Search
-
How to Safely Store Breast Milk
Breast milk. It's often referred to as liquid gold. And fortunately, it can be safely refrigerated or frozen for later use, which can allow you to be a bit more flexible in your new routine with baby. Whether you're getting ready to return to work, planning for the chance date night out or just exclusively pumping, it's crucial to understand the guidelines for proper breast milk storage. Storing Breast Milk Use clean bottles with screw caps, hard plastic cups that have tight caps or nursing bags (pre-sterilized bags meant for breast milk). Be sure to label each container with the date the milk was pumped and your baby's name if the milk is going to childcare providers. You can add fresh, cooled milk to milk that is already frozen, but add no more than is already in the container. For example, if you have two ounces of frozen milk, then you can add up to two more ounces of cooled milk. For healthy full-term infants, milk can be stored as follows: Room temperature - six to eight hours (no warmer than 77°F, or 25°C). Refrigerator - up to five days at 32°-39°F (0°-3.9°C). Freezer– Varies depending on freezer type. Up to two weeks in a freezer compartment located within the refrigerator. Three to six months in a freezer that is self-contained (standard kitchen fridge/freezer combination) and kept at 0°F (-18°C). Breast milk should be stored in the back of the freezer and not in the door. Six to 12 months in a deep freezer that is kept at -4°F (-20°C). Be sure to leave about an inch of space at the top of the container or bottle to allow for expansion of the milk when it freezes. Thawing Breast Milk Place frozen breast milk in the refrigerator to thaw (about 24 hours) then warm by running warm water over the bag or bottle of milk and use it within the next 24 hours. If you need it immediately, remove it from the freezer and run warm water over it until it's at room temperature. Never microwave breast milk and do not refreeze it. Once your baby has started to drink from the bottle, you should use it within one hour. You may find that different resources provide different recommendations about the amount of time you can store breast milk at room temperature, in the refrigerator and in the freezer. Talk to your doctor or lactation consultant if you have any concerns or questions.
-
Stroke Survival as a Warrior – Kimi's Story
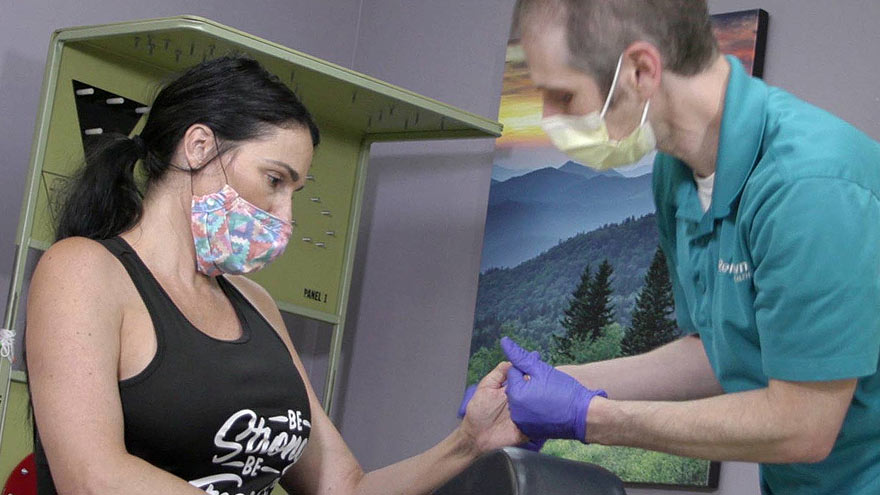
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Heart Attack Survivor Fights the Good Fight
Something wasn’t right. Even though it was the holiday season, on December 23, 2018, Mondo Corona didn’t feel good…not to mention his sudden earache. Although Christmas was a happy celebration with his family. He still felt tired. Was it the flu? And that darn earache wouldn’t go away. On that cool winter day, Mondo could not imagine he was near death. Or that he would become a heart attack survivor. Know Your Heart A few days later, on December 27, he wasn’t feeling any better. He decided to go to the emergency room at Renown Regional Medical Center. That’s when a simple blood test revealed shocking results. “I thought about death a lot. I was calling people to ask them to help take care of my family if I wasn’t going to be here anymore,” he emotionally confesses. Although Mondo loves his job as a railroad engineer, it involves on-call shifts and an erratic sleep schedule. At that time his exercise and eating habits weren’t the best either. Yet he never imagined he would have a massive, often lethal, type of heart attack called ‘the widowmaker.’ In fact, his family had been concerned about his health for awhile. “He worked so much and he didn’t take care of himself and he didn’t exercise – he was burning the candle at both ends,” shares his wife, Alison. His daughter Justice, an avid exerciser, was always encouraging him to join her at the gym, but could never quite convince him. Mondo remembers the time before he became a heart attack survivor. “I didn’t have any exercise whatsoever in my life. At that point my eating habits were just terrible,” he shares. He went to the emergency room due to his earache, but nothing was found until one of the doctors ordered some tests. Specifically blood work showed high troponin levels. Troponin is a blood protein often released in large amounts when the heart muscle has damage, sometimes by a heart attack. Heart Attack Survivor “My surgeon came in and told us that it was going to be a triple bypass – that three of the four…major arteries were clogged 100 percent,” Mondo explains. Amazingly his heart was pumping on only 10 percent blood flow. Heart surgeon, Joseph Brandl, MD, told him he survived a widowmaker heart attack. This type of heart attack happens when there is a 100 percent blockage in the critical left anterior descending artery (LAD) of the heart. Frequently the symptoms can often be mistaken for the flu. According to the Centers for Disease Control and Prevention (CDC), every 40 seconds a person in the U.S. has a heart attack. And 1 in 5 heart attacks are “silent” – meaning you can be a heart attack survivor, but not know it. For Mondo’s children, seeing their strong father struggle after heart surgery was difficult. Justice tearfully shares, “It was really hard seeing him so vulnerable. He really needed anybody’s and everybody’s help at that point.” A Heart Attack Survivor Program After leaving the hospital on January 5, 2019, he was extremely weak. On February 12, Mondo began Renown Health’s Intensive Cardiac Rehabilitation (ICR) Program called the Healthy Heart Program. This program, requiring a doctor referral, includes 12 weeks of supervised exercise along with nutrition education and stress management skills. In spite of heart disease being the leading cause of death in the U.S. – more than all cancers combined, the risk can be lessened with daily lifestyle habits. Mondo credits the ICR program with motivating him and getting his focus back on his health. He saw the team members setting an example and also caring about his health. He describes one of his favorite recipes, “In ICR Sara showed us how to make this incredible fruit salad, with jicama, watermelon, grapes, oranges, red onion, and ginger!” Of course, the recovery process was not overnight. “It did take a long time to really realize that he was going to be back to normal, that he was going to be okay and that he was going to be that strong provider for me and my children,” Alison reflects. “Mondo’s had an amazing outcome and he’s not limited in his activities at all and should hopefully have a life that’s not limited at all from heart disease as we’re monitoring everything and everything’s looking good,” reports his heart doctor Jayson Morgan, MD. Mondo describes his care experience being a heart attack survivor as life-changing. “The care teams at both Renown and ICR were incredible. There wasn’t a single person we came across who didn’t immediately become a part of the family. They truly cared for us, all of us, including the extended family that came to visit. They were informative and supportive. I felt like I created lasting bonds with so many of them, especially the gang in ICR. What amazing people.” Lynice Anderson, Director of Intensive Cardiac Rehab, Healthy Heart Program, shares,” Mondo is one of the most genuine, thoughtful and humble people I have ever met. His love for his family is palpable. His impact on me personally and our team is forever.” She acknowledges family support is key to his success, “Mondo’s family is his rock and they are his. I have never met a family that was so ‘all in’ in the support of their loved one. His new heart healthy lifestyle is modeled through his family every day.” Fighting The Good Fight Of course, Mondo may look familiar to you. That’s because he is featured in Renown Health’s “Fight The Good Fight” brand campaign. For this reason, you may have seen him in advertising working out on a treadmill, shirtless, with his open heart surgery scar in full view. When asked how he feels about showing his scar he confidently says, “I don’t mind showing it to people. I don’t. I earned that scar.” He is a proud heart attack survivor. Today, he’s grateful to be alive and takes his health commitment seriously. “Things have a different feel now. The skies and lakes are bluer and the trees greener. My family is so much more a part of my day. We go on so many more outdoor adventures, trying to incorporate a little exercise into our fun. We watch what we eat more and are trying to teach our children and loved ones about healthy choices. And I think with a few we’ve even been successful!” he observes. “Don’t take life for granted.” “Unconditional love. I get nothing but support from my family without them I wouldn’t be where I’m at. What happened to me definitely makes me a fighter for sure. I’m fighting for my life – the good fight – I think life is good,” he adds.
-
Six Tips for Healthy Vision
You might think worsening eyesight is inevitable as you age. But the truth is, there are easy things you can do to keep your eyes in tiptop shape for years to come. Clear vision is an essential part of overall health and there are daily habits we can adopt to keep our eyes seeing clearly. Mitchell Strominger, M.D., a registered ophthalmologist with Renown Health specializing in pediatric ophthalmology and neuro-ophthalmology, offers some everyday tips to keep you focused on eye health. Know your family’s vision history Look to your parents and grandparents for clues about the future of your eye health. Were they near-sighted at a young age? Do they have a history of eye crossing or a lazy eye? Did they develop glaucoma or macular degeneration (AMD)? Some genes have a strong association with eye health, specifically macular degeneration. AMD is a leading cause of blindness worldwide and the top cause of vision loss and blindness for Americans over 65, according to the Centers for Disease Control and Prevention (CDC). Also be aware certain medical conditions, such as diabetes, high blood pressure and liver disease, increase the risk of long-term eye problems. Receive regular vision screening exams Children under three need vision screening examinations by their pediatrician. A medical concern or family history warrants a comprehensive eye examination by a pediatric ophthalmologist (or general ophthalmologist or optometrist who has experience with children) per the American Academy of Ophthalmology (AAO). Vision screenings should occur every two years throughout adolescence unless pain, eye crossing, difficulty seeing the board or reading, or other eye concerns occur. In adulthood the risk of eye problems increases over age 40, so the AAO recommends regular dilated exams. When your pupils are dilated it allows your eye care professional a more accurate view of your retina and optic nerve, located in the back of your eye. This allows them to look for AMD or other eye problems. Eye diseases can be caught at their earliest stages during a dilated eye exam. “It is especially important to have your child evaluated as soon as possible if there is any concern for eye crossing or lazy eye,” says Dr. Strominger. “The visual system develops in the early years so intervention, whether it be glasses, eye patching to strengthen the vision in one eye, or eye muscle surgery is critical. Children at risk include those who are born premature, have development abnormalities, genetic disorders such as Downs syndrome, or a strong family history and should be evaluated at a young age. Often small problems are not clearly evident and cannot be picked up on routine screening examinations in the pediatrician’s office.” Block the sun, improve your vision Everyone knows not to stare directly into the sun, but indirect ultraviolet (UV) sun rays can cause serious harm over time. According to the National Eye Institute, sunglasses (or a protective UV tint) are a daily must to protect your eyes from: Cataracts (a clouding of the eye’s lens causing blurred vision) AMD - macular degeneration Pterygium (a tissue growth over the white surface of the eye that can cause astigmatism) Look for sunglasses which block 99 to 100 percent of both UVA and UVB rays. You still need sunglasses if your contact lenses block UV rays. Sun rays can damage your eyelids and other tissue not covered by contact lenses. Wearing sunglasses protects your entire eye area. Eat colorful meals Your eyes need vital nutrients to keep them healthy including vitamin C, zinc, beta carotene and copper. A diet filled with citrus fruits and a variety of vegetables provide these essential nutrients. Regularly filling up on fish high in omega-3 fatty acids (salmon, tuna, sardines) may reduce your risk of AMD and help maintain your eye health. Green, leafy vegetables (kale, spinach, collard greens) containing lutein and zeaxanthin are also a must for your dinner plate. Water your eyes Eyes, like the rest of your body, need plenty of water to prevent dehydration. Make sure you stay hydrated and steer clear of smoke to avoid dry eyes and irritation. Hours staring at the computer screen can also make your eyes feel dry or tired. Try regularly refreshing them with lubricating eye drops. Taking frequent computer breaks is also important. Follow the 20/20/20 rule: every 20 minutes, look at an object 20 feet away from you for 20 seconds. Eye makeup can also lead to dry eye as the glands at the base of the eyelashes may become clogged, causing dry eye. Make sure all eye makeup is hypoallergenic and is thoroughly removed with a gentle cleanser for the delicate eye area each day. Stop Smoking (or never start) Smoking is harmful to every part of your body, including your eyes. It's not only linked to cancer and heart disease but also cataracts, AMD, dry eye, optic nerve problems and many other problems. Smoking during pregnancy can also harm the eyes of the unborn child. If you currently smoke take steps to quit and your entire body will benefit.
-
Cancer Nutrition - Helpful Tips to Support Your Loved One to Eat Healthy
Eating healthy is a daily challenge for many, but for those with cancer it is an even harder struggle. A cancer diagnosis not only impacts those diagnosed, but family members and friends too. One key area of concern is making sure your loved one stays well by eating healthy food every day. Here are some essential cancer nutrition tips from Renown Health registered dietitians Jessica Blauenstein and Amy Laster. Help to Prepare Meals and Snacks for Daily Cancer Nutrition Make it grab and go. Easy-to-make meals help reduce the burden of having to cook and prepare food. Having easy to grab snacks on the counter or in the fridge can help ensure your loved one has access to those nutrients when needed. Sit outside of the kitchen. This allows your loved one to avoid cooking smells which can make them feel sick as a side effect of cancer treatments. Also try serving them cold foods such as sandwiches, cheese and crackers, or shakes which have a mild scent. Try drinkable meals. Some people with cancer find it easier to sip their calories over the course of 30 minutes to an hour. Consider smoothies or supplemental shakes such as Ensure Enlive or Boost Plus as snacks not meal replacements. A great foundation for a smoothie is a protein source (Greek yogurt, protein powder, nut butters or milk) with a carbohydrate (fruits, juice or berries). Add other ingredients as desired, such as spinach, kale, and ground flaxseed or chia seeds to give it more vitamins, minerals, and fiber. Snack Ideas for Those Undergoing Cancer Treatment The following ideas are both quick and easy to make for your loved one. Chicken or tuna salad with whole grain crackers or as a sandwich on whole grain bread Greek yogurt mixed with cereal, fruit and/or nuts Cottage cheese with banana, cinnamon and/or peanut butter Favorite fruit with 100% natural peanut or almond butter spread - Try peanut butter with bananas, apples, or even celery Their favorite veggies dipped in a salad dressing of your choice - For example, carrots with hummus or ranch dressing Cheese and whole grain crackers - Add tomato slices with a dash of oregano on top for more flavor Eggs scrambled with cheese, vegetables and/or salsa Peanut butter and jelly sandwich on whole grain bread A baked sweet potato with some favorite toppings Hard boiled eggs and/or egg salad with whole grain crackers, or as a sandwich on whole grain bread Oatmeal or cream of wheat prepared with milk, fruit and/or nuts Sometimes your loved one may not feel like eating or refuse to eat. If treatment side effects are impacting your loved one’s ability to eat, please visit the websites below containing recipes tailored to treat side effects. Cook for Your Life ELLICSR Of course you may also consult a registered dietitian and/or the patients care team, if you have more cancer nutrition concerns. No Appetite? Assisting with Cancer Taste Changes Taste changes are common during cancer treatment. Patients experiencing these changes may not feel like eating, which can negatively impact their nutrition. Help your loved one overcome taste changes with these cancer nutrition strategies: Metallic or bitter taste in food - add something sweet such as maple syrup, honey or jelly. You may also try adding fat, such as a nut butter, avocado or regular butter. Pickles or vinegar could help with this too. A taste like cardboard - try adding salt and extra flavor to foods with seasonings and spices. Some examples are onion, garlic, chili powder, basil, oregano, rosemary, tarragon, barbecue sauce, mustard, ketchup, or mint. Lemon juice, citrus, vinegar, or pickles may also help with this as well Food tastes too sweet - try adding six drops of lemon or lime juice. Add small amounts until the sweetness is gone. Very salty taste - try adding ¼ teaspoon of lemon juice. Try plastic utensils instead of metal, especially if your loved one is struggling with foods tasting metallic. Dipping small bites of food into either lemon juice or vinegar can have a “palate cleansing” feel and may improve taste perception. This helps avoid getting tired of the flavor after a few bites. Try marinating food or meats in sweet fruit juices, salad dressings, or sweet-and-sour sauce. Other “palate cleansing” foods are lime juice, orange juice, mangos, lemongrass, parsley, cilantro, mint, ginger, basil, and pickled foods. Use aroma to make foods appealing, avoiding any smells that may cause nausea. In particular, cinnamon, nutmeg, cloves, coriander, cumin, ginger, and black pepper can add an aromatic flavor. Also include herbs such as oregano, rosemary and thyme. Think texture. Consider trying wafers, crunchy nut butters, carrots, celery, cucumbers, chips, rice crispies, corn flakes, crackers, panko crumbs, nuts, or seeds if you are able to chew and swallow them safely. Remember that patience with your loved one's changing appetite and tastes can be the strongest form of support you can provide. Nutrition Tips for Cancer Survivorship and Beyond If eating large meals is difficult for your loved one, encourage them to snack throughout the day. Aim for 4-6 snacks or small meals per day. Focus on consuming 2-3 protein-rich foods each day such as lean animal meats, fish, eggs, soy or a protein supplement with 20-30 grams of protein per serving. Eat a variety of brightly colored fruits and veggies. Aim to make half of each meal fruits and vegetables. Eat less than 18 oz. (cooked weight) of red meat per week. Limit cold cuts, bacon, sausage, and hot dogs. Avoid excess salt and saturated fats. Cut back on simple carbs. (i.e. desserts, candies, white bread/pastas, french fries, packaged foods, chips) Drink in moderation- if at all- one drink per day for women, two for men. Get enough vitamin D (through diet and/or supplement) Avoid tobacco of any kind. Keep a healthy weight and stay up on exercise. Other Ways to Help a Loved One with Cancer Assist with Chores Allow your loved one to relax as you help take care of chores around the house, such as cleaning, cooking and grocery shopping. This may reduce overall stress and can be helpful for those that get tired after their treatments. Physical activity can still be beneficial, so be sure to do an activity together that they enjoy and is approved by their doctor. Be Patient It can be very difficult to see a loved one go through cancer treatment. Remember to be patient with your loved one. There may be things we want them to do or eat that we know would be good for them, however, meet your loved one with grace and understanding. It is ultimately their decision on what to do, just be there to support and assist them as they go through this challenging time. Additionally, Renown hosts free “Eating Well After Cancer Treatment” nutrition classes for cancer survivors. Our next cancer nutrition class series starts Thursday, June 3, 2021, and will be hosted virtually. It is open to anyone in the community. For more information or to register please click here.
Read More About Cancer Nutrition - Helpful Tips to Support Your Loved One to Eat Healthy
-
4 Breastfeeding Tips for New Moms
While breastfeeding is natural, it's not always easy. We asked Certified Lactation Counselor Sarah Mitchell for some tips to help make the process easier for mom and baby. From increased infant immunity to improved maternal health and well-being, the benefits of breastfeeding are many. Still, only 60 percent of U.S. moms in the United States continue to breastfeed past their baby's first six months. There are for many reasons for why moms stop, including the mother's their need to return to work. We reached out spoke to Sarah Mitchell, a certified lactation counselor at The Lactation Connection at Renown, for some expert advice. Tip 1 At first, it's normal to expect obstacles. Even in cultures where close to 100 percent of moms breastfeed, they can experience issues, including getting the baby to "latch on," sore nipples, and milk production. In addition, it sometimes can take several weeks for mom and baby to get comfortable. Tip 2 Line up a coach, even before the baby is born. This can be a professional lactation coach, family member, or friend who is experienced and encouraging. While online videos can be helpful, most new moms need the one-on-one guidance that a coach can provide. Renown offers outstanding resources in its Lactation Connection center, including expert consultants, products, and support. Tip 3 Well ahead of the due date, set up a support network of friends, family members, or community groups such as La Leche League. Women historically have relied on extended support systems to help them with raising children, and breastfeeding is one of those areas that, while natural, still needs encouragement from the women who’ve been there. Tip 4 Don’t get discouraged if you need to supplement at times with formula. This, too, as it turns out, is not uncommon in other cultures. In other parts of the world, babies are given beverages and foods such as tea, broth, soup, juice, mashed bananas, and papaya. The American Academy of Pediatrics recommends supplementation only with approved formula -- but the point is, it’s ok to supplement if you need to. Finally, don’t forget the importance of breastfeeding for connecting with your baby. It’s essential to maintain breastfeeding over the weekends, preferably “on-demand,.” and will keep that special bond strong after you have returned to your job.
-
Breast Feeding Doesn't Have To Mean Sore Nipples
If you think sore nipples are just a normal part of breastfeeding, think again. Robin Hollen, APRN, and Breastfeeding Medicine Specialist, says that nursing can be an enjoyable experience for mom and baby without pain and discomfort. A top concern of nursing moms within the first week after delivery is how to prevent sore nipples. Even moms who’ve nursed before struggle with this common issue. While many women think it is a regular part of the nursing experience, it is actually a sign that something isn’t quite right. “Nursing your baby should be enjoyable,” says Robin Hollen, Breastfeeding Medicine Specialist with Renown Health. For over 30 years Robin has been supporting moms to breastfeed. Below she shares some valuable information and tips, helping you create a happy and healthy breastfeeding experience for you and your baby. What causes sore nipples? The most common cause of sore nipples involves incorrect latching. For a proper latch, a baby’s mouth takes in the entire nipple and some of the breast, so that the nipple rests at the back of the mouth where the palate is soft. With an improper latch, the mouth may slip down to the tip of the nipple while the baby nurses. This constant pressure on your sensitive skin may cause discomfort and pain. A board-certified lactation consultant can help assess if your baby is latched correctly and troubleshoot your breastfeeding concerns. Less common causes of sore nipples include: • Improper tongue placement of baby • Clenching • Incorrect breast pump use How can a mother prevent sore nipples from an improper latch? Breastfeeding is a learning experience for both mom and baby. Ask for help with the latch so your baby learns it correctly and maintains its depth. In the past, new mothers were surrounded by a community of women — their own mothers, grandmothers, or other family and friends — to provide assistance and guidance with every latch at the beginning of an infant’s life. In today’s culture, new moms can find themselves on their own with no extended family to lend their knowledge. Nurses, pediatricians and lactation consultants now fill that role; they are the eyes and hands along with the much-needed experience to guide new mothers. Our Breastfeeding Medicine experts assist nursing moms with latch every day. Even a single visit with a lactation consultant observing your breastfeeding baby can provide valuable insight on achieving, and maintaining, the proper latch - preventing future nipple soreness and discomfort. How to heal sore nipples from breastfeeding To heal sore nipples, you must first fix the cause, and correcting the latch prevents further damage. A lactation consultant can also help you address the pain. Below are some breast healing tips: • Your own expressed breast milk is excellent to rub into the nipple for anti-bacterial protection. • For those moms who need more lubricant or fat than breast milk offers, use a lanolin or a cream that is labeled safe for the baby. • Soothies are a gel pads providing comfort in between feedings, but should not be used with lanolin products. • Breast shells, not to be confused with shields, can guard the nipples from irritation or pressure in between feedings. If you have more questions about preventing and healing sore nipples or general breastfeeding concerns, talk to your pediatrician or a Renown Health Breastfeeding Medicine specialist at 775-982-6365.
Read More About Breast Feeding Doesn't Have To Mean Sore Nipples
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
The Road to Recovery Close to Home
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.
-
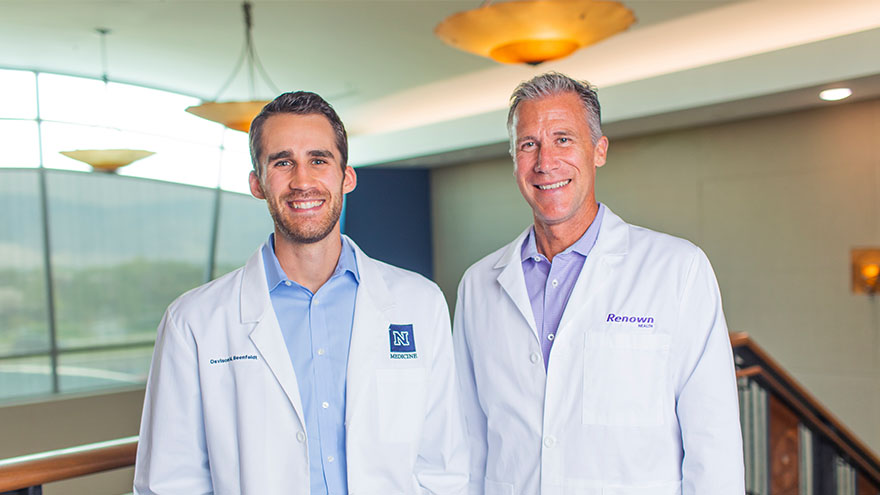
A Family's Legacy
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school
-
Reliable Care From Home
Renown Health has always been on the frontlines of technological advancement, and that innovation remained unwavering during the COVID-19 pandemic. Our telehealth teams heeded the call to provide home monitoring for our patients, transforming how we provide care. The care providers at Renown successfully monitored lower acuity COVID-19 patients from the comfort of their own homes. Bernard Lee was diagnosed with COVID-19 and pneumonia, and was able to return home to continue his recovery with a home monitoring system. While at home, Bernard’s health took a turn for the worse while he was sleeping, but thanks to the continuous monitoring of Health at Home, his worsening vitals did not go unnoticed. “This monitoring system really saved my life,” Bernard said. “It was telling me that my sats were low, but I didn’t even feel the common COVID symptoms; I just felt tired.” Because of his low oxygen saturation (sats) and the continuous monitoring, he woke up to providers calling to check on him in the early morning. He was immediately transferred to the Renown Intensive Care Unit to be cared for and monitored by our expert care teams. Today Bernard is recovering, feeling great and continuously refers to the team and the home monitoring system as his guardian angels.
-
What Foods to Eat and What to Avoid When Pregnant
Eating a well-balanced and nutritious diet when pregnant is one of the more essential things you can do for your baby and yourself. The basic principles of what to eat when pregnant are quite similar to how we should be eating all the time. This includes focusing on fruits, vegetables, whole grains, lean protein and healthy fats. Of course, there are a few areas that you should pay close attention to when you’re pregnant and a few foods you should avoid. We consulted Renown Health’s Caitlin Bus, RD, LD, CDE to learn more about pregnancy nutrition. Foods to Eat Regularly: Veggies Vegetables of all kinds -- and in all forms -- are beneficial for you and your baby during pregnancy. Veggies ensure your body is getting the fiber, vitamins and minerals it needs. However, fresh or frozen veggies are considered best, but if you choose to eat canned veggies, make sure you choose a low sodium product. The more greens, the better! If you have an aversion to vegetables, especially in the first trimester, try sneaking them into smoothies. Healthy Proteins Protein-rich foods support your baby's growth while giving your body the nutrients to build and repair tissues, including your muscles, hair, skin and nails. Although protein requirements vary from person to person, a pregnant woman needs additional protein for her baby's growth, especially in the second and third trimesters. Regularly eating high protein foods -- like fish, chicken, turkey, eggs, peanut butter, nuts and beans –– promotes your baby's healthy brain and heart development. Grains Food like brown rice, quinoa, whole-wheat pasta and oatmeal are great to eat while pregnant. They are rich in fiber, iron, B vitamins and folic acid, which are all beneficial to physical development. Grains also help alleviate constipation and hemorrhoids. Fruits Fruit can help satisfy any sugar cravings you have when pregnant while also supplying your baby with nutrients – it's a win-win. Some people advise against fruit consumption while pregnant, but this is a myth. Like with all foods, moderation is key. Fruit can be high in sugar, so it is important to be aware of your intake. Also, make sure you are mindful of your preparation – thoroughly rinse produce under running water for 30 seconds to help avoid foodborne illness. Pasteurized Dairy Dairy products like milk, cheese and yogurt can be great sources of protein and calcium needed for the healthy development of a baby's bones, teeth and muscles. These foods also help with ensuring healthy heart function and nerve transmission. When buying these products, make sure to choose pasteurized products to avoid exposing your body to germs and bacteria. The American College of Obstetrics and Gynecology recommends 1,000mg of calcium per day for pregnant and lactating women. This equates to 4 servings of dairy or calcium-rich foods such as leafy greens, broccoli, tofu, almonds or dried figs. DHA Omega-3 Fats Omega-3s like DHA help support the health of a baby's brain and parts of their eyes. Women who are pregnant or breastfeeding should eat at least 8 ounces and up to 12 ounces of seafood each week. Ideally, food sources that offer DHA omega-3 and that are lower in mercury should be emphasized in your diet, including fish like salmon, sardines and anchovies. If you do not eat fish or omega-3 fortified foods, a DHA omega-3 supplement is recommended. Choline Did you know that 92% of pregnant women fail to meet the daily choline recommendation? Choline is crucial for an infant's brain and central nervous system development. One egg supplies 33% of the recommended daily intake. Although choline is often absent or low in prenatal vitamins, the best food sources include eggs, meats, fish, dairy, navy beans, Brussels sprouts, broccoli and spinach. Iron and Folic Acid Iron is the most common nutrient deficiency during pregnancy. Foods with high and moderate amounts of iron include red meat, chicken, fish, fortified cereals, spinach and beans. Folic acid is used to make the extra blood your body needs during pregnancy. Consuming adequate folic acid early in pregnancy reduces the risk of birth defects that affect the spinal cord. It is recommended to consume 400 micrograms (mcg) per day for pregnant women. This amount is included in your prenatal vitamins. Water Staying hydrated is one of the best things you can do for yourself and your baby when pregnant. In addition to just being good for you, hydration alleviates morning sickness and nausea, while dehydration can lead to contractions and even pre-term labor. Aim for 10 cups of fluids per day, on top of the water naturally occurring in foods. Foods to Avoid: Raw Fish and Fish with High Mercury Content Sorry sushi fans, according to the Center for Disease Control and Prevention, pregnant women are 10 times more likely to get infected by Listeria, a bacteria found in raw or undercooked fish. Also, avoid fish often found to be high in mercury, including swordfish, king mackerel, tuna and marlin. Processed or Raw Meat Similar to eating raw fish, eating undercooked or raw meat increases your risk of infection while pregnant. Hot dogs and lunch meats should also be avoided, unless they have been reheated to be steaming hot (for example, in a microwave). Alcohol Drinking alcohol when pregnant can impact your baby’s brain development and increases your risk of premature birth, low birth weight or miscarriage. Just don’t do it! Minimize Caffeine High caffeine intake during pregnancy can restrict your baby’s growth; therefore, it is recommended that pregnant people limit their caffeine intake to less than 200 mg per day – that’s roughly two cups (16 fl oz) of coffee per day. Runny Eggs Eating raw or runny eggs when pregnant increases your risk of Salmonella, which can cause fever, nausea, vomiting, stomach cramps and diarrhea. Always make sure your eggs are cooked through or use pasteurized eggs.
Read More About What Foods to Eat and What to Avoid When Pregnant