 77°F, or 25°C). Refrigerator - up to five days at 32°-39°F (0°-3.9°C). Freezer– Varies depending on freezer type. Up to two weeks in a freezer compartment located within the refrigerator. Three to six months in a freezer that is self-contained (standard kitchen fridge/freezer combination) and kept at 0°F (-18°C). Breast milk should be stored in the back of the freezer and not in the door. Six to 12 months in a deep freezer that is kept at -4°F (-20°C). Be sure to leave about an inch of space at the top of the container or bottle to allow for expansion of the milk when it freezes. Thawing Breast Milk Place frozen breast milk in the refrigerator to thaw (about 24 hours) then warm by running warm water over the bag or bottle of milk and use it within the next 24 hours. If you need it immediately, remove it from the freezer and run warm water over it until it's at room temperature. Never microwave breast milk and do not refreeze it. Once your baby has started to drink from the bottle, you should use it within one hour. You may find that different resources provide different recommendations about the amount of time you can store breast milk at room temperature, in the refrigerator and in the freezer. Talk to your doctor or lactation consultant if you have any concerns or questions.
-
Emergency Care During a Pandemic
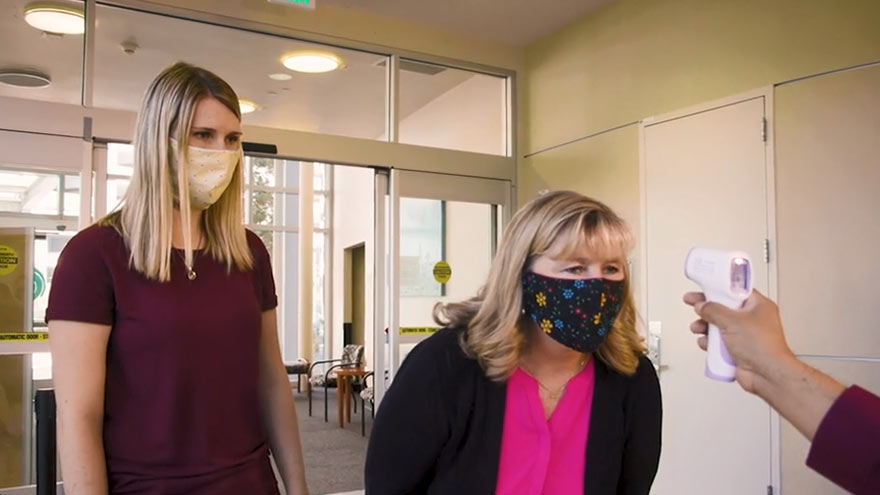
Medical emergencies like strokes and heart attacks still happen, even in a pandemic. That’s why Renown Health is always ready to provide emergency care to patients in need, and being admitted at Renown does not put patients at risk of getting COVID-19. When to Get Emergency Care Resources like Renown Virtual Visits have allowed us to stay home while making routine visits with our primary care physician. But, if you are feeling any of the following symptoms, please call 911 or have someone you know take you to the emergency room. Symptoms that may require emergency care: Heart attack Stroke symptoms Difficulty breathing Chest pain Seizure Sudden loss of consciousness Severe abdominal pain Serious allergic reaction Fighting the Good Fight for Our Patients Renown Health provides a clean and safe environment 365 days of the year, 24 hours a day. Alongside regular sanitation practices, Renown is dedicated to protecting patients from infectious disease while providing emergency care. Staff, Care Providers and Visitors Wear Masks Every staff member, care provider and visitor is wearing a mask. Additionally, providers are following guidelines from the Centers for Disease Control (CDC) on wearing protective equipment, such as masks and gloves. Respiratory Illness Screenings for Everyone Care providers and staff members are participating in respiratory illness screenings. Therefore, any care provider or staff member with a fever, cough, difficulty breathing or severe respiratory illness is not on a Renown campus. Visitor Restrictions are in Place Visitor restrictions are in place to prevent the spread of infectious disease by practicing physical distance. Because of these restrictions, Renown is only allowing one visitor per patient for with extenuating circumstances. Staying healthy and safe means caring for yourself in emergency situations, too. Please do not hesitate to call 911 when you or a loved one are in need of emergency medical care. Virtually Visit a Renown Urgent Care Login to MyChart to “get in line” for a virtual urgent care visit between 8:30 a.m. to 10:30 p.m. Monday-Friday and 9:30 a.m. to 4:30 p.m. Saturday and Sunday. Login to MyChart
-
Making Patient Safety the Priority It Deserves to Be
I am regularly amazed by medical advancements and innovation in the United States. However, even as we make significant progress in many areas of medicine, there is still much more work to be done in others. One such area is patient safety. What is Patient Safety? When we talk about patient safety, we are discussing how hospitals and healthcare organizations protect patients from errors, injuries and infections. Anyone can make a mistake at work, but in healthcare these mistakes can result in serious outcomes. In 1999, the Institute of Medicine released a report that estimated 98,000 deaths per year result from medical examination or treatment. The most recent study in 2013 suggested these numbers could range from 210,000 to 440,000 deaths per year. Many of these deaths result from preventable medical errors. This is inexcusable and shows how much more work our industry still needs to do to improve patient safety. Making Patient Safety a Priority Patient Safety is our number one priority at Renown Health. We dedicate a lot of time to establishing, reviewing, and revising our processes to prevent errors. Despite the obvious importance of patient safety, this issue is largely left to individual hospitals and health systems to manage. There is a surprising lack of national attention around this truly important issue. However, a silver lining of the COVID-19 pandemic is that it is igniting interest in hygiene and infection prevention. Patients want to learn more about the processes that are in place to prevent the spread of infections. In addition to the many protocols that guide our treatment of injuries and illness, Renown Health has implemented the following measures to prevent the spread of communicable diseases: Requiring everyone entering Renown sites to wear a mask or face covering. Establishing new processes to help patients and visitors practice social distancing. Limiting the number of visitors in our facilities. Screening all employees and patients for symptoms. Enhancing our already-thorough cleaning and disinfection processes. I hope patient safety and infection prevention remain in the national spotlight long after the COVID-19 pandemic has ended. The healthcare industry must come together to develop stronger systems and regulations to minimize preventable medical errors. We have a responsibility to our patients to do better.
Read More About Making Patient Safety the Priority It Deserves to Be
-
Bringing a Public Health Perspective to Healthcare
There are many lenses through which to view health. As you would expect, medical providers typically focus on the health of individual patients. For example, doctors consider a person’s symptoms, their current lifestyle, their past medical history, and their family’s history to diagnose medical conditions and recommend treatments. The Public Health Perspective Public health professionals look beyond the health of an individual and instead focus on the health of an entire community or population of people. They strive to achieve “the greatest good for the greatest number.” As the CEO of a health system, I feel fortunate to have education and training in both medicine and public health. As Renown Health’s leader, it is my responsibility to care for the people and communities we serve. That involves bringing world-class staff and innovative medical care to northern Nevada. We also focus on prevention by looking for ways to improve health outside of our facilities. That means partnering with local organizations to address the social, economic, and environmental factors that shape our health. Or working with local government to create policies that help to prevent disease and injury. In order to make a genuine and long-lasting impact on health, we must foster a community that helps our neighbors live well. Public health is especially important during times of crisis, such as the COVID-19 pandemic that we’re experiencing now. During these times, health systems must be able to swiftly shift focus from prioritizing the needs of individual patients to considering what is best for our local population. For example, we may need to temporarily limit hospital visitors or educate the public about how to socially distance in order to stop the spread of disease. Being prepared to make this shift and having strong relationships with our local health department and community organizations help us better serve the public. In both good times and bad, I am thankful that my public health background provides me with the perspective to look beyond our health system and embrace the health our community.
Read More About Bringing a Public Health Perspective to Healthcare
-
How You Can be a COVID-19 Vaccine Ambassador
We get it – the entire world has been overwhelmed with COVID-19 vaccine information, questions and celebrations around vaccines developed to combat COVID-19 induring the past several months. It’s hard to know where to start in digesting all this news and information. But one thing is clear: healthcare experts agree that the authorized COVID-19 vaccines are safe, effective and recommended to help end this pandemic. If you are passionate about stepping up in your community to encourage the vaccination efforts, we’re offering a few ideas on how you can be an ambassador. Find the Facts Content on the vaccine is abundant, but and there’s a few resources that we can all rely on to help digest the information: The Centers for Disease Control (CDC) updates its website content around the vaccine regularly, and also offerings information in Spanish. Health departments across the U.S. are leading the way in distribution logistics planning, and partnering with other providers, like such as hospitals and pharmacies, to distribute give people doses. Their websites are great resources to understand options where you live. Locally, check out washoecounty.gov/health/programs-and-services/environmental-health/covid-19-guidance for vaccine updates in Washoe County. Many providers like Renown Health and other providers are sharing content around their recommendations for the vaccine. Get answers about the vaccine types from one of our pharmacists, read common concerns addressed by experts and view videos from many doctors and other specialists on our YouTube Channel.
Read More About How You Can be a COVID-19 Vaccine Ambassador
-
4 Breastfeeding Tips for New Moms
While breastfeeding is natural, it's not always easy. We asked Certified Lactation Counselor Sarah Mitchell for some tips to help make the process easier for mom and baby. From increased infant immunity to improved maternal health and well-being, the benefits of breastfeeding are many. Still, only 60 percent of U.S. moms in the United States continue to breastfeed past their baby's first six months. There are for many reasons for why moms stop, including the mother's their need to return to work. We reached out spoke to Sarah Mitchell, a certified lactation counselor at The Lactation Connection at Renown, for some expert advice. Tip 1 At first, it's normal to expect obstacles. Even in cultures where close to 100 percent of moms breastfeed, they can experience issues, including getting the baby to "latch on," sore nipples, and milk production. In addition, it sometimes can take several weeks for mom and baby to get comfortable. Tip 2 Line up a coach, even before the baby is born. This can be a professional lactation coach, family member, or friend who is experienced and encouraging. While online videos can be helpful, most new moms need the one-on-one guidance that a coach can provide. Renown offers outstanding resources in its Lactation Connection center, including expert consultants, products, and support. Tip 3 Well ahead of the due date, set up a support network of friends, family members, or community groups such as La Leche League. Women historically have relied on extended support systems to help them with raising children, and breastfeeding is one of those areas that, while natural, still needs encouragement from the women who’ve been there. Tip 4 Don’t get discouraged if you need to supplement at times with formula. This, too, as it turns out, is not uncommon in other cultures. In other parts of the world, babies are given beverages and foods such as tea, broth, soup, juice, mashed bananas, and papaya. The American Academy of Pediatrics recommends supplementation only with approved formula -- but the point is, it’s ok to supplement if you need to. Finally, don’t forget the importance of breastfeeding for connecting with your baby. It’s essential to maintain breastfeeding over the weekends, preferably “on-demand,.” and will keep that special bond strong after you have returned to your job.
-
Breast Feeding Doesn't Have To Mean Sore Nipples
If you think sore nipples are just a normal part of breastfeeding, think again. Robin Hollen, APRN, and Breastfeeding Medicine Specialist, says that nursing can be an enjoyable experience for mom and baby without pain and discomfort. A top concern of nursing moms within the first week after delivery is how to prevent sore nipples. Even moms who’ve nursed before struggle with this common issue. While many women think it is a regular part of the nursing experience, it is actually a sign that something isn’t quite right. “Nursing your baby should be enjoyable,” says Robin Hollen, Breastfeeding Medicine Specialist with Renown Health. For over 30 years Robin has been supporting moms to breastfeed. Below she shares some valuable information and tips, helping you create a happy and healthy breastfeeding experience for you and your baby. What causes sore nipples? The most common cause of sore nipples involves incorrect latching. For a proper latch, a baby’s mouth takes in the entire nipple and some of the breast, so that the nipple rests at the back of the mouth where the palate is soft. With an improper latch, the mouth may slip down to the tip of the nipple while the baby nurses. This constant pressure on your sensitive skin may cause discomfort and pain. A board-certified lactation consultant can help assess if your baby is latched correctly and troubleshoot your breastfeeding concerns. Less common causes of sore nipples include: • Improper tongue placement of baby • Clenching • Incorrect breast pump use How can a mother prevent sore nipples from an improper latch? Breastfeeding is a learning experience for both mom and baby. Ask for help with the latch so your baby learns it correctly and maintains its depth. In the past, new mothers were surrounded by a community of women — their own mothers, grandmothers, or other family and friends — to provide assistance and guidance with every latch at the beginning of an infant’s life. In today’s culture, new moms can find themselves on their own with no extended family to lend their knowledge. Nurses, pediatricians and lactation consultants now fill that role; they are the eyes and hands along with the much-needed experience to guide new mothers. Our Breastfeeding Medicine experts assist nursing moms with latch every day. Even a single visit with a lactation consultant observing your breastfeeding baby can provide valuable insight on achieving, and maintaining, the proper latch - preventing future nipple soreness and discomfort. How to heal sore nipples from breastfeeding To heal sore nipples, you must first fix the cause, and correcting the latch prevents further damage. A lactation consultant can also help you address the pain. Below are some breast healing tips: • Your own expressed breast milk is excellent to rub into the nipple for anti-bacterial protection. • For those moms who need more lubricant or fat than breast milk offers, use a lanolin or a cream that is labeled safe for the baby. • Soothies are a gel pads providing comfort in between feedings, but should not be used with lanolin products. • Breast shells, not to be confused with shields, can guard the nipples from irritation or pressure in between feedings. If you have more questions about preventing and healing sore nipples or general breastfeeding concerns, talk to your pediatrician or a Renown Health Breastfeeding Medicine specialist at 775-982-6365.
Read More About Breast Feeding Doesn't Have To Mean Sore Nipples
-
COVID-19 Booster Shots, What You Need to Know
Getting the COVID-19 booster is the best way to protect yourself from severe illness or death due to COVID-19, and both the CDC and the FDA have approved booster shots for people ages 18 and older. So, with the holidays right around the corner and infection rates on the rise both in Nevada and nationally, the best thing you can do to prevent the continued spread of this deadly virus is to get boosted today. The Basics: Who: It is recommended that everyone 18 years or older get a COVID-19 booster shot. When: At least 6 months after completing your primary COVID-19 vaccination series. What: Any of the COVID-19 vaccines authorized in the United States. The CDC allows for mix and match dosing for booster shots. How: To make an appointment for your COVID-19 vaccine booster, please visit vaccines.gov today. Appointment Reminders: Don’t forget to bring your CDC vaccination record card to your appointment. Refresh yourself on the potential side effects and remember that these are normal signs your body is building up protection. Commonly Asked Questions: Q: Does anything change if I received the Johnson & Johnson as my first COVID-19 vaccine? A: If you received the Johnson & Johnson COVID-19 vaccine, you are elidable for a booster two months after completing your primary vaccine. Q: Is the formula the same for the boosters as it was for the primary vaccine? A: COVID-19 booster shots are the same formulation as the current COVID-19 vaccines. However, in the case of the Moderna COVID-19 vaccine booster shot, it is half the dose of the vaccine people get for their primary series. Q: Am I still considered “fully vaccinated” if I don’t receive a COVID-19 booster shot. A: Yes, everyone is still considered fully vaccinated two weeks after their second dose in a two-shot series, such as the Pfizer-BioNTech or Moderna vaccines, or two weeks after a single-dose vaccine, such as the J&J/Janssen vaccine. All information courtesy of the Center for Disease Control and Prevention. All information courtesy of the Center for Disease Control and Prevention
Read More About COVID-19 Booster Shots, What You Need to Know
-
How to Ease Your Child's Fear of Vaccines
Getting a shot can be scary for kids and anxiety-inducing for parents and caregivers. With flu shot season well underway and children's COVID-19 vaccine clinics in full swing, we wanted to share ways to reduce the stress for you and your child. Plan Ahead and Be Honest A few days before the scheduled appointment, casually mention to your child that you’re both going to the doctor’s office (or vaccine clinic, or pharmacy) soon for their vaccine. Explain to them that this will help protect them and will only take a second. Being honest is important, telling your child that it will hurt for a moment. If possible, try and schedule the vaccine at a kid-specific vaccine clinic, your pediatrician's office or a school-based site. Remember that words are powerful. Take notice if you are using a word that might make them more upset, such as prick, jab, needle or shot. You can interchange words such as vaccine, immunization or injection. Bring Toys Don’t be afraid to let your child bring one of their favorite toys or stuffed animals to the appointment. This can make them feel more comfortable and provide distraction. Ask for Pain Reliever/Numbing Agent If you know from past experience (or suspect) that your child has a needle phobia, talk to the vaccination location ahead of time and ask if they can use a pain reliever or numbing agent before administering the vaccine. Distract. Distract. Distract. Sing a song, tell them a joke, make a funny face. If you can pull your child’s attention away from the needle and make them laugh, they won’t focus all their energy on worrying about the shot. Lead By Example If you haven't gotten your flu shot, COVID shot or COVID-19 booster yet, ask the facility ahead of time if you can also get a shot before your child. Show them that the shot is no big deal and that they will have no problem getting it themselves. Celebrate Don’t be afraid to celebrate this victory with your child once it is over – bring them to the park, go out for an ice cream cone, let them pick what’s for dinner. This reward will show that you’re proud of them for being brave and may also make the next time your child is due for a shot easier.