Search
-
-
12Dec
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. For scheduling/cancellation questions, contact 775-982-RSVP (7787) For questions about workshop content, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
-
15Aug
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. For scheduling/cancellation questions, contact 775-982-RSVP (7787) For questions about workshop content, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
-
20Jun
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. For scheduling/cancellation questions, contact 775-982-RSVP (7787) For questions about workshop content, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
-
10Oct
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. For scheduling/cancellation questions, contact 775-982-RSVP (7787) For questions about workshop content, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
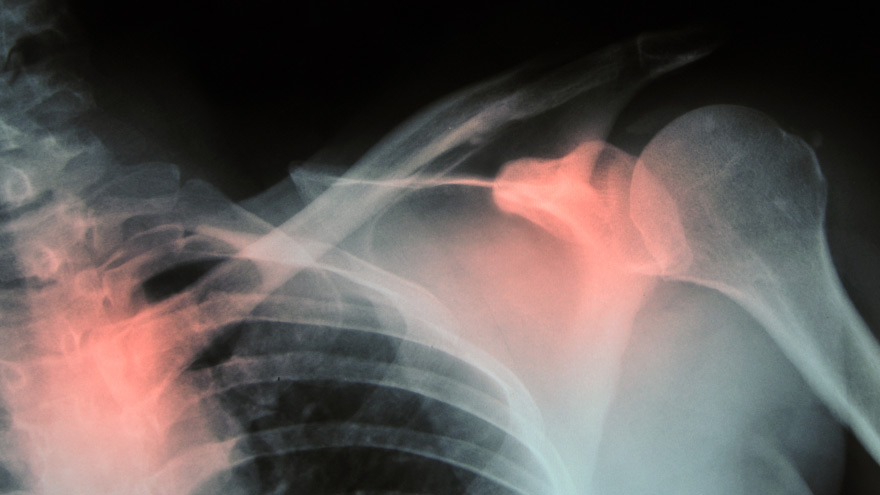
Prevent Osteoporosis: Take Control of Your Bone Health Today
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
Here's How to Commemorate National Healthcare Decision Day
National Healthcare Decision Day is forthcoming. Here’s an easy and free way to commemorate the occasion: openly discussing how we want to be cared for at the end of our lives. Join Renown Health’s experts at a workshop about making decisions about an advance directive. Among the random national holidays, this one has significance: April 16 is National Healthcare Decision Day. And experts agree that the best time to discuss your views about end-of-life care and to learn what choices are available is before a life-limiting illness or crisis occurs. By preparing in advance, you can help reduce the doubt and anxiety related to decision making for your family if you cannot speak for yourself. “Completing your advance directive is a gift you give your family,” says Mary-Ann Brown, RN, MSN, director of Palliative Care. “The stress associated with these difficult decisions is decreased if everyone knows what is important to you and what you want the end of life.” What Are Advance Directives? An advance directive is a document that states your choices about medical treatment and names another person to make medical decisions on your behalf if you are unable to. This document allows you to make legally valid decisions about future medical care. Find more information about advance directives and the form online. The Conversation The first step in completing an Advance Directive is to think about what’s important to you and talk to your loved ones. The Conversation Project provides helpful tools to guide you and your family through this challenging topic. Getting this information together will help you fill out and complete your advance directives. Some things to consider and discuss with your family include: When you think about the last phase of your life, what’s most important to you? Who do you want involved in your care? Who should make decisions on your behalf if you’re not able to? Where do you want or not want to receive care? Are there specific treatments you would or would not want? Complete Your Advance Directive Planning In order to complete an advance directive, you will need either two witnesses or a notary to sign the form. Be sure to note restrictions on the witness process. When an advance directive is complete, you should keep the original. Copies should be given to your agent named in the form, your family, your doctor(s) and the location that you receive care. Renown Health offers four advance directive workshops every month to cover the details of filling out this document. A healthcare team is available to answer questions and work through the process with you. A notary is also present to finalize the process, which means you can complete your advanced directives during this workshop. Find the workshop by calling 775-982-RSVP for more information. Advance Care Planning Workshop April 17, 1-2:30 p.m. | Free Join Renown Health’s experts for a workshop about making decisions regarding end-of-life care. You will learn how to fill out an advance directive, receive one-on-one assistance and have your documents signed by a notary. Workshops are typically held several times each month. To RSVP, call 775-982-7787
Read More About Here's How to Commemorate National Healthcare Decision Day
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Stroke Survival as a Warrior – Kimi's Story
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Getting to Know Renown's Canine Companions
A slobbery kiss, a wagging tail, a judgement-free smile. There are few things better than the love and attention of a canine companion. At Renown Health, we have a loyal and playful group of pet therapy teams. This volunteer program uses animal-assisted interactions (AAI) and animal-assisted therapy (AAT) to provide comfort, reduce boredom, increase social interactions, improve mood, boost general well-being and – perhaps most importantly – bring smiles to our patients’ faces. Benefits of AAT & AAI: Lowers blood pressure and heart rate by relieving anxiety Helps in pain management Eases feelings of depression, loneliness, boredom and isolation Stimulates communication Encourages physical activity For more information about the program, a complete list of our teams or to get involved, click here. Meet Keno and Linda Linda, Keno’s human, has volunteered as one-half of a therapy dog team for more than 14 years. Keno is her third Newfoundland, and he is a sweet and cuddly 2-year-old pup, who, according to Linds, thinks is a lap dog. “My mother was in assisted living for almost 10 years, and I saw what an impact a therapy dog can have,” Linda said. When she moved to Reno from Portland six years ago, she immediately contacted Renown. A Memory the Stands Out: A patient in the ICU was not responsive because of oxygen deprivation due to almost drowning. Linda and Keno went into the patient’s room at his physical therapist’s request, and the therapist asked the patient to reach out and pet the dog. After the third request, he moved his hand toward the dog, and his mother burst into tears. It was the first time the patient had moved since his accident. Linda and Keno went back several days in a row, and soon the patient was talking, sitting up and eating on his own. Meet Madi and Clark Madi, Clark’s human, is an employee at Renown, and Clark made it a family affair by joining the team in Sept. 2021. Clark is a unique pup with an amazing demeanor who adores everyone as much as they adore him. He is a hardworking Goldendoodle who loves to be a goofball at home when he’s off the clock. Why They Became a Therapy Dog Team: Madi was inspired to get Clark trained as a therapy dog because, as an employee at Renown, she was always so happy to see dogs walking around, and she knew that I wanted to provide that same relief to others. Her favorite thing about being a Renown volunteer is the joy it spreads to those working and the patients they are caring for. Meet Richard and Raven Raven is a four old Belgian Malinois who has been working as a therapy dog for two and a half years. She is calm, friendly and loves having her tummy rubbed. “The therapy dog teams are just one little part of Fighting the Good Fight,” Raven’s human Richard said. A Memory that Stands Out: Raven and Richard were assigned to the Sierra oncology ward one shift and visited a woman who had a picture of her dog displayed next to her bed. Raven immediately went to the bedside and the patient started petting her. As she spent more time petting Raven, Richard could see the stress disappearing from her face. He later learned that it was the patient’s first chemotherapy infusion, and Raven gave her the peace and the strength she needed to face the chemotherapy head-on. Meet Savannah and Hallie Hallie and Savannah’s journey as a therapy dog team began in 2017 at the Morgan Stanley Children’s Hospital in New York and has also taken them to San Francisco General Hospital and Stanford Hospital. The duo moved to Reno in 2020 and immediately joined the Renown Pet Therapy Program. A friend, energetic and cuddly American Cocker Spaniel, Hallie especially loves spending time with the young children at the hospital. A Memory That Stands Out: Savannah remembers one visit to a patient in the Children’s Emergency Room who was struggling with suicidal thoughts. Having struggled with mental health herself, Savannah felt a deep connection to the patient and a need to help. She recalls placing Hallie on the patient’s bed a seeing a “very small hint of a smile.” Savannah later learned that the Renown nurses hadn’t seen the patient smile in days. It was that moment that made Savannah realize what a profound impact Hallie can have on patients. Meet Chivas and Donna Chivas was a McNab/Border Collie mix who volunteered at Renown with her human Donna for two years. With help from Donna, Chivas was a master at reading situations in the hospital and reacting accordingly. For example, if a patient was afraid of dogs, she would sit with her back to the person so she didn’t come off as threatening. Contrarily, she would lie down on the floor when playing with young children to let them pet her on their level. Why They Became a Pet Therapy Team: This dynamic duo started out as a member of a local pet therapy group. During the height of the COVID-19 shutdown, they participated in outdoor pet therapy parades for various hospitals in the area. Donna and Chivas met Renown Volunteer Coordinator Wendy Peuket at one of the parades and she inspired Donna to pursue becoming a registered therapy dog team for Renown's Therapy Dog Program. Chivas sadly passed away unexpectedly in early December 2021, and the world is a whole lot dimmer place without Chivas’ light shining brightly.
-
Perfect Peanut Butter and Pumpkin Puppy Treats
This holiday season, don't forget about your favorite furry friends by baking these easy, AKC-approved dog treats. Simple ingredients and quick baking times make this the ideal last-minute surprise. Make it a gift by picking up affordable canisters (usually abundant at dollar and thrift stores) and filling them with homemade treats. It makes the merriest, pet-friendly gift of the season!
Read More About Perfect Peanut Butter and Pumpkin Puppy Treats
-
Bone Fractures in Children Honest Expert Advice
Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis, answers some common questions about bone fractures. Is there a difference between broken bones and fractures? No, these are two different names for the same injury. Of course the common term is a broken bone. Using either name will describe your concerns. Medical personnel typically describe a broken bone as a fracture to a specific bone. For example, a broken wrist is also a fractured distal radius. To clarify, this describes the injured bone and the precise location. How do I know if my child has broken their bone? Many times children will fall and complain of their arm or leg hurting. In most cases the pain goes away and the child will return to their activities. When there is a deformity to the limb (curve in arm) and the child is complaining of pain, it is probably a fracture. If the arm or leg looks straight, look to see if there is any swelling or bruising. Both are signs of a possible fracture. Finally, if the limb looks normal but the child continues to complain, gently push on the bone. Likewise if it causes the same pain, then they likely have a fracture and should have an x-ray. My child fractured their growth plate, what does this mean? Growth comes from this area of the bone. In detail, these are located all over the body but typically at the end of the bones. With this in mind, fractures to these areas can result in the bone growing abnormally. Because of potential shortening of the arm or leg, or bones growing crooked, it is important to follow fractures closely (up to 1-2 years or longer). It is better to identify a problem early. Small problems can be treated with small surgeries. What if the bones of the x-ray do not line up? Because children are growing, unlike adults, their bones will remodel and straighten with growth. The amount of remodeling occurring depends on a child’s age, the bone fractured and the location. In many cases an angled bone will grow straight over the course of a year. For this reason, someone with experience in caring for children needs to follow bone growth. How long does it take fractures to heal? Factors deciding when a cast can come off include: Child’s age. Bone fractured. Fracture location. Young children heal faster than teens, teens heal faster than young adults, who heal faster than older adults. In young children most fractures heal in 4-6 weeks. However, teens generally take 6 weeks to heal, and adults can take much longer. Although your child is out of their cast, it may not be healed completely to return to all activities. Placing a splint is during this time is common. This typically gives them added protection for several weeks after their cast is removed - in case they forget their limitations. What if my child is still limping? Whether a child is in a walking or non-weight bearing cast, removing it often leaves them stiff and sore. Therefore many children will walk as though they still have a cast in place. In most cases this resolves in about three weeks. Regardless, if your child is still limping or walking abnormally after three weeks, contact the treating doctor. They may benefit from physical therapy or a repeat evaluation. (This article was original published in the July 2019 issue of South Reno Kids & Sports.)
Read More About Bone Fractures in Children Honest Expert Advice