Search
-
Get to Know the Types of Car Seats
Parents often struggle with installing and choosing car seats for their children. Picking out a car seat for your child is a never-ending battle. Safe Kids Washoe County has made it simple for you to understand the types of car seats that will work for your child. Types of Car Seats Rear-Facing Only Seat. Your baby's first car seat is often used from 5 to 40 pounds. People usually buy this type of seat because it is portable. Convertible Car Seat. This seat is larger and stays in the car; it may be rear-facing until your child is two years or more. After that, it can change to a forward-facing seat. Forward-facing-only car seat. This type of seat is used in one direction and has a 5-point harness and top tether. Combination seat. This is a forward-facing seat with a 5-point harness and top tether and can change into a booster seat when you remove the harness. 3-in-1 car seat. This seat also stays in the car. You can use it rear-facing, forward-facing, and then later, as a booster seat. Booster seat. It boosts the child for a safer and more comfortable fit of the adult seat belt. Make sure your child has outgrown the weight or height limits allowed in the forward-facing car seat. The seat belt must lie flat across your child's chest, on the bony part of the shoulder, and low on the hips or upper thighs. Most children will be between the ages of 8 to 12 years old before they are ready for the seat belt alone. Have a trained car seat technician check your installation Why: 3 out of 4 car seats are installed improperly, with some studies show that the misuse rate is 90%, with the average car seat having three mistakes. Solution: Ensuring that your child's car seat is installed correctly by a certified car seat technician will ensure your child's safety.
-
Transitioning Your Child Out of Their Car Seat
Car seat technicians often find parents are moving their child to their next car seat stage too soon, as they get older. Here are a few reminders of when to transition your child from their booster seat to a seat belt. Moving to a booster seat too soon According to Safe Kids Worldwide, nearly 9 in 10 parents remove children from their booster before they’ve reached the recommended height, weight, or age of their car seat recommendations, which leaves the seat belt in a position on the child that could injure them. If the child is not the proper height, the seat belt can rise up on the belly, instead of the hips where it’s supposed to sit, which can lead to spinal cord damage or whiplash in the event of a car crash. Solution: You can switch from a car seat to a booster seat when your child has topped the weight allowed by the car seat manufacturer; typically 40 to 80 pounds (18 to 36 kilograms). Remember, however, that your child is safest remaining in a car seat with a harness for as long as possible. Booster seats must always be used with a lap and shoulder belt — never a lap-only belt. Transitioning to a safety belt too soon Older children need booster seats to help ensure the seat belt stays properly positioned on their body. The lap belt should lie low across the child's hips and pelvis with the shoulder belt crosses the middle of the child's chest and shoulder, so that in the event of a crash, the forces are applied to the hip bones and not the abdomen. If the lap belt is not positioned properly then it could lead to injuries to the spinal cord and abdominal organs. Solution: Most kids can safely use an adult seat belt sometime between ages 8 and 12. Always use a booster seat until the child passes the 6-step test Your child reaches a height of 4 feet, 9 inches (nearly 1.5 meters) Their back is flat against the seat back. Knees bend over the edge of the seat and feet are flat on the floor. The shoulder belt sits on their shoulder and chest (not face or neck.) The lap belt sits low on their hips and touches their upper thighs (not on their stomach.) Your child can sit comfortably this way for the entire trip. The American Academy of Pediatrics reminds us that the back seat is the safest place for children younger than age 13.
Read More About Transitioning Your Child Out of Their Car Seat
-
Pool Safety: Things To Know About Drowning
The warm weather is here and pools are open. Swimming is a great way to keep your kids cool, occupied and exercised throughout summer, however pools come with their fair share of risks. Before you take your children swimming, check out these pool safety tips. Pool safety is something every parent needs to take more seriously. Why? Because drownings of young children ages one to four have increased in recent years. Unfortunately, drownings are the number one cause of death in this age group - we lose the equivalent of 10 school buses full of children to fatal drownings in the U.S. each year. With warmer temps and hopes of cooling off in a local pool, you can’t be too careful when it comes to protecting your children from the risk of drowning. Children are naturally drawn to water, so parents must be extra aware in order to protect their kids from diving in headfirst. Kris Deeter, MD, pediatric intensive care physician at Renown Children’s Hospital, offers tips to keep your littles safe in the water. Preparing Your Child for the Pool People aren’t born knowing how to swim. This means parents must teach their children about swimming and pool safety if they want them to be safe and confident around water. It can take years to develop these skills, so the key is to start when your children are very young. Here are some ground rules: Teach your child to swim starting at age one. We recommend enrolling your toddler in swim classes; there are several organizations in the Reno-Tahoe area that offer baby and toddler swim classes. Keep your kids away from plastic and inflatable pools - they’re easy for children to fall or climb into and drown. They’re also a breeding ground for bacteria. Floaties and water wings are not safe! They are not a safe substitute or “crutch” for learning how to swim and they can lead to drowning if the child is using them incorrectly or while unsupervised. Stay within arm’s reach of babies and toddlers when at the pool. Supervision alone is not enough – you must be within arm’s reach in case they fall in and need to be rescued quickly. Learn child and infant CPR. If a drowning does occur, the best course of action is to call 911, get the child onto dry land and conduct CPR until breathing is restored or the EMTs arrive. Pool Parties: A Risk for Drowning? Surprisingly, pool parties, a common summer pastime, actually increase the risk of drowning incidents. Although responsible adults are usually at pool parties, distractions ranging from alcohol to pool toys can actually make it easier for drownings to occur unnoticed. Does this mean you should RSVP “no” to the next pool party your child is invited to? Not if you follow the pool safety tips below: Attend the party with your child so you can supervise them while they swim. Remove unused floaties and toys from the pool. They can obscure visibility, making it difficult to see a child in the pool. Don’t drink alcohol while supervising a pool party. Assign an adult “water watcher” to pay constant attention to children in the pool. Pool Safety Precautions for Homeowners If you own a pool, there are several more precautions to ensure the safety of your children. Even if your kids are strong swimmers who have mastered the rules of pool safety, there may be neighbors or friends who are younger and more vulnerable to drowning. You must undertake precautions for these children too. Some of these may seem time-consuming or expensive, but they are worth it to prevent a child from a fatal drowning. To keep your pool or spa safe, please: Cover your pool or spa when not in use. Choose a pool or spa cover with safety features like locks, safety sensors or alarms. Fence in your pool or spa area. The fence should be locked and at least four feet tall. Do not leave toys in the pool area as these may attract children.
-
2 Dangerous Car Seat Mistakes and Solutions
Car seat mistakes can have very serious consequences. Misuse of a car seat can injure your child, or fail to keep them safe in the event of a crash. A lot goes into finding the right car seat for your child. With so many factors to consider (including age, weight and height of the child, type and brand of a car seat, cost of the car seat, etc.) it can be easy to forget critical factors. Here are two common mistakes that certified technicians often find when speaking with parents. Mistake #1: Getting a used car seat without knowing its history Why: A used or secondhand car seat can pose several factors that can compromise its safety in a crash. First, car seats expire six to ten years after their date of manufacture, so refer to the car seat's manual for recommended car seat longevity. The safety mechanisms can be compromised if a car seat has been in a crash. So it's crucial to replace your car seat following a collision. Solution: Only use a car seat if you know its history. A new car seat is your best bet, as they are up to date on the latest safety guidelines, and safety mechanisms are up to standard. However, if you are considering a used car seat for your child, please ensure the following: The car seat has never been in a car crash. The car seat isn't expired or outside the manufacturer's recommended longevity. It comes with the car seat manual and has all safety labels, including manufacture date, model number, and use instructions and restrictions. The car seat or any of its parts have not been recalled. The overall state and integrity of the car seat and its parts are undamaged. The carseat or any of its parts have not been recalled and are present and in working order.
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Stay Inside When Skies Are Smoky
Even when fires burn outside our area, the air quality in the region can reach dangerous levels. Our expert explains how to maintain your lung health when fire season strikes. It’s a sight we know all too well as northern Nevadans — a hazy or thick layer on the horizon when smoke rolls in from nearby fires. Sometimes the smoke is more evident than others, but it’s important to remember, even when the smoke may not be as visible across the valley, it still impacts our air quality. The last week or so, our air quality has been in the “unhealthy for sensitive groups” range, which can be dangerous for people who are sensitive to air pollution. Air Quality Changes: Who’s at Risk? Renown Pediatric Pulmonologist Sonia Budhecha, M.D., explains certain people are especially at risk when smoke moves in: Older people, whose lungs are not as healthy as they used to be Young children, whose lungs are still developing People with heart and lung disease including asthma, COPD and emphysema “Smoke and haze from fires carry particulates that can get into your respiratory system and eyes, which can be a danger for all ages,” Dr. Budhecha says. How You Can Protect Yourself Until the smoke clears and the air returns to the “good” range, it is best to follow these tips to protect yourself and your family: Stay indoors and keep windows closed Turn on the air conditioning to recirculate clean air Drink plenty of fluids to help your body flush out any toxins you inhale Additionally, all community members should reduce their physical activity and try to prevent heavy exertion outside. If you or a loved one has a heart or lung disease, avoid physical exertion altogether because smoke can aggravate these conditions. “People with heart disease may experience shortness of breath, chest pain, palpitations or fatigue,” Dr. Budhecha says. “People with lung disease may also have shortness of breath, chest discomfort, wheezing, phlegm or a cough.” Smoky Signs and Symptoms Smoke can also impact healthy people — irritating your eyes, nose or throat. And in some cases, inhaling smoke can lead to bronchitis. When haze moves into our area, keep an eye out for these symptoms: Burning or stinging eyes Runny nose Cough or scratchy throat Headaches Wheezing Shortness of breath Difficult taking a full breath Chest heaviness Lightheadedness Dizziness If experiencing any of the above symptoms, seek medical attention or call your doctor for advice. Sometimes, these symptoms do not appear for as long as 24 to 48 hours after smoke inhalation. For those that have pre-existing lung or heart conditions, consult with a health care provider on action or management plans. To schedule an appointment Visit Renown Pulmonary Medicine, or call 775-982-5000. Understanding Our Air Quality The Air Quality Index (AQI) is broken down by large (PM10) and small (PM2.5) particulates. According to Dr. Budhecha, large particulates are usually ones that can be seen and smelled. They can damage your eyes and nose but don’t often get deep in the lungs or blood vessels. “The more dangerous ones are PM2.5, which can’t always be seen or smelled,” Dr. Budhecha says. “Any time the AQI is above 51, children with lung or heart disease should not be outdoors.” For the latest air quality update in your area, visit AirNow.gov or call (775) 785-4110.
-
Stroke Survival as a Warrior – Kimi's Story
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Heart Attack Survivor Fights the Good Fight
Something wasn’t right. Even though it was the holiday season, on December 23, 2018, Mondo Corona didn’t feel good…not to mention his sudden earache. Although Christmas was a happy celebration with his family. He still felt tired. Was it the flu? And that darn earache wouldn’t go away. On that cool winter day, Mondo could not imagine he was near death. Or that he would become a heart attack survivor. Know Your Heart A few days later, on December 27, he wasn’t feeling any better. He decided to go to the emergency room at Renown Regional Medical Center. That’s when a simple blood test revealed shocking results. “I thought about death a lot. I was calling people to ask them to help take care of my family if I wasn’t going to be here anymore,” he emotionally confesses. Although Mondo loves his job as a railroad engineer, it involves on-call shifts and an erratic sleep schedule. At that time his exercise and eating habits weren’t the best either. Yet he never imagined he would have a massive, often lethal, type of heart attack called ‘the widowmaker.’ In fact, his family had been concerned about his health for awhile. “He worked so much and he didn’t take care of himself and he didn’t exercise – he was burning the candle at both ends,” shares his wife, Alison. His daughter Justice, an avid exerciser, was always encouraging him to join her at the gym, but could never quite convince him. Mondo remembers the time before he became a heart attack survivor. “I didn’t have any exercise whatsoever in my life. At that point my eating habits were just terrible,” he shares. He went to the emergency room due to his earache, but nothing was found until one of the doctors ordered some tests. Specifically blood work showed high troponin levels. Troponin is a blood protein often released in large amounts when the heart muscle has damage, sometimes by a heart attack. Heart Attack Survivor “My surgeon came in and told us that it was going to be a triple bypass – that three of the four…major arteries were clogged 100 percent,” Mondo explains. Amazingly his heart was pumping on only 10 percent blood flow. Heart surgeon, Joseph Brandl, MD, told him he survived a widowmaker heart attack. This type of heart attack happens when there is a 100 percent blockage in the critical left anterior descending artery (LAD) of the heart. Frequently the symptoms can often be mistaken for the flu. According to the Centers for Disease Control and Prevention (CDC), every 40 seconds a person in the U.S. has a heart attack. And 1 in 5 heart attacks are “silent” – meaning you can be a heart attack survivor, but not know it. For Mondo’s children, seeing their strong father struggle after heart surgery was difficult. Justice tearfully shares, “It was really hard seeing him so vulnerable. He really needed anybody’s and everybody’s help at that point.” A Heart Attack Survivor Program After leaving the hospital on January 5, 2019, he was extremely weak. On February 12, Mondo began Renown Health’s Intensive Cardiac Rehabilitation (ICR) Program called the Healthy Heart Program. This program, requiring a doctor referral, includes 12 weeks of supervised exercise along with nutrition education and stress management skills. In spite of heart disease being the leading cause of death in the U.S. – more than all cancers combined, the risk can be lessened with daily lifestyle habits. Mondo credits the ICR program with motivating him and getting his focus back on his health. He saw the team members setting an example and also caring about his health. He describes one of his favorite recipes, “In ICR Sara showed us how to make this incredible fruit salad, with jicama, watermelon, grapes, oranges, red onion, and ginger!” Of course, the recovery process was not overnight. “It did take a long time to really realize that he was going to be back to normal, that he was going to be okay and that he was going to be that strong provider for me and my children,” Alison reflects. “Mondo’s had an amazing outcome and he’s not limited in his activities at all and should hopefully have a life that’s not limited at all from heart disease as we’re monitoring everything and everything’s looking good,” reports his heart doctor Jayson Morgan, MD. Mondo describes his care experience being a heart attack survivor as life-changing. “The care teams at both Renown and ICR were incredible. There wasn’t a single person we came across who didn’t immediately become a part of the family. They truly cared for us, all of us, including the extended family that came to visit. They were informative and supportive. I felt like I created lasting bonds with so many of them, especially the gang in ICR. What amazing people.” Lynice Anderson, Director of Intensive Cardiac Rehab, Healthy Heart Program, shares,” Mondo is one of the most genuine, thoughtful and humble people I have ever met. His love for his family is palpable. His impact on me personally and our team is forever.” She acknowledges family support is key to his success, “Mondo’s family is his rock and they are his. I have never met a family that was so ‘all in’ in the support of their loved one. His new heart healthy lifestyle is modeled through his family every day.” Fighting The Good Fight Of course, Mondo may look familiar to you. That’s because he is featured in Renown Health’s “Fight The Good Fight” brand campaign. For this reason, you may have seen him in advertising working out on a treadmill, shirtless, with his open heart surgery scar in full view. When asked how he feels about showing his scar he confidently says, “I don’t mind showing it to people. I don’t. I earned that scar.” He is a proud heart attack survivor. Today, he’s grateful to be alive and takes his health commitment seriously. “Things have a different feel now. The skies and lakes are bluer and the trees greener. My family is so much more a part of my day. We go on so many more outdoor adventures, trying to incorporate a little exercise into our fun. We watch what we eat more and are trying to teach our children and loved ones about healthy choices. And I think with a few we’ve even been successful!” he observes. “Don’t take life for granted.” “Unconditional love. I get nothing but support from my family without them I wouldn’t be where I’m at. What happened to me definitely makes me a fighter for sure. I’m fighting for my life – the good fight – I think life is good,” he adds.
-
Fall Recovery Gets Patient Back to Life and Movement
Standing at the top of the stairs to the basement Sharon Sturtevant was chatting with her grandson in the kitchen. Suddenly, Sharon stumbled and fell down the stairs. “The last thing I remember was my head hitting the floor before everything went black,” she recalls. Her grandson, Oliver, quickly called 911 and paramedics arrived on the scene, taking her by ambulance to Renown Regional Medical Center where she was diagnosed with a broken collarbone and a neck fracture that would require complex surgery involving fusion of her neck. Fall Recovery Begins After her surgery, Sharon was transported to the Renown Rehabilitation Hospital and her recovery process began. Sharon smiles as she describes the rehab hospital team “They are fabulous here, I learned so much about how my body moves, and the proper way to move it. At home I wouldn’t have known what to do,” she confesses. “They set me up for success to return home and not get injured again.” At Renown Rehabilitation Hospital, different therapists coordinated a custom plan to help Sharon recover from her injuries. Ultimately, the goal of her physical therapy was to help restore and improve her strength, reduce pain and increase her mobility for stamina and balance. Physical Therapy Key to Successful Treatment of Falls “My recovery after the operation was an eye-opener,” Sharon declares. “I had no idea how much went into regaining everyday moment.” During her rehabilitation hospital stay, she had to re-learn how to swallow, go up and down stairs, as well as successfully get in and out of a wheelchair, which involved transferring her body weight safely. Due to hormonal changes after menopause women are 50% more at risk for falls than men, according to research. Sharon now has a greater awareness of how to move her body and is significantly stronger than before entering her physical rehabilitation sessions. Not everyone knows that everyday mobility is impacted by four basic skills: stepping, trunk flexibility, upright posture and weight shifting. “I don’t know how I could have gotten this far without the wonderful therapists here,” she shares. “They are so thorough. Proper alignment was encouraged helping me to walk and stand correctly. They were all so nice and patient with me,” she states. “I actually had less pain because I didn’t hurt myself moving the wrong way.” Falls Are Common Among Aging Adults As we age balance becomes more important. Unfortunately falls are common among older adults with negative quality of life effects, even fatalities. According to the Centers for Disease Control and Prevention (CDC), one in four seniors fall each year in the U.S. A comprehensive physical therapy plan for sudden falls or chronic conditions is a safe, effective alternative treatment to medication such as opioids. Today Sharon is back at home with a new banister installed on the basement stairs. As a music lover she is enjoying her musical grandchildren Oliver and Eliana who play instruments. She looks forward to attending their upcoming school concerts. Sharon remembers the staff at Renown Rehabilitation Hospital fondly, “They were unfailingly patient, supportive, informative and understanding.” Her advice to those unexpectedly finding themselves in the rehabilitation hospital is, “Listen to your therapists carefully and follow their instructions.”
Read More About Fall Recovery Gets Patient Back to Life and Movement
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
The Road to Recovery Close to Home
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.
-
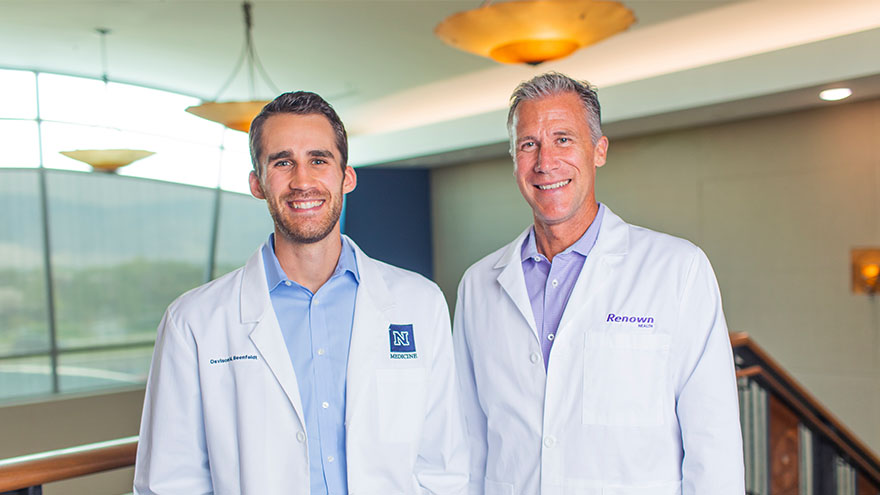
A Family's Legacy
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school