Search
-
Prevent Osteoporosis: Take Control of Your Bone Health Today
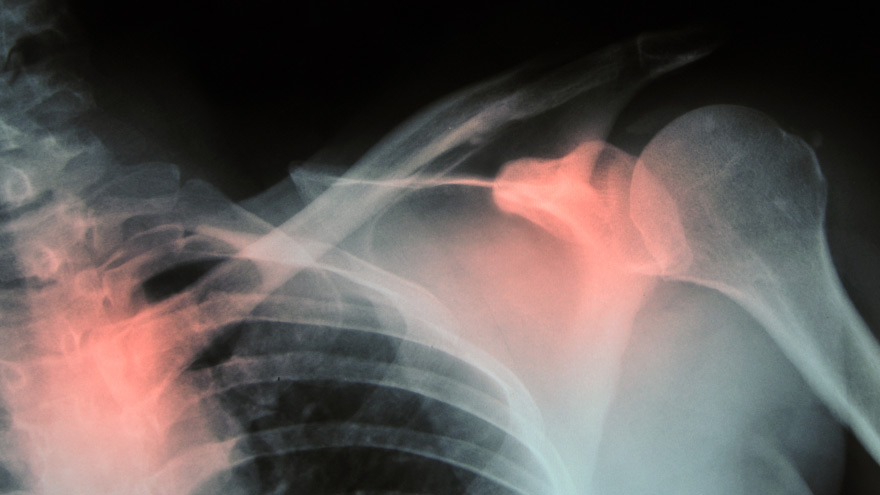
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
Ask the Expert: What is Scoliosis?
Posture is important, but for those children diagnosed with scoliosis (spinal curvature) it can be a difficult issue. The Washoe County School District Student Health Services Department screens 7th grade students for scoliosis as growth spurts often reveal the condition and, if diagnosed early, scoliosis can stop progressing. We asked Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis to answer some frequently asked questions about scoliosis. What is scoliosis? There are many types of scoliosis: early onset (occurs before age 10), congenital scoliosis is when the bones of the spine do not form correctly, neuromuscular scoliosis which is due to children’s neurologic and muscle disease, and the most common is Adolescent Idiopathic Scoliosis. The term “idiopathic “ means the exact cause is unknown, although we do know it runs in families. This type of scoliosis occurs in 2-3 percent of adolescents and is mainly seen during their growth spurt. This is why middle school screenings are recommended. Both genders get scoliosis but girls are 8 times more likely to have their curves progress and become larger. What are the signs that my child may have scoliosis? A few signs for parents to watch for are: One shoulder might be higher than the other. One leg may seem longer. A hip may be higher or look more prominent. The waist may not look the same from side to side (asymmetry). The trunk or rib cage may be more prominent on one side or shifted. When they bend forward they may have a bump on their back. How is scoliosis diagnosed? It can be noticed by a pediatrician at a physical, school screening nurse, PE teacher or parents. Once the curve is suspected the child is usually referred to a pediatric orthopedic surgeon scoliosis expertise. At the initial visit the doctor will perform a thorough physical including a complete neurologic exam to assess the amount of curvature. Once the exam is completed the physician will determine if a spinal x-ray is needed. The curve on the x-ray is measured utilizing the cobb angle (a measurement in degrees) which helps guide the treatment. What are common treatments for scoliosis? The treatment depends on the size of the spinal curve and the amount of growth the child has remaining. An x-ray of the child’s hand is used to determine the amount of growth remaining. This allows the determination of the child’s bone age, and based on the hands growth plates it can determined if the child is in their rapid phase of growth. Treatments include: Observation - For curves less than 20-25 degrees. This entails visits every 6-9 months with a repeat scoliosis x-ray. Since scoliosis curves increase only 1-2 degrees per month, and variations in measurements can be 3-5 degrees, an x-ray is not recommended before 6 months. If the curve remains less than 25 degrees the child is followed until their growth is completed (usually age 16-18). Progressing Curve - If growth is finished and the curve is less than 40 degrees, the risk of more curvature into adulthood is small. If growth is completed and the curve is over 45 degrees, the child is followed for several years as these curves can progress into adulthood. If the patient is still growing and the curve has progressed greater than 25 degrees but still in the non-operative range (less than 45-50 degrees) bracing is used to stop the progression of the curve. Bracing - Indicated for curves over 25 degrees but less than 45 degrees. If a brace is required you will be referred to an orthotist (bracing specialist). The orthotist assesses your child, reviews the x-ray and then fits the brace. (Having a brace made usually takes 2-3 weeks.) Once the brace is fit, your child will visit the scoliosis specialist for an x-ray in the brace to ensure it fits correctly. The primary goal of bracing is to halt progression of the curve and prevent the need for surgery. The brace must be worn for about 16 hours per day to be effective. In a recent bracing study 72% of the patients who wore their braces as prescribed prevented the need for surgery compared to the group who did not wear their brace. Surgery: When a curve reaches 45-50 degrees, and a child is still growing, surgery is usually recommended because the curve is likely to continue progress. If a curve is over 50 degrees and the child is done growing surgery also may be recommended. This is because when curves are over 50 degrees they tend to increase 1-2 degrees per year for the rest of your life. As curves get larger the amount of lung function tends to decrease which could cause breathing problems later in life. The goals of surgery are to stop the progression of the curve and safely correct any misalignment. This is accomplished by attaching implants (rods, screws, hooks and bands) to the spine. Bone graft is then placed around the implants to encourage the spine to fuse (grow together). This then forms a solid column of bone with metal rods in place, preventing the curve from changing. Most patients are back to their regular sports and activities six months post surgery.
-
Copays vs. Coinsurance: Know the Difference
Health insurance is complicated, but you don't have to figure it out alone. Understanding terms and definitions is important when comparing health insurance plans. When you know more about health insurance, it can be much easier to make the right choice for you and your family. A common question when it comes to health insurance is, "Who pays for what?" Health insurance plans are very diverse and depending on your plan, you can have different types of cost-sharing: the cost of a medical visit or procedure an insured person shares with their insurance company. Two common examples of cost-sharing are copayments and coinsurance. You've likely heard both terms, but what are they and how are they different? Copayments Copayments (or copays) are typically a fixed dollar amount the insured person pays for their visit or procedure. They are a standard part of many health insurance plans and are usually collected for services like doctor visits or prescription drugs. For example: You go to the doctor because you are feeling sick. Your insurance policy states that you have a $20 copay for doctor office visits. You pay your $20 copay at the time of service and see the doctor. Coinsurance This is typically a percentage of the total cost of a visit or procedure. Like copays, coinsurance is a standard form of cost-sharing found in many insurance plans. For example: After a fall, you require crutches while you heal. Your coinsurance for durable medical equipment, like crutches, is 20% of the total cost. The crutches cost $50, so your insurance company will pay $40, or 80%, of the total cost. You will be billed $10 for your 20% coinsurance.
-
Health Insurance Terms Explained: Deductible and Out-of-Pocket Maximum
Health insurance might be one of the most complicated purchases you will make throughout your life, so it is important to understand the terms and definitions insurance companies use. Keep these in mind as you are comparing health insurance plan options to choose the right plan for you and make the most of your health insurance benefits. One area of health insurance that can cause confusion is the difference between a plan's deductible and out-of-pocket maximum. They both represent points at which the insurance company starts paying for covered services, but what are they and how do they work? What is a deductible? A deductible is the dollar amount you pay to healthcare providers for covered services each year before insurance pays for services, other than preventive care. After you pay your deductible, you usually pay only a copayment (copay) or coinsurance for covered services. Your insurance company pays the rest. Generally, plans with lower monthly premiums have higher deductibles. Plans with higher monthly premiums usually have lower deductibles. What is the out-of-pocket maximum? An out-of-pocket maximum is the most you or your family will pay for covered services in a calendar year. It combines deductibles and cost-sharing costs (coinsurance and copays). The out-of-pocket maximum does not include costs you paid for insurance premiums, costs for not-covered services or services received out-of-network. Here's an example: You get into an accident and go to the emergency room. Your insurance policy has a $1,000 deductible and an out-of-pocket maximum of $4,500. You pay the $1,000 deductible to the hospital before your insurance company will pay for any of the covered services you need. If you received services at the hospital that exceed $1,000, the insurance company will pay the covered charges because you have met your deductible for the year. The $1,000 you paid goes toward your out-of-pocket maximum, leaving you with $3,500 left to pay on copays and coinsurance for the rest of the calendar year. If you need services at the emergency room or any other covered services in the future, you will still have to pay the copay or coinsurance amount included in your policy, which goes toward your out-of-pocket maximum. If you reach your out-of-pocket maximum, you will no longer pay copays or coinsurance and your insurance will pay for all of the covered services you require for the rest of the calendar year.
Read More About Health Insurance Terms Explained: Deductible and Out-of-Pocket Maximum
-
Understanding "In-Network" and "Out-of-Network" Providers
When finding a provider to receive your health services, you've probably heard the terms "in-network" and "out-of-network" when it comes to your health plan. But what do these terms mean for a patient? And why should you be aware if a provider is out-of-network? What does it mean when a provider is "in-network" with a health plan? A provider is a person or facility that provides healthcare. When a provider is in-network it means there is a contractual agreement with that health plan regarding the rates for services. The provider will accept negotiated rates for services from the insurance. This means a patient will typically pay less for medical services received and is less likely to receive surprise bills. What does it mean when a provider is "out-of-network" with a health plan? Providers that are out-of-network are those that do not participate in that health plan's network. The provider is not contracted with the health insurance plan to accepted negotiated rates. This mean that patients will typically pay more or the full amount for the service they receive. Why should patients see in-network providers? Seeing an in-network provider for medical services can significantly reduce your medical expenses. Remember that in-network providers have a contractual agreement for negotiated rates with the health plan, so they cannot charge you more than that negotiated rate for a service. Seeing an in-network provider will always ensure any costs you do incur (copays or co-insurance) are applied to your health plan's deductible and out-of-pocket maximum (out-of-network costs don't apply to these amounts). To find the amounts you will pay for specific services, you can check your health insurance plan's Summary of Benefits. What is the best way to find which providers are in-network with a patient's health plan? Most health insurance companies offer multiple ways to find if a provider is in-network. To find the most accurate benefit information from your health plan, you can: Call their Customer Service department Check their website for their online provider directories If offered, check your online member portal.
Read More About Understanding "In-Network" and "Out-of-Network" Providers
-
Making Patient Safety the Priority It Deserves to Be
I am regularly amazed by medical advancements and innovation in the United States. However, even as we make significant progress in many areas of medicine, there is still much more work to be done in others. One such area is patient safety. What is Patient Safety? When we talk about patient safety, we are discussing how hospitals and healthcare organizations protect patients from errors, injuries and infections. Anyone can make a mistake at work, but in healthcare these mistakes can result in serious outcomes. In 1999, the Institute of Medicine released a report that estimated 98,000 deaths per year result from medical examination or treatment. The most recent study in 2013 suggested these numbers could range from 210,000 to 440,000 deaths per year. Many of these deaths result from preventable medical errors. This is inexcusable and shows how much more work our industry still needs to do to improve patient safety. Making Patient Safety a Priority Patient Safety is our number one priority at Renown Health. We dedicate a lot of time to establishing, reviewing, and revising our processes to prevent errors. Despite the obvious importance of patient safety, this issue is largely left to individual hospitals and health systems to manage. There is a surprising lack of national attention around this truly important issue. However, a silver lining of the COVID-19 pandemic is that it is igniting interest in hygiene and infection prevention. Patients want to learn more about the processes that are in place to prevent the spread of infections. In addition to the many protocols that guide our treatment of injuries and illness, Renown Health has implemented the following measures to prevent the spread of communicable diseases: Requiring everyone entering Renown sites to wear a mask or face covering. Establishing new processes to help patients and visitors practice social distancing. Limiting the number of visitors in our facilities. Screening all employees and patients for symptoms. Enhancing our already-thorough cleaning and disinfection processes. I hope patient safety and infection prevention remain in the national spotlight long after the COVID-19 pandemic has ended. The healthcare industry must come together to develop stronger systems and regulations to minimize preventable medical errors. We have a responsibility to our patients to do better.
Read More About Making Patient Safety the Priority It Deserves to Be
-
3 Ways to Switch to a Medicaid Plan Accepted at Renown
Medicaid plays a significant role in our health care system and is the nation’s public health insurance program. In addition, this program is the predominant source of long-term care coverage for Americans. Renown Health is contracted with two Medicaid plans: Molina and Anthem. If you currently have a different plan but want to change to one that Renown accepts, you can request to change plans during the open enrollment period from January 1 to March 31. Request to change your Medicaid plan in one of three ways: Request a change to your plan, or managed care organization (MCO), by reviewing the available MCO plans online at bit.ly/MCOPlansNV and filling out the form on the webpage. Email Nevada Medicaid to ask for a plan change and include your name, Medicaid ID and the names and Medicaid IDs of any dependents in your home: MCORedistribution@dhcfp.nv.gov. Call your local Medicaid district office at 775-687-1900 (northern Nevada) or 702-668-4200 (southern Nevada) to ask about changing your plan. For more information about the Medicaid plans accepted at Renown Health, please visit: Anthem Molina Healthcare Renown Health accepts most insurances, but please visit the link below for the full list. Click here for all accepted plans
Read More About 3 Ways to Switch to a Medicaid Plan Accepted at Renown
-
Addressing the Threat of Workplace Violence in Hospitals
In recent years, workplace violence against healthcare workers has been on the rise. According to the Occupational Safety and Health Administration (OSHA), about 75 percent of nearly 25,000 reported annual workplace assaults occur in healthcare and social service settings. Those who don’t work in healthcare may be surprised to learn that violent altercations are so common in our field. Hospital settings can create fear and stress for patients and their families. Pain, mind-altering medications and drugs, and difficult prognoses can amplify these feelings. While inappropriate responses may be understandable, violence cannot be tolerated. As the leader of a health system, protecting our employees is an issue that I take seriously. Reporting Workplace Violence Unfortunately, sometimes employees don’t report dangerous incidents fearing they might be blamed, or not realizing it’s a reportable offense. At Renown Health, we take these events seriously. We have clear, mandatory policies and protocols for reporting and investigating violent incidents. Each incident is investigated to ensure follow through and accountability. We also teach de-escalation skills to our hospital security teams, clinicians, and other frontline employees. As an added layer of protection, Renown Health has a first-rate security team that closely monitors activity on our campuses, addressing potential issues before they escalate. Our organization values our partnerships with community organizations including local law enforcement agencies like the Washoe County Sheriff’s Office and the Reno Police Department. Renown Health maintains a close relationship with these partners, and we alert them when our care teams experience an increase in violent incidents. I also recognize that workplace violence is a national problem that demands collaborative solutions. That’s why I am also proud to serve as a member of the American Hospital Association’s Hospitals Against Violence Advisory Committee. Nurses, doctors, paramedics, and frontline health workers care for us every day. It’s our responsibility to support them by ensuring they feel safe at work.
Read More About Addressing the Threat of Workplace Violence in Hospitals