Search
-
3D vs Whole Breast Ultrasound Which is Right for You
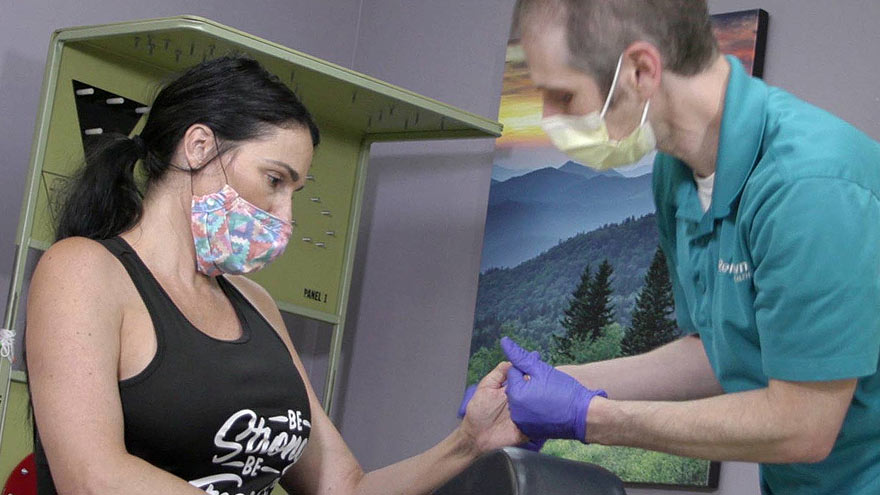
Breast cancer is the leading cause of cancer deaths in women in the U.S. That’s why early detection is so important. Dr. George Krakora, a radiologist with Renown Institute for Cancer, explains what to watch for and how new technology can lead to early detection. Most women know the importance of breast health and staying current with annual breast exams, but may not know that both screening guidelines and technology is evolving. So we asked George Krakora, MD, a radiologist for the Renown Institute for Cancer, what every woman should know about breast cancer detection and which screening method is right for them. First off, when should women start getting breast exams? Generally, women should start getting breast exams using mammography or ultrasound after they turn 40 years old. But we also want women ages 18 to 39 to talk to their primary care provider and ask for what’s called a formal risk assessment to see if screening is needed sooner. And you want to make sure your care provider is giving you a breast exam starting at age 25. It’s also a good idea to be familiar with how your breasts look and feel so you can report any changes to your care provider. What are the risk factors for breast cancer? Are there any preventive steps women can take? There a few risk factors you can’t control, like your age, family history of breast or other cancers, and if you have dense breast tissue. Your risk for breast cancer increases as you get older, and most breast cancers are diagnosed after age 50. Knowing your family history is important because a history of cancer and shared lifestyle can raise your risk. Your breast density can also increase your risk: Women with high breast density are four-to-five times more likely to get breast cancer than women with low breast density. But the good news is there are quite a few things you can do to prevent breast cancer, like not smoking, watching your alcohol intake, and maintaining a healthy weight with good diet and exercise. There are a lot of newer screenings out today. What is the difference between 2-D and 3-D mammography? In a 2-D mammogram, the tech takes X-rays of the breast. These pictures can show the radiologist if there are any lumps or tumors you might not be able to feel. In 3-D mammography, the process is largely the same but more X-rays are taken and it takes a few seconds longer for each image. This kind of exam detects 41 percent more cancers and reduces the number of false-positive results given to patients. This improvement in technology is great for both patients and their care providers. 3-D mammography provides better images of the breast, which allow doctors to more clearly diagnose and avoid false positives, especially in women with dense breast tissue. And what about a whole breast ultrasound. What is that? A whole breast ultrasound uses sound waves to detect cancerous tumors in the breast without using any radiation — it’s an ultrasound just like pregnant women get to check up on their baby. And the exam only takes about 20 minutes. We recommend these exams for patients whose mammograms have shown that they have dense breast tissue. Dense breast tissue can make it harder for doctors to see any abnormalities, lumps or tumors in a mammogram, so this technology ensures better early detection.
Read More About 3D vs Whole Breast Ultrasound Which is Right for You
-
Foods to Avoid When Taking Heart Medications
Did you know certain medications can interact with everyday food and drink? We asked Pharmacy Manager Adam Porath how to take these important medications safely. One in five Americans between the ages of 40 and 75 are currently taking a statin drug to reduce their cholesterol level or to prevent atherosclerosis (hardening of the arteries). Many others also take anticoagulants (blood thinners) to prevent blood clots from forming, which can increase the risk of stroke. Adam Porath, pharmacy manager with the Renown Institute for Heart and Vascular Health’s Anticoagulation Program, explains how to safely take these medications. What is a statin? A statin is a drug that can lower cholesterol by helping your body absorb cholesterol or by blocking a substance your body needs to make it. The American Heart Association cites a global study reporting the benefit of statins to help reduce heart attacks and strokes. Common statins include atorvastatin (Lipitor), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor). Which foods or drinks should be avoided while taking statin drugs? Grapefruit juice is the only food or drink that has a direct interaction with statins. Statins do not directly interact with any food but people taking statins should moderate their intake of saturated fats to help lower their LDL cholesterol and overall risk of cardiovascular disease. What is a blood thinning drug? Blood thinning drugs, such as warfarin, rivaroxaban (Xarelto), apixiban (Eliquis), dabigatran (Pradaxa) and edoxaban (Savaysa), are used to prevent stroke. Which foods or drugs should be avoided while taking blood thinning drugs? If taking warfarin, alcohol and cranberries (including juice) should be avoided. Patients taking warfarin should be aware of foods that contain Vitamin K (green leafy vegetables) and try to maintain a consistent diet of these foods. Warfarin interacts with many over the counter and prescription medications. Patients should consult a pharmacist when starting, stopping, or changing doses of any medication when taking warfarin. Also, patients taking any blood thinning medication should avoid over-the-counter pain relievers (i.e. aspirin, ibuprofen, etc.) How do I know whether to take my medication with food or not? Consulting with a pharmacist is the best resource to determine if a medication should be taken with or without food. In general, all statins and blood thinners can be taken with or without food. The only exception is Xarelto (rivaroxaban), which should be taken with the largest meal of the day If you are a Renown patient you can also review your prescriptions online, request a refill or ask a question via MyChart. With MyChart, you can access all your healthcare information securely 24/7.
Read More About Foods to Avoid When Taking Heart Medications
-
Cervical Cancer Screenings Can Reduce Risk of Cancer
According to the American Cancer Society, approximately 14,100 new cases of invasive cervical cancer will be diagnosed, and 4,280 women will die from cervical cancer. However, cervical cancer is preventable with regular screening tests and the HPV vaccine. It’s important to note that medical advances have allowed progress in diagnosing and treating cervical cancer. While it used to be one of the most common causes of cancer death for American women, the incidence of death has significantly declined. What to Know About the HPV Vaccine HPV vaccination is the best way to prevent cervical cancer and is recommended for all youth starting as early as age 9, or for teens and adults up to age 45 who didn’t start or finish the series. In Nevada, only 50.1% of teens ages 13-17 have been vaccinated for HPV. There are 13 types of HPV, and the vaccine Gardasil 9 protects against 9 of those HPV strains, greatly reducing the incidence of cervical cancer among vaccinated individuals. What to Know About Cervical Cancer Screenings The CDC says the most important thing you can do to help prevent cervical cancer is to have regular screening tests starting at age 21. And there are two common tests that can detect early stages of cervical cancer (or precancer) and improve health outcomes. The pap test (or pap smear). This screening looks for precancers. Women should begin getting pap smears when they’re 21. The human papillomavirus (HPV) test looks for the virus that can cause these cell changes. Cervical Cancer Screening Schedule The American Cancer Society offers the following guidelines for screenings: All women should begin cervical cancer screening at 21. Women between 21 and 29 should have a pap test every three years. Beginning at 30, the preferred way to screen is with a pap test combined with an HPV test every five years. This is called co-testing and should continue until age 65. A pap test (or pap smear) is performed during a regular screening appointment to look for precancers, cell changes on the cervix that might become cervical cancer if they are not evaluated or appropriately treated. Typically outpatient procedures can reduce the risk of long-term health impacts that prevent pre-cancerous cells from becoming cancer cells. Women over 65 who have had regular screenings in the previous ten years should stop cervical cancer screening as long as they haven’t had any severe precancers found in the last 20 years. How to Get Screened Request an appointment with your primary care physician or OBGYN to schedule a screening.
Read More About Cervical Cancer Screenings Can Reduce Risk of Cancer
-
Why are Annual Exams & Routine Screenings Important?
March is Colorectal Cancer Awareness Month, and we want you to receive the best preventative care possible. Early detection can help prevent serious illness, yet many people still choose to skip their annual exams and routine screenings. Bonnie Ferrara, MD, MPH, Section Chief for Primary Care at Renown Medical Group, further explains the importance of this simple, easy way to stay healthy. Why are annual exams so important? The benefits of early detection and prevention to save lives and reduce the impacts of disease have been proven. These exams are the perfect opportunity to get your health questions answered. “This is your chance to sit down with your provider and talk about your overall health and your family’s health history as well as your concerns for the future,” says Bonnie Ferrara, M.D., family medicine. “It’s the opportunity for your provider to talk with you about your lifestyle, tobacco use, exercise and alcohol use, all of which make a difference in your future longevity.” The annual wellness exam is also an ideal time for most adult patients to discuss health screenings. In addition, these visits are the perfect time to address issues that may not directly relate to a particular medical problem or immediate illness. A good rule of thumb is to schedule these appointments around your birthday each year to make sure you and your provider are both updated on your care. Why would you need an annual exam if you aren’t feeling sick? According to Dr. Ferrara, seeing your care provider when you aren’t sick is one of the best times. “It is better if you try to arrange this visit when you are not feeling ill,” she says. “It is an opportunity to talk about wellness. Not only how to contribute to your wellness but also the changes that you can make that will make huge dividends in the future for your wellness. In addition, it allows us to do some education about what to expect in the coming years as far as your health and lifestyle changes.” What can you expect at an annual exam? Annual exams usually check your: History – lifestyle behaviors, health concerns, vaccination status, family medical history Vitals – blood pressure, heart rate, respiration rate and temperature General appearance – your care provider can find out a lot about you just by watching and talking to you Dr. Ferrara adds, “If this is a Medicare annual wellness exam, it is an opportunity to talk to your provider about depression and dementia as well as be tested for those.” You can also leverage your annual exam to speak to your provider about managing your chronic health problems. "As a provider, these visits give us the opportunity to hear how the medications and lifestyle changes we have recommended are working and if you are having problems with these, we have the opportunity to make suggestions of how to do things better for the future," Dr. Ferrara.
Read More About Why are Annual Exams & Routine Screenings Important?
-
Stroke Survival as a Warrior – Kimi's Story
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Women and Stroke Surprising Signs to Know
Stroke is unfortunately common, with 1 in 5 American women experiencing it each year. When it comes to a stroke the phrase “time is brain” speaks to the urgency of getting rapid care. In fact, a woman may lose nearly 2 million neurons per minute of oxygen loss to the brain. The Renown Health Comprehensive Stroke Center experts share the importance of timely treatment and how stroke symptoms can differ in women. Women and Stroke – Surprising Symptoms Each year stroke affects more women than men. Even more concerning, women are less likely to recover from a stroke. The following non-traditional, less common, warning signs can be common in women: Hiccups with chest pain Sudden disorientation, drowsiness, confusion or a general altered mental status Nausea or vomiting A sudden headache that feels like the ‘worst headache of your life’ Unusual chest pain (especially with hiccups) Body numbness or weakness, such as an arm or leg suddenly ‘falling asleep’ Fainting or loss of consciousness Stroke Diagnosis The first step is neuroimaging by CT scan. This allows for rapid identification of any bleed, and also assists in determining candidacy for the early clot busting medication. MRI brain imaging is much higher resolution, and can better determine the core stroke size, assisting in prognosis and recovery. Since strokes have several different origins, an inpatient workup is essential to determine the underlying cause. Whether the stroke is secondary to plaque in the large vessels, clots being thrown in the setting of atrial fibrillation (an abnormal heart rhythm), or small vessel disease from years of uncontrolled vascular risk factors (high blood pressure, smoking, high cholesterol, diabetes), determining the cause is essential to implementing a management plan to reduce risk for further strokes. Quick Treatment for Stroke is Key Early recognition of stroke symptoms and seeking prompt attention is paramount. There are interventions that can be instituted to minimize the stroke and increase likelihood of recovery, but only if a patient presents to the hospital early. A clot busting medication, called tPA, can be given to patients with stroke if given within 4-5 hours from time of onset. Renown Regional Health Center is designated as a Comprehensive Stroke Center, the highest level of stroke certification available. To earn the designation of comprehensive stroke center, a hospital has to meet stringent requirements, including biannual on-site evaluations. This includes care for ischemic stroke patients (lack of blood flow), hemorrhagic stroke patients (bleeds), and determining the underlying cause to guide secondary stroke management prevention. Stroke Symptoms Remember “B.E.F.A.S.T.” to recognize the symptoms of a stroke below: B – Balance Being off balance or dizzy, is common. E – Eyes An eyesight change such as blurring or double vision may occur. F – Face droop One side of the face, or lip, droops A – Arm weakness Does one arm drift down? S – Speech Talking may slur or sound strange. T – Time Time to call 911. Call an ambulance immediately if you or anyone else, experiences any of these symptoms.
-
8 Important Health Screenings for Men
Unfortunately, men are less likely to visit their doctor for exams, screenings, and consults than women. So with the help of Bonnie Ferrara, MD of Renown Health, we've put together a list of eight screenings to help men stay on top of their health game. 1. Blood Pressure Tests Ages 20+ Blood Pressure tests measure the pressure in your arteries as your heart pumps. Biennial (every two years) checks are recommended if you have normal blood pressure or more frequently if you have high blood pressure (hypertension) or low blood pressure (hypotension). The United States Preventative Services Taskforce cites normal blood pressure below 120 systolic (top number) and 80 diastolic (bottom number). 2. Cholesterol Screening Ages 20+ High levels of cholesterol increase your risk of stroke and heart disease. A simple blood test will help your healthcare provider determine your numbers and if you're at risk. If you have a family history of diabetes or heart disease, you may need yearly screenings. But, again, your doctor can provide the best course of action.
-
Avoid Heat Exhaustion With This Simple Checklist
Young children under 4 and adults over 65 are especially vulnerable to heat exhaustion. Avoid heat exhaustion this summer with some expert tips. Northern Nevada summers can be downright hot, and although the balmy temperatures can feel great, they may cause heat-related illness, also known as heat exhaustion. Infants and children under 4 and adults over 65 are particularly vulnerable to heat exhaustion because their bodies adjust to heat more slowly. Without proper intervention, heat exhaustion can progress to heat stroke, which can damage the brain and other vital organs and even cause death. The Warning Signs of Heat Exhaustion Heavy sweating Elevation of body temperature Paleness Muscle cramps Tiredness, weakness, dizziness Headache Fainting Nausea or vomiting Cool and moist skin Fast and weak pulse Fast and shallow breathing Heat stroke happens when the body’s temperature rises rapidly and the body loses its ability to sweat. The Symptoms of Heat Stroke Body temperatures rising to 106 degrees or higher within 10 to 15 minutes Red, hot and dry skin (no sweating) Rapid, strong pulse Throbbing headache Dizziness or nausea Prevention and Treatment Make sure your air conditioner works Stay indoors and drink plenty of fluids Limit strenuous outdoor activities to mornings and evenings Drink plenty of water throughout the day Avoid caffeine and alcohol Do outdoor activities in the shade and wear light, loose clothing Take plenty of breaks and drape a wet bandanna around your shoulders to cool down If you suspect you or someone else is headed toward heat exhaustion or heat stroke, call 911 immediately.
Read More About Avoid Heat Exhaustion With This Simple Checklist
-
3 Healthcare Musts for Millennials
Many millennials are fortunate to have good health, but it’s important to be prepared for your next doctor’s visit. Here are three things that millennials should stay on top of for tracking and maintaining their health. For many millennials, doctor visits and preventive healthcare fall by the wayside. Alison Lynch, MD, a family medicine provider with Renown Medical Group says there are a few key things you can do now to set yourself up for a healthy future. 1. Establish with a Primary Care Provider Millennials are more likely to go to urgent care or consult the internet when a healthcare issue arises. While these are helpful tools, here’s a better one: a primary care provider. The benefit of establishing with a primary care provider is that your medical records, history and a baseline for your health will be documented. That means that when a problem or question comes up, your doctor will already have helpful information on file and can help you navigate your needs. Having a primary care provider is often required for prescription refills and referrals to a specialist. By establishing now, you’ll be able to get what you need in the future much faster. Make an Appointment Today 2. Protect Yourself and Your Community There are a few vaccinations and screenings that Dr. Lynch recommends for millennials. Flu Shots: These are available every year and are recommended for protecting not only yourself against the flu but also others you may come into contact with. Flu shots are usually available from August through December through your healthcare provider, pharmacies and pop-up events. Tetanus or Tdap: Most people receive a tetanus shot as a child, but it’s recommended that everyone get a booster every 10 years. If you are overdue, talk to your primary care provider or pharmacist about getting updated. Pap smear: If you’re a woman, a pap smear is recommended every three years in your 20s and every five years in your 30s. HPV vaccine: This vaccine helps prevent the virus that causes cervical cancer as well as the majority of head and neck cancers and warts. The HPV vaccine is recommended for all genders up until age 45. STD screening: Consider an STI/STD screening if you’re sexually active.
-
Lung Cancer Screening and Early Detection
Lung cancer is the leading cause of cancer deaths in both men and women in the U.S. The good news is the five-year survival rate increases dramatically if lung cancer is treated before spreading to other parts of the body. Julie Locken, MD, of Renown Health Imaging, explains more. What are the signs and symptoms of lung cancer? As you might expect, most lung cancer symptoms appear in the chest and can affect your breathing. Watch for signs such as: Persistent cough Constant chest pain Shortness of breath Wheezing Bloody or rust-colored phlegm Hoarseness Swelling of the neck Pain or weakness in the shoulder, arm or hand Recurring pneumonia, bronchitis or other lung infections Loss of appetite and loss of weight can also be signs of lung cancer That said, there are usually no symptoms in the early stages of lung cancer, which means getting screened can truly be a lifesaver. If you have a history of smoking, you should get screened as a precaution. What are the risk factors of lung cancer? Around 80% of lung cancer cases stem from a history of smoking tobacco. But there are other known causes, such as secondhand smoke, radon, asbestos and diesel exhaust. It’s important to do what you can to eliminate exposure to all of these to reduce your lung cancer risk. People with an immediate relative – a parent, sibling or child – diagnosed with lung cancer and people between 50 and 80 years old are also at higher risk and may need to consider screening. People who are at the highest risk are those with a history of smoking tobacco, particularly smokers who averaged one pack of cigarettes per day for 20 years or more, as well as former heavy smokers who quit in the last 15 years.
-
Lyme Disease: 3 Things You Should Know
Approximately 476,000 Americans are diagnosed and treated for Lyme disease every year. Lyme disease is an infection that is transmitted to humans through the bite of infected black-legged or “deer” tick. It’s the most common and fastest-growing vector-borne disease in the United States. This bacterial infection, if left untreated, can cause serious pain, fatigue and other crippling symptoms. Keeping an eye out for early signs of Lyme disease, implementing prevention techniques and understanding testing and treatment options can go a long way in maintaining your health. We consulted with Peter O’Reilly, PA-C at Renown Medical Group – South Carson to learn more. 1. Recognizing the Signs of Lyme Disease Lyme disease is extremely easy to misdiagnose, given that most of its early signs and symptoms mimic those of other conditions, such as COVID-19. Common Lyme Disease symptoms include: Fever Chills Joint or muscle pain Swollen glands Extreme fatigue Headache The primary initial symptom that occurs in about 80 percent of Lyme disease cases is a “bulls-eye” rash that spreads around the site of the tick bite – called “erythema migrans.” Tick bites can be hard to find and not everyone gets the classic bullseye rash, making Lyme disease difficult to self-diagnose. O’Reilly suggests talking to either your primary care doctor or infection doctor as soon as possible if you’re concerned about Lyme disease.
-
Keeping Kids Safe on Halloween
Halloween is around the corner. So while you're prepping pumpkins for carving, putting together creative costumes and coordinating trick-or-treating plans, safety is one more detail to remember. Masks, haunted houses, witches, ghosts and ghouls — it all spells Halloween, and what could be more frighteningly fun, right? For children, however, Halloween can indeed be frightening and not so fun. According to Dr. Kristina Deeter, Physician-in-Chief of Renown Children’s Hospital and Chair of Pediatrics for the University of Nevada, Reno School of Medicine, it is common for younger children to express Halloween fears — being afraid of monsters, the dark or really anything out of the norm. “It's normal for children to struggle with separating reality from fantasy,” she explains. For children who fall into this category, the month of October can be traumatizing. Halloween may not come until the end of the month. Still, in the weeks building up to the spookiest night of the year, little ones are bombarded on all sides with decorations — mummies, skeletons, coffins, vampires, you name it. For a child with a blossoming imagination who, as Dr. Deeter said, is still learning to differentiate real from pretend, this can cause additional fears and anxieties. In commemoration of Halloween Safety Month, Dr. Deeter shares safety tips for the spooky holiday from the American Academy of Pediatrics: Dressing Up & Heading Out Plan costumes that are bright and reflective. Ensure shoes fit well and that costumes are short enough to prevent tripping, tangling or coming into contact with flames. Consider adding reflective tape or striping to costumes and trick-or-treat bags and baskets for greater visibility. Masks can limit or block eyesight. Instead, consider non-toxic makeup and hats, which should fit properly to prevent them from sliding over the eyes. Test makeup ahead of time on a small patch of skin to test for allergies before full application. When shopping for costumes, wigs and accessories, look for and purchase those with a label clearly indicating they are flame resistant. If a sword, cane or stick is a part of your child's costume, make sure it is not sharp or long. A child may be easily hurt by these accessories if he stumbles or trips. Do not use decorative contact lenses without an eye examination and a prescription from an eye care professional. While the packaging on decorative lenses will often make claims such as "one size fits all," or "no need to see an eye specialist," obtaining decorative contact lenses without a prescription is both dangerous and illegal. This can cause pain, inflammation, serious eye disorders and infections, which may lead to permanent vision loss. Review with children how to call 9-1-1 (or their local emergency number) if they ever have an emergency or become lost. Carving Pumpkins Leave the carving to the grownups. Have children draw the pumpkin design with markers, but keep knives away. Consider using a flashlight or glow stick instead of a candle to light your pumpkin. If you do use a candle, a votive candle is safest. Candlelit pumpkins should be placed on a sturdy table, away from curtains and other flammable objects, and not on a porch or any path where visitors may pass close by. They should never be left unattended. Prepping Your Home Keep your entryway safe for trick-or-treaters by removing all items from the porch or front yard that a child could trip over, like garden hoses, toys, bikes and lawn decorations. To ensure visibility, check outdoor lights and replace burned-out bulbs. Sweep leaves (or snow) from sidewalks and steps. If there are dogs in the home, take steps to ensure they don't jump on trick-or-treaters. Hunting for Treats Young children should always be accompanied by a parent or responsible adult. Give each child and adult a flashlight (with fresh batteries). If older children are heading out to trick-or-treat alone, plan and review a route you can agree on, as well as a specific time they are supposed to return home. Only visit homes with a lit porch light. Never enter a home or a car for a treat. Notify law enforcement authorities of any suspicious or unlawful activity immediately. Since pedestrian injuries are the most common injuries to children on Halloween, remind youngsters to take crosswalk safety precautions. For more key tips regarding Halloween safety for your young trick-or-treaters, visit our partners at Safe Kids Worldwide for a variety of spooky safety resources.