Search
-
Use Caution: Mixing Over-the-Counter Medications Can Be Harmful
With allergy season’s extended stay and cold and flu season having just begun, you may soon find yourself seeking relief through several different kinds of over-the-counter medications. Know what precautions you need to take when fighting multiple symptoms with multiple medications. When you’re too sick to go to work but not sick enough for a doctor’s visit, over-the-counter medicines are a welcome relief to help alleviate that fever, runny nose or allergies. But because those medicines aren’t signed off on or managed by your doctor and pharmacist, it’s crucial that you’re especially mindful of what you put into your body. Whenever you pop a pill, you want to make sure you’re taking the right dosage, waiting the right amount of time before taking another dose and not mixing certain medicines together. Recent stories like this one detail dangerous over-the-counter medicine combinations, and we’re following suit: Here is a quick go-to guide about potentially harmful over-the-counter combinations. Too Much Tylenol/Acetaminophen Tylenol — or acetaminophen — is a popular pain reliever for many, but too much can be bad for your liver. “Our bodies have a finite ability to metabolize Tylenol,” says Andy Wright, clinical pharmacist at Renown Rehabilitation Hospital. “When too much builds up in the liver, it becomes toxic. In patients with medical conditions like cirrhosis of the liver or hepatitis, this could be disastrous.” Remember, acetaminophen is in more than just Tylenol and generic pain relievers. You may also see acetaminophen in flu, cold and cough medicines, like Nyquil, and some prescription medications including Norco and Percocet. Keep a list of the medications you take, and limit daily acetaminophen use to 3,000 mg per day. When you’re scanning medicine bottle contents, remember acetaminophen is also referred to as APAP, AC, acetam or paracetamol. Mixing Painkillers When you’re dealing with pain and not getting any relief, taking a different medication may seem like the easy solution. Maybe you take some Aleve — a form of naproxen — for a headache, but it isn’t working, so you switch to Motrin, an over-the-counter form of ibuprofen. Not a smart idea. Ibuprofen and naproxen along with aspirin are known as nonsteroidal anti-inflammatory drugs (NSAIDS). Because these medicines work in similar ways, they should never be combined or used in larger doses or more frequently than directed. Otherwise your risk of side effects can increase, which range from mild nausea to severe gastrointestinal bleeding. It’s also important to consider your family history when taking NSAIDs because, “recent studies have shown NSAIDs may have greater cardiovascular risks for people taking blood thinners or those with hypertension,” explains Andy. “A good example is ibuprofen: It has a relatively low gastrointestinal bleed risk while it has a moderate to high cardiovascular risk. The opposite is true for naproxen.” Rather than experimenting with multiple medicines, figure out which drug works best for you. You may find muscle soreness improves with aspirin, whereas when a headache hits, naproxen is best. Keep in mind that these medications aren’t always best for everyone in the family. “Aspirin in children and teens is not recommended unless under the supervision of a doctor,” Andy says. And pregnant and lactating women should generally avoid NSAIDS due to risk of birth defects and bleeding. “In both of these cases, acetaminophen or Tylenol are preferred but only if approved by an OB/GYN.” Fighting Allergies Over-the-counter antihistamines like Claritin, Zyrtec and Allegra have made fighting itchy eyes and runny noses a little easier. But these daily medicines — when taken inappropriately or in the wrong combinations — can also have an adverse effect. Similar to acetaminophen, you need to watch for antihistamines in other products. Sleep aids — like Tylenol PM and Unisom — commonly use an antihistamine known as diphenhydramine, which may increase your risk of overdose. “Combining antihistamines, or overdosing, can cause many adverse effects including dry mouth, blurred vision — even arrhythmias,” Andy says. “Only take these medications on their own.” If you’re still struggling with symptoms, you can talk to your doctor about adding an over-the-counter nasal steroid. Andy confirms the importance of closely following the directions listed on antihistamine (and all medicine) bottles. He has seen extended release nasal decongestants cause significant arrhythmias requiring medical care after a patient took the medicine with warm fluids. “The decongestant in question is designed to slowly release, but it can dissolve suddenly in the presence of warm liquids like coffee,” Andy explains. “This can cause the pill to deliver 12 to 24 hours of medication all at once.” Taking an Antidiarrheal with Calcium Calcium supplements and antidiarrheal medicines are another harmful combination. Calcium firms up your stool, but if taken with an antidiarrheal, can cause severe constipation. If you need to take an antidiarrheal, take a break from your calcium for a few days until you’re back to normal. Another consideration when taking calcium supplements or calcium-based antacids is gas. “I’ve had several patients report cases of excessive gas using Tums or calcium carbonate-based supplements.” Andy suggests instead “trying Maalox or Mylanta for indigestion and Citracal as a supplement.” Talk with Your Doctor or Pharmacist About Your Medications If over-the-counter drugs aren’t providing the relief you need, it’s time to see your doctor. And remember, for your safety it is important to keep your doctor and pharmacist up-to-date with any medications — prescribed or over-the-counter — that you are taking.
Read More About Use Caution: Mixing Over-the-Counter Medications Can Be Harmful
-
Perseverance and Physical Therapy Help UNR Student Walk Again
University of Nevada, Reno student Khoa Le was paralyzed in 2010 after a longboarding accident. Through physical therapy, a positive attitude and sheer will, Le is walking again. This weekend, Le will walk across the commencement stage to accept his college diploma. “Walking around on my own power is just the greatest feeling,” says Khoa Le, a senior at the University of Nevada, Reno. Just after finishing summer school at the university in July 2010, his whole life changed within seconds after stepping on a longboard skateboard for the first time. He lost control of the board and hit the curb, causing paralysis on the left side of his body. His journey to recovery began at Renown Health Physical Therapy & Rehab. His physical therapist, Dina Barry, says he never complained once in four years. “I started seeing Khoa in April 2011, and we worked for four years together,” says Barry, a lead physical therapist at Renown. “Everything I’ve ever asked him to do, he does. Le is a hard worker, is continuously optimistic and smiling, and I think that is why he’s accomplished what he has.” Le plans to pursue a career as an information systems manager.
Read More About Perseverance and Physical Therapy Help UNR Student Walk Again
-
Name-Brand Medication vs. Generic: What's the Difference?
Most prescriptions meds are available in generic form. Find out the similarities and differences between the two and how to determine whether a generic is right for you. Approximately 80 percent of prescriptions sold today are generics. If you’re taking a prescription medication, chances are it’s a generic form of the brand-name drug. But are you getting the same quality in a generic medication? Do generics measure up? The answer in most cases is yes — generics, just like branded products, are regulated by the Food and Drug Administration. “To have a generic product approved by the FDA, the generic manufacturer must prove that its product is bioequivalent to the branded product,” explains Adam Porath, PharmD, BCPS AQ-Cardiology, BCACP and Vice President of Pharmacy Services. Basically, it has to function the same. “Generic products are extremely well tolerated and will provide the same results as using a branded product,” Porath says. Here’s how generics are the same as name-brand prescriptions: Generic products contain the same active ingredients. They produce the same desired clinical effect and accompanying side effects. Generics come in the same form as their branded counterparts: pill, liquid or inhaler, for example. Release into the bloodstream matches the name brand in timing and strength. Here’s how they differ: Generics generally cost less. Federal law requires generics have different names and look different: shape, size, markings and color. Generics contain different inactive ingredients, like binders, fillers and artificial colors. Different side effects with generics can usually be attributed to these additions. Why do generics cost less? When pharmaceutical companies develop a new drug, they are paying for research, development, clinical studies, marketing — in some cases it can cost more than $800 million and take 10 to 15 years to develop a new drug. “The manufacturers of branded medication products have to recoup their research and development costs,” Porath says. So companies are granted a limited patent to sell their drug without the competition of generic counterparts. “When patent exclusivity ends, the market is open for any generic manufacturer to make a competing product with FDA approval.” Without the same startup costs, companies can sell generics at 80 to 85 percent less. And because more than one company can produce the same generics, competition drives prices even lower.
Read More About Name-Brand Medication vs. Generic: What's the Difference?
-
The Healthy Nevada Project Changed My Life: A Local Mom's Story
Read about Jordan Stiteler, a local mom who says the Healthy Nevada Project provided insights into her family’s genetic makeup — and the likely cause of her dad and great grandfather’s deaths. Now she is changing her life due to her new diagnosis of familial hypercholesterolemia, which will allow her to take steps toward preventing the same fate. Jordan Stiteler’s dad died suddenly of a stroke nearly ten years ago — at only 45 years old. His grandfather died at age 40. Now through the Healthy Nevada Project’s no-cost genetic testing, she is closer to understanding why that may have happened. And she can take proactive steps to prevent the unhealthy symptoms that often lead to a stroke and heart problems. After getting her Geno 2.0 by National Geographic ancestry report, Stiteler got a call from Renown Institute for Heart & Vascular Health Cardiologist and Renown IHI Director of Research, Dr. Christopher Rowan. “They told me that I have FH, which is familial hypercholesterolemia,” she said. “I have genetically very high cholesterol because I have a non-functioning gene that doesn’t get rid of my cholesterol like a normal body would.” Familial Hypercholesterolemia: Simple Life Changes Dr. Rowan told Stiteler it is curable with medication and a change in lifestyle. Stiteler has embraced healthy lifestyle changes by exercising more and eating healthier. “It is so important. Being a mom, I think you have so much more to live for. Having this information has changed my life.” Stiteler feels confident FH affected her Dad. “It is helping my family realize that we need to get tested,” she said. “There were big milestones that my Dad missed. He didn’t get to see either of us get married or have our children. That was huge.” She has become passionate about sharing the need to join the Healthy Nevada Project as her way of helping to prevent other families from possibly going through what she and her family did with the early loss of her Dad. In addition to FH results, the Healthy Nevada Project is returning clinical results on BRCA 1/2 (hereditary breast and ovarian cancer) and Lynch syndrome (colorectal and endometrial cancer) to consenting study participants. To sign up for the Healthy Nevada Project, go to HealthyNV.org. Join the Healthy Nevada Project Recruitment for phase two is still open. In addition to opting in to receive clinical results, participants receive National Geographic’s Geno 2.0 ancestry app at no cost. They also have the chance to pick an additional app for health and wellness after completing a follow-up survey. Learn More or Sign Up
Read More About The Healthy Nevada Project Changed My Life: A Local Mom's Story
-
Cancer Support FAQs: How to Help When It's Someone You Love
Every cancer journey is different — and so are the ways individuals deal with a cancer diagnosis. So if you’re a close friend or family member, how can you help? Bobbi Gillis, manager of cancer support services with Renown Institute for Cancer, explains more. Just as we are all unique, we all also have our own ways of dealing with difficult news. For some, receiving a cancer diagnosis is devastating, and they want family members rallying around them in support; for others, they want to be left completely alone. So how do you know what is helpful and what is hurtful? For advice, we reached out to Bobbi Gillis, manager of cancer support services with Renown Institute for Cancer. Support, Defined What are some ways to support a loved one when they find out they have cancer? First and foremost, let them know you are there for them. As we can all imagine, a cancer diagnosis is scary, and it’s helpful just to know you have support if and when you need it. Second, try to listen and give advice only when you are asked. In trying to help as much as possible, many family and friends take on the role of “researcher” to find out more treatment options, but it’s best to avoid saying “you should try this” or “you ought to do that.” Patients are already dealing with a lot of information at once from care providers and their own research. You don’t want to make them feel overwhelmed or question the treatment they’re planning. What are some words of encouragement or support people can use? Just as you would in any difficult situation, speak from the heart and be genuine. But also be careful not to show false optimism or to tell them to just stay positive; saying these things may discount their fears and concerns. Here are some ideas to get you started: “We’re going to get through this together.” “Count me in to help out.” “I’m not sure what to say, but I want you to know I care and I’m here.” What resources are available to patients? What about their families? For patients with cancer, we offer support groups in-person or online. There are also support groups specific to the type of cancer you or your loved one have. You can check these out on our website, renown.org, or ask your care provider. There are also support groups and emotional support services available for family and friends. How can family and friends help throughout cancer treatment? It’s great to offer help, but it’s important to be specific when you offer. Saying “call me if you need something” is very general, and people may feel like they’re putting you out when they do ask for something specific. Instead, offer help with certain tasks — like driving them to treatment, babysitting, making them dinner or buying groceries. As much as possible, keep things normal. For some patients, being able to do everyday things like walking the dog helps them feel better. Loved ones can try to do too much for a patient, and while well-intentioned, this can make them feel less useful after being diagnosed. Renown Institute for Cancer | 775-982-4000 At the Renown Health Institute for Cancer, our experienced team provides the support and care to maintain the highest quality of life and then achieve the best possible outcome, all in one location that’s close to home. Our dedicated team, clinical expertise and advanced treatment options allow us to tailor care to each patient. Learn about: Our Team Cancers We Treat Screening and Prevention Treatment Options Find a Doctor
Read More About Cancer Support FAQs: How to Help When It's Someone You Love
-
Is Bariatric Surgery Right for You?
You’ve likely heard about bariatric surgery — and perhaps even have friends who’ve done it. But is it a potential solution for you? Here, Dawn Remme, RN, Metabolic Bariatric Surgery Program Manager, provides insight. You may have been struggling with excess weight for years. You’ve tried high-protein diets, low-carb diets and more. Most patients considering weight loss surgery have tried numerous dieting methods. The truth is, some patients who suffer with obesity are successful dieters. Unfortunately though, excess weigh often returns. This impacts their health and the quality of their life. It can be a disheartening battle. Weight loss surgery is a big decision. In making this decision, keep in mind that surgery is only one step toward your goal of achieving better health. It is neither magic, nor is it the “easy way out.” Weight loss surgery can offer you a TOOL to help you become more successful in controlling the disease of morbid obesity. By combining this tool with a lifelong commitment to important lifestyle changes, medical follow-up and nutritional modifications, you have the potential to become a healthier you. Bariatric Surgery By the Numbers Exploring the facts about obesity, how it impacts your health, and how surgery can resolve or significantly improve your chronic medical conditions is the first step to making a decision. Obesity is medically defined as “excess body fat” and is measured by a mathematical ratio known as the Body Mass Index (BMI). To calculate your BMI, we consider your height, weight, age, gender and body build. Here are the standards: “Normal” BMI: less than 25 Overweight: 25 – 29.9 Obese: BMI of 30 – 39.9 Morbid obesity: BMI of 40 or more Morbid obesity (BMI over 40) is a lifelong, progressive disease, and the prevalence of morbidly obese Americans (100 or more pounds over a healthy weight) is increasing rapidly. According to the CDC, the disease of obesity affects 78 million Americans. Further estimates indicate about 24 million have morbid obesity. Serious medical problems known as co-morbidities often occur when someone is morbidly obese. Studies tell us conditions such as type 2 diabetes, high cholesterol, sleep apnea, high blood pressure and degenerative arthritis increase in severity as the BMI is increasing in patients. When may weight loss surgery be an option? When someone has a BMI greater then 40. If a person’s BMI is 35 – 39.9 and they have significant health problems such as type 2 diabetes, high blood pressure, high cholesterol, sleep apnea, or other diagnosed health conditions related to obesity. Gastric Sleeve, Gastric Bypass Explained To resolve or significantly reduce these health conditions, bariatric surgery can be done when diet and exercise haven’t worked. Weight loss surgery makes changes to your digestive system to help you lose weight. The gastric sleeve limits how much you can eat, whereas gastric bypass limits how much you can eat and reduces the absorption of certain nutrients. Other Benefits of Surgery You can greatly increase life expectancy by resolving or significantly improving conditions like diabetes, high cholesterol, high blood pressure, sleep apnea, and obesity itself. Infertility can also be positively affected. A significant weight loss and relief from serious health conditions and diseases will greatly improve your quality of life. Studies tell us that type 2 diabetes is resolved or significantly improved in 84 percent of patients following bariatric surgery. Cholesterol levels dropped in 95 percent of patients. And hypertension and sleep apnea showed improvement in 68 and 80 percent of patients, respectively, following bariatric surgery. Bariatric Surgery at Renown In making the decision to move forward to better health, it is important to remember: Obesity is a disease, and the desire to have a healthier, longer, more fulfilling life is possible. If you are interested in learning more, please visit the Bariatric Surgery Program page to view more information about Renown Regional Medical Center’s MBSAQIP accredited bariatric program, as well as information about upcoming educational seminars. Or call 775-982-RSVP (7787) to reserve your seat. Learn More
-
Jakob’s Journey at Renown Children’s Hospital
In August 2016, six-year-old Jakob was admitted to Renown Children's Hospital with what seemed like a common ear infection. Jakob's condition quickly progressed, and he started experiencing neurological symptoms such as difficulty speaking and a full-body shutdown. Doctors, neurologists and specialists from Renown worked with doctors from Stanford, where he was ultimately diagnosed with Bickerstaff brainstem encephalitis (BBE). BBE is a rare, autoimmune response that attacks the nerves in the body due to an acute illness such as a cold, flu or, in Jakob's case, an ear infection. Jakob could not breathe or eat and experienced paralysis on the side of his face, throat, stomach, bowels, lungs and legs. In addition, he started to rapidly lose weight as well as body function. Jakob lost half his body weight which resulted in the need for a Gastrostomy tube. This device is placed surgically and gives direct access to the stomach to give the child the nutrition needed. He also needed occupational therapy, and after three and a half months of ICU respiratory therapy, surgeries and treatments, he was released home to regain his strength. Forever Grateful Anica, Jakob's mom, said, "If it were not for the quick response and unconditional support and compassion from the team at Renown, Jakob would not be here today." Jakob's family is forever grateful to the staff, community and expertise at Renown for their unwavering commitment to their son and family during their most trying time in life. "When I met Jakob on the first day of his illness, so much was unknown. My team and I were worried, as his symptoms were very unusual. His rapid deterioration, after being a perfectly healthy child, was clearly terrifying for his parents. Handing over a child's care to a team of strangers is one of the scariest things that can happen to parents,” said Dr. Kris Deeter, Physician in Chief at Renown Children’s Hospital. “However, Anica and Jeremiah were also very clear that they did not want Jakob transferred somewhere else. So, we used all our resources to care for him, arrive at a diagnosis, and start aggressive therapies. They listened to every word we said, educated themselves, and became partners in Jakob's care. We all became part of Team Jakob, and soon, he proved to us just how strong he was." Today, Jakob is 13 years old and thriving in every aspect of his life. He is currently on the honor roll in school and finds joy in his newfound passion for the violin. He loves spending his free time learning about mixing music, making new friends and traveling to different parts of the country. This summer, he will travel to Europe to explore his passion for culture. The family says, "We owe it all to the family and staff at Renown."
Read More About Jakob’s Journey at Renown Children’s Hospital
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Stroke Survival as a Warrior – Kimi's Story
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Heart Attack Survivor Fights the Good Fight
Something wasn’t right. Even though it was the holiday season, on December 23, 2018, Mondo Corona didn’t feel good…not to mention his sudden earache. Although Christmas was a happy celebration with his family. He still felt tired. Was it the flu? And that darn earache wouldn’t go away. On that cool winter day, Mondo could not imagine he was near death. Or that he would become a heart attack survivor. Know Your Heart A few days later, on December 27, he wasn’t feeling any better. He decided to go to the emergency room at Renown Regional Medical Center. That’s when a simple blood test revealed shocking results. “I thought about death a lot. I was calling people to ask them to help take care of my family if I wasn’t going to be here anymore,” he emotionally confesses. Although Mondo loves his job as a railroad engineer, it involves on-call shifts and an erratic sleep schedule. At that time his exercise and eating habits weren’t the best either. Yet he never imagined he would have a massive, often lethal, type of heart attack called ‘the widowmaker.’ In fact, his family had been concerned about his health for awhile. “He worked so much and he didn’t take care of himself and he didn’t exercise – he was burning the candle at both ends,” shares his wife, Alison. His daughter Justice, an avid exerciser, was always encouraging him to join her at the gym, but could never quite convince him. Mondo remembers the time before he became a heart attack survivor. “I didn’t have any exercise whatsoever in my life. At that point my eating habits were just terrible,” he shares. He went to the emergency room due to his earache, but nothing was found until one of the doctors ordered some tests. Specifically blood work showed high troponin levels. Troponin is a blood protein often released in large amounts when the heart muscle has damage, sometimes by a heart attack. Heart Attack Survivor “My surgeon came in and told us that it was going to be a triple bypass – that three of the four…major arteries were clogged 100 percent,” Mondo explains. Amazingly his heart was pumping on only 10 percent blood flow. Heart surgeon, Joseph Brandl, MD, told him he survived a widowmaker heart attack. This type of heart attack happens when there is a 100 percent blockage in the critical left anterior descending artery (LAD) of the heart. Frequently the symptoms can often be mistaken for the flu. According to the Centers for Disease Control and Prevention (CDC), every 40 seconds a person in the U.S. has a heart attack. And 1 in 5 heart attacks are “silent” – meaning you can be a heart attack survivor, but not know it. For Mondo’s children, seeing their strong father struggle after heart surgery was difficult. Justice tearfully shares, “It was really hard seeing him so vulnerable. He really needed anybody’s and everybody’s help at that point.” A Heart Attack Survivor Program After leaving the hospital on January 5, 2019, he was extremely weak. On February 12, Mondo began Renown Health’s Intensive Cardiac Rehabilitation (ICR) Program called the Healthy Heart Program. This program, requiring a doctor referral, includes 12 weeks of supervised exercise along with nutrition education and stress management skills. In spite of heart disease being the leading cause of death in the U.S. – more than all cancers combined, the risk can be lessened with daily lifestyle habits. Mondo credits the ICR program with motivating him and getting his focus back on his health. He saw the team members setting an example and also caring about his health. He describes one of his favorite recipes, “In ICR Sara showed us how to make this incredible fruit salad, with jicama, watermelon, grapes, oranges, red onion, and ginger!” Of course, the recovery process was not overnight. “It did take a long time to really realize that he was going to be back to normal, that he was going to be okay and that he was going to be that strong provider for me and my children,” Alison reflects. “Mondo’s had an amazing outcome and he’s not limited in his activities at all and should hopefully have a life that’s not limited at all from heart disease as we’re monitoring everything and everything’s looking good,” reports his heart doctor Jayson Morgan, MD. Mondo describes his care experience being a heart attack survivor as life-changing. “The care teams at both Renown and ICR were incredible. There wasn’t a single person we came across who didn’t immediately become a part of the family. They truly cared for us, all of us, including the extended family that came to visit. They were informative and supportive. I felt like I created lasting bonds with so many of them, especially the gang in ICR. What amazing people.” Lynice Anderson, Director of Intensive Cardiac Rehab, Healthy Heart Program, shares,” Mondo is one of the most genuine, thoughtful and humble people I have ever met. His love for his family is palpable. His impact on me personally and our team is forever.” She acknowledges family support is key to his success, “Mondo’s family is his rock and they are his. I have never met a family that was so ‘all in’ in the support of their loved one. His new heart healthy lifestyle is modeled through his family every day.” Fighting The Good Fight Of course, Mondo may look familiar to you. That’s because he is featured in Renown Health’s “Fight The Good Fight” brand campaign. For this reason, you may have seen him in advertising working out on a treadmill, shirtless, with his open heart surgery scar in full view. When asked how he feels about showing his scar he confidently says, “I don’t mind showing it to people. I don’t. I earned that scar.” He is a proud heart attack survivor. Today, he’s grateful to be alive and takes his health commitment seriously. “Things have a different feel now. The skies and lakes are bluer and the trees greener. My family is so much more a part of my day. We go on so many more outdoor adventures, trying to incorporate a little exercise into our fun. We watch what we eat more and are trying to teach our children and loved ones about healthy choices. And I think with a few we’ve even been successful!” he observes. “Don’t take life for granted.” “Unconditional love. I get nothing but support from my family without them I wouldn’t be where I’m at. What happened to me definitely makes me a fighter for sure. I’m fighting for my life – the good fight – I think life is good,” he adds.
-
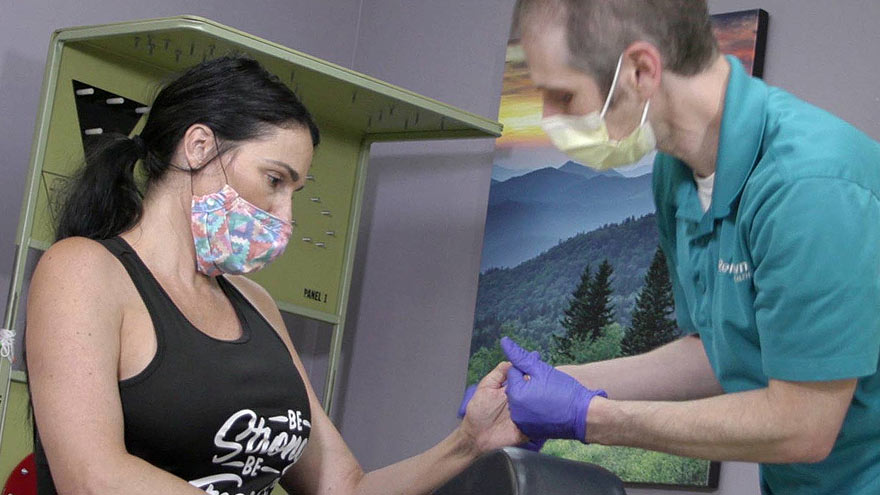
Helpful Caregivers Make a Wedding Dream Come True
A wedding is a big day for the wedding couple, but it’s also special for loved ones. A patient at Renown, Ken, got to take part in his daughter’s special day as her wedding plans changed to accommodate his medical condition. Grab some tissues and read how Renown’s team of compassionate caregivers and chaplains planned a wedding in Fianna’s Healing Garden. Ken was hospitalized at Renown Regional Medical Center where he was battling a lung problem – which was unrelated to COVID-19 – and his condition worsened rapidly on Wednesday, Aug. 12. His family made the decision to transition him to palliative care, which helps patients near the end of their lives remain comfortable, while supporting their dignity and quality of life. Ken’s medical condition altered wedding plans for his daughter, Chandra, and her fiancé, Tyler, who were planning to tie the knot later in 2020. Chandra wanted her father there, but knew he could not leave the hospital. That’s why Chandra’s sister, Heather, approached Ken’s care team with a request to have a small wedding ceremony at the hospital. Planning the Wedding A member of Ken’s care team, Amy Heston, registered nurse (RN), began planning how the wedding could be held outdoors in Fianna's Healing Garden in the E. L. Wiegand Pavilion, which was donated by the E. L. Wiegand Foundation. In 24 hours, Amy planned a wedding ceremony with the help of her colleague, Breyanna Aufiero, RN; the Renown Spiritual Care team; and nursing leaders on the coronary intensive care unit (ICU). Together, they decorated the aisle in the garden with flowers and battery-operated candles. They also made a sign for Ken’s hospital bed, which read, “Father of the Bride,” and crafted a bow tie for him to wear for the special occasion. With visitor restrictions in place at the hospital due to coronavirus (COVID-19), having the wedding outside in the Healing Garden allowed for more members of Ken’s family to attend including his wife, Charlotte, and his dog, Bella. Every step in planning the wedding required thoughtful and thorough care coordination so Ken could participate. His breathing was supported by oxygen and special arrangements were made to transport the oxygen tanks he needed to take part in his daughter’s wedding. Amy worked with respiratory technician, Kasey Benfield, and critical care technician, Ruben Duckworth, to ensure Ken’s oxygen needs were met using portable machines. Celebrating Love and Life Together Ken’s team of caregivers bathed him and shaved his face so he could look and feel his best for the ceremony. They put on his bow tie, covered his bed in decorations and his favorite blue, flannel blanket, and wheeled his bed outside for the ceremony. Renown associate chaplains Terri Domitrovich and Susan Palwick coordinated music and performed the ceremony for Chandra and Tyler on Thursday, Aug. 13, 2020. The bride and groom shared their first dance in the garden and Ken’s care team provided water and treats to give the family a full wedding experience. Shortly after the ceremony, Ken passed away. This wedding provided Ken and his family meaningful memories for their big life-changing moments as they celebrated and said goodbye. “Seeing Ken surrounded by family he never would have gotten to see again while in the hospital, watching him get to share a father-daughter dance with Chandra on her wedding day, and having him tell me that this day meant more to them than we would ever know were some of the most moving moments I’ve witnessed as a nurse,” Amy said. “I am so thankful for the team we have here. I know that this beautiful day wouldn’t have happened without the help of every single person who gave their time, money, creativity and passion to make it a day to remember.”
Read More About Helpful Caregivers Make a Wedding Dream Come True
-
Free Virtual Event! Saving Money on Medications
According to a National Center for Health Statistics survey, about 8% of U.S. adults are not taking their medications because they can’t afford them. This means millions of adults aren’t taking their medication due to the high cost. Virtual Event with pharmacist, Adam Porath Thursday, July 23, 11 a.m. to Noon Attend Virtual Lecture 5 Ways to Cut Medication Costs Safely Cost might not be affecting your medication plan, but the following ways to save money on medication can help: 1. Questions to ask your prescribing provider Do I have to take this medication? This is particularly a good question when you’ve been taking a pill for some time and not sure if you should continue. Is there a way to combine my medications? A good example of this is for those who are taking blood pressure medications. Do I have to take this particular pill? Often there are generic choices in the same medication class. Can I get a larger supply? Basically, knowing the cost of a 30- vs 90-day supply is always a good idea. In other words, it could save you time and money. This generally works for medications you take long-term. Remember, asking questions can help you save money on medication, so communicate your concerns. 2. Research online Find the website for the medication and look to see if there are savings and support available through the drug company. 3. Consider a co-pay card Co–pay card programs offered by drug manufacturing companies are a direct way to lower out-of-pocket costs for prescription drugs for eligible patients. The cards can patients pay for the medications they, or their doctors, prefer. If you don’t qualify for a co-pay card, then you can look into patient assistance programs. 4. Consider patient assistance programs Drug companies sponsor these programs by income and they are often hard to find. The best way to find a patient assistance program is by asking your pharmacist. 5. If you’re on Medicare, consider updating your plan Medicare plans can change from year to year, which often times includes the medication they cover and the co-payments or deductible amounts. Annual Enrollment takes place October 15 – December 7, 2020. Most important, review the options and shop around for the best plan. Visit Senior Care Plus for information on Medicare Advantage Plans available to you. Want to ask a pharmacist more questions on how to save on medication? Join us for a Sterling Silver Club virtual event on Saving Money on Medication. To learn more about the Sterling Silver Club, visit our club website.
Read More About Free Virtual Event! Saving Money on Medications