Search
-
Early Onset of Puberty in Girls on the Rise
Many factors are contributing to the rise of early onset puberty in girls. Learn what they are below and how you can support your daughter. The number of girls experiencing early puberty has increased dramatically over the last few years and continues to grow. More and more girls in the U.S. are starting to show signs of development before the age of 8. Recent studies show that up to 10 percent of Caucasian girls and 23 percent of African American girls are showing signs of puberty by age 7. What’s Contributing to Early Puberty in Girls? Determining the exact cause is difficult. But experts agree that several factors may be contributing to these growing numbers. Increasing rates of childhood overweight and obesity. Excess body fat alters the levels of hormones responsible for the acceleration of pubertal timing. Physical inactivity may decrease melatonin levels, which can also trigger pubertal development. Increased animal protein intake. Higher total protein, animal protein and meat intake in children ages 3 to 7 have been associated with earlier onset of menstruation. High protein intake elevates IGF-1 levels and promotes growth, which could accelerate the onset of puberty. Poor diet. Children with lower-nutrient diets tend to enter puberty earlier. A diet rich in processed foods and meats, dairy, and fast food is disruptive to normal physical development. Exposure to EDCs (endocrine-disrupting chemicals). EDCs are synthetic chemicals found in plastics, pesticides, fuels and other industrial chemicals that inhibit or alter the action of natural hormones. Because EDCs accumulate in the fatty tissues of animals, animal foods contain higher levels of these chemicals than plant foods. Exposure to BPA (bisphenol A). BPA is an industrial petrochemical found in a variety of products including plastics, tin-can linings and even cash register receipts. Because it acts as a synthetic estrogen it may speed up pubertal development. Soy products. Soy contain isoflavones which are converted to phytoestregens in the body, and are similar to the hormone estrogen, Dr. Chelsea Wicks says. “Soy consumed from natural food sources is likely safe and will not cause abnormal hormones levels. However, when consumed in large amounts, such as with soy supplements or in more processed foods, there have been links to chronic medical problems due to elevated estrogen levels. I feel a good answer to this is to continue working on eating fresh foods and trying to avoid the processed, packaged foods as this will be best for overall general nutrition as well,” she adds. What You Can Do While some genetic factors play a role in the early onset of puberty, parents can help lessen environmental causes of the condition. Encourage and help your child to maintain a healthy weight with proper nutrition and exercise. Avoid exposure to hormones such as estrogen and testosterone that may be found in hair products, medications and nutritional supplements. Avoid exposure to EDCs and BPA. Offer your child a diet centered around whole plant foods rather than animal foods, which will help keep protein intake within a safe range and reduce consumption of EDCs. Create a supportive environment for your daughter. Avoid commenting on her appearance and instead focus on her achievements, academic successes or artistic talents. Speak to her openly and honestly about the physical changes she’s experiencing — that although these changes are normal, she’s simply developing early — and that ultimately her peers will undergo the same changes. Encourage your daughter to continue participating in social activities and pursuing her interests, and reassure her you are always open to discuss any questions or worries. If you are concerned that your child may be going through these changes before expected, speak with your pediatrician. Sources: Early Puberty: Causes and Consequences When Is Puberty Too Early? Precocious Puberty (Early Puberty) Precocious Puberty
-
Stroke Survival as a Warrior – Kimi's Story
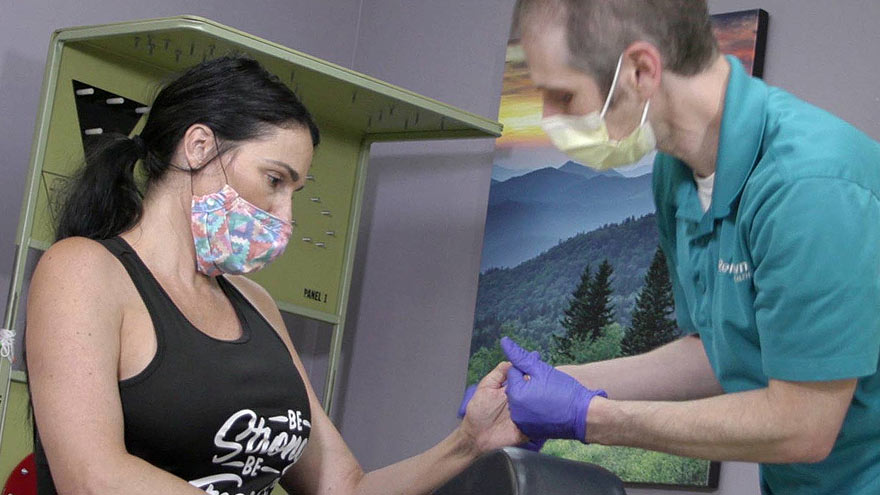
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Teens and Social Media: When Is it Too Much?
Dr. Max J. Coppes, Physician-in-Chief Renown Children’s Hospital, and Nell J. Redfield Chair of Pediatrics, UNR Med, talks about how much is too much when it comes to teens and social media. Social apps (Facebook, Instagram, Twitter, WhatsApp, Snapchat, TikTok, etc.) have become an integral part of most people’s lives. In contrast to traditional media — where one source goes to many receivers — social media operates in a dialogic transmission system. Many sources interact, sometimes simultaneously, with many receivers and provide for superior interactivity between its users. Not surprisingly, it also plays a significant role in our children’s lives once they are old enough to understand how to access and use these apps. On average, children start exploring social media at around ages 10 to 12. They rapidly discover that electronic communication allows for unique and personalized ways to make and keep friendships. They also use it to develop and expand family ties, get help with homework, share music, art, and experiences, and learn and discover the world. Social Media and Teens Surveys suggest that more than 90 percent of teenagers use social media. Additionally, approximately 75 percent have at least one active profile by age 17. Access to social media is greatly facilitated because more than two-thirds of teens have their own mobile devices with internet capabilities, a substantial change relative to previous generations. The use of social apps can have many positive aspects. But we now also recognize that it can also have negative impacts. The use of hazardous sites or the inherent risks of using social media (identity theft, being hacked, cyber-bullying, etc.) are indeed damaging to children. Any use of hazardous social apps is too much and carries serious hazards. But what about the use of “normal” and/or “safe” social media? Well, data suggest that too much use of “non-hazardous” apps can indeed affect health. How Much Do Teens Use Social Media? First, some basic data. For example, how much do normal teenagers use social media? A study from Pew Research found that more than 50 percent of 13- to 17 year-olds go online several times a day. This quickly increases during the teenage years to more than 70 minutes per day. Teenage girls have the highest usage at just over 140 minutes per day. It is important to recognize that non-school related use of the internet and social media is often beheld by teenagers as important for developing their self-esteem, their acceptance among peers, and their mental health in general. As parents, we recognize that the use of social media can indeed contribute, in many positive ways, to our children’s growth. At the same time, we also worry about them spending too much time online. We worry about their ability to communicate effectively in face-to-face settings or in writing. Many of us also feel and/or worry that our children are addicted. Social Media and Addiction Recent studies suggests that the overuse of social media indeed mirrors addiction. Reports now show that teenagers and college kids experience anxiety when deprived from their connected devices and consequently feel a compulsion to access their social applications. The emotional symptoms they experience are very similar to those seen in substance abuse. In fact, the American Psychiatric Association is considering making internet addition a bonafide diagnosis. Pediatricians therefore encourage limits on the use of social media, a recommendation more easily suggested than accomplished. So when should a parent consider seeking help? Aside from unhealthy use of these apps (cyber-bullying, sexting, online users asking for sexual relations, etc.), which should always trigger concern, the use of social media for more than 120 minutes per day should trigger parental concern. If you feel unable to address the overuse of social media, contact your pediatrician for help and guidance. Renown Children’s Hospital Whether it’s seeing a pediatrician, getting a sports physical or looking for advice, our care is centered around supporting and nurturing patients and families at our many locations. We have pediatricians dedicated to children who have experience recognizing children’s illnesses. They also have knowledge about tests and treatments for young ones to ensure your child gets the best care possible. Explore Children’s Services
Read More About Teens and Social Media: When Is it Too Much?
-
Improving the Way we Deliver Quality Rural Healthcare
One of the most pressing issues in modern medicine is the need to improve rural healthcare. This challenge hits particularly close to home, as Renown Health is the only provider covering 100,000 square miles in northern Nevada, an area that’s mostly rural. People in rural areas suffer from chronic diseases such as heart disease, cancer and respiratory disease, at higher rates than the general population. One of the largest contributors to these health disparities is a lack of access to health services. Many rural communities have fewer providers and care facilities. This forces residents to travel farther to receive preventive care and medical treatment. We must identify ways to better support the health needs of the millions of Americans who live in rural communities. Ideas for improving rural healthcare Health systems must identify innovative ways to leverage existing resources and new technologies to care for patients in these communities. For example, telehealth can help diminish a person’s need to travel long distances to receive specialty care. Similarly, online classes can help educate patients about preventive behaviors. Remote monitoring technology also allows patients to track their health conditions from home. Additionally, we can address physician shortages by empowering health professionals such as nurse practitioners, physician assistants and technologists to care for patients. These providers receive excellent training and have demonstrated success in improving health outcomes. Renown Health cares for people from diverse backgrounds and we are dedicated to caring for patients in every community we serve. Renown Telehealth We’re leading the region in using video conferencing technology to provide the best care possible – no matter where you are. Renown Telehealth is telemedicine that gives you access to top-level care and better outcomes with less stress and fewer travel costs. Learn More
Read More About Improving the Way we Deliver Quality Rural Healthcare
-
How to Get Your Kids to Sleep, Screen-Free
If you’re a parent, you’ve probably been there — the sometimes-nightly struggle to get your little ones off to bed. Elaina Lantrip, an APRN with Renown Pediatrics, offers some tips and explains how your child’s electronics may be getting in the way of a good night’s sleep. These days, kids are consuming media from a very early age on all types of devices — from tablets and phones to TVs. While they can benefit from some media use, it can have a negative impact on bedtime. We asked Elaina Lantrip, an advanced nurse practitioner with Renown Pediatrics, for some advice on downloading a better bedtime routine. What are the most important practices for parents to establish for their children’s bedtime routines? I often have parents tell me that their child won’t go to bed — or to sleep. Parents frequently ask for tips on bedtime routines that work. My first question is whether their regular bedtime routine involves television, iPad, tablet, phone or anything with a screen. It’s very important that bedtime includes a bath, reading a story, talking, singing and bonding with young ones, rather than using any devices. Why shouldn’t children have a device at bedtime? A growing body of research supports that screen time at bedtime contributes to delays in a child’s falling to sleep; overall inability to reach the important REM, or deep sleep; waking up during the night; nightmares and night terrors. For older youth, engaging with social media before bedtime can bring up stresses, emotions and relationship issues with peers that don’t exactly create peaceful bedtime thoughts. Bedtime should be a screen-free, stress-free, peaceful time of day. It’s a great time for parents to promote self-esteem, talk through things going on in the child’s life, to encourage and build them up. Children grow up fast — bedtime is a great the opportunity with younger children to cuddle up and read a story or sing a lullaby. What are other major considerations in making bedtime smooth and relaxing for kids and their parents? Another factor that contributes to positive sleep habits includes children getting enough activity during the the day so they’re genuinely tired at night. Also helpful are ambient noise makers, peaceful music, avoiding sugar two hours prior to bedtime, consistency in bedtime routine, comfortable pajamas and comfortable temperature in the home. Is it important to keep the child’s bedroom dark? Dimming the lights is important, regardless of the time of year. This is another reason to ban screens, as they emit light that stimulates wakefulness.
-
Women and Stroke Surprising Signs to Know
Stroke is unfortunately common, with 1 in 5 American women experiencing it each year. When it comes to a stroke the phrase “time is brain” speaks to the urgency of getting rapid care. In fact, a woman may lose nearly 2 million neurons per minute of oxygen loss to the brain. The Renown Health Comprehensive Stroke Center experts share the importance of timely treatment and how stroke symptoms can differ in women. Women and Stroke – Surprising Symptoms Each year stroke affects more women than men. Even more concerning, women are less likely to recover from a stroke. The following non-traditional, less common, warning signs can be common in women: Hiccups with chest pain Sudden disorientation, drowsiness, confusion or a general altered mental status Nausea or vomiting A sudden headache that feels like the ‘worst headache of your life’ Unusual chest pain (especially with hiccups) Body numbness or weakness, such as an arm or leg suddenly ‘falling asleep’ Fainting or loss of consciousness Stroke Diagnosis The first step is neuroimaging by CT scan. This allows for rapid identification of any bleed, and also assists in determining candidacy for the early clot busting medication. MRI brain imaging is much higher resolution, and can better determine the core stroke size, assisting in prognosis and recovery. Since strokes have several different origins, an inpatient workup is essential to determine the underlying cause. Whether the stroke is secondary to plaque in the large vessels, clots being thrown in the setting of atrial fibrillation (an abnormal heart rhythm), or small vessel disease from years of uncontrolled vascular risk factors (high blood pressure, smoking, high cholesterol, diabetes), determining the cause is essential to implementing a management plan to reduce risk for further strokes. Quick Treatment for Stroke is Key Early recognition of stroke symptoms and seeking prompt attention is paramount. There are interventions that can be instituted to minimize the stroke and increase likelihood of recovery, but only if a patient presents to the hospital early. A clot busting medication, called tPA, can be given to patients with stroke if given within 4-5 hours from time of onset. Renown Regional Health Center is designated as a Comprehensive Stroke Center, the highest level of stroke certification available. To earn the designation of comprehensive stroke center, a hospital has to meet stringent requirements, including biannual on-site evaluations. This includes care for ischemic stroke patients (lack of blood flow), hemorrhagic stroke patients (bleeds), and determining the underlying cause to guide secondary stroke management prevention. Stroke Symptoms Remember “B.E.F.A.S.T.” to recognize the symptoms of a stroke below: B – Balance Being off balance or dizzy, is common. E – Eyes An eyesight change such as blurring or double vision may occur. F – Face droop One side of the face, or lip, droops A – Arm weakness Does one arm drift down? S – Speech Talking may slur or sound strange. T – Time Time to call 911. Call an ambulance immediately if you or anyone else, experiences any of these symptoms.
-
Department Spotlight: Acute Care Rehab Therapy
Being admitted to the hospital is never easy. Being admitted for a traumatic injury can be even harder. Whether it's learning how to walk again or powering through a new speech therapy routine, recovering from an injury that may affect the course of your life can be daunting. But it doesn’t have to be, thanks to the Acute Care Rehab Therapy team at Renown Health. The smiling faces of the Acute Care Rehab Therapy team at both Renown Regional Medical Center and Renown South Meadows Medical Center will make you see that there is a light at the end of the tunnel. Your dedicated physical therapists, occupational therapists and speech language pathologists are here to serve you and place you back on the right path to recovery and function. The Role of Acute Inpatient Therapy The Acute Care Rehab Therapy team comes in at a critical juncture in a patient’s care process after hospital admission. As one of the primary rehabilitation partners on a care team, these dedicated therapists are here to maximize every patient’s safe and independent living before they set off back home – all while reducing the risk of hospital readmission. “As physical therapists, we address musculoskeletal deficits and assess a patient’s current function after acute injury or illness from their baseline and develop a plan for functional recovery,” said Kristie Eide-Hughes, Physical Therapist at Renown Regional. “We also use our clinical expertise to assist with the discharge process and make sure each patient has the best durable medical equipment the first time around, removing the guesswork.” “On the occupational therapy side, we work with patients to facilitate their independence with basic life skills, such as dressing, bathing and using the restroom,” added Jeanne Clinesmith, Occupational Therapist at Renown Regional. “In the pediatric setting, we help babies and kids get back to what they were doing before they came into the hospital,” continued Rhonda Yeager, Pediatric Occupational Therapist at Renown Regional. “In the NICU specifically, we support the development of babies, trying to prevent problems from worsening. It’s nice to be a source of positivity in an otherwise intimidating situation.” The role of therapy in this setting reaches all ages, from babies in the neonatal intensive care unit (NICU) to adults approaching end-of-life care. Every therapeutic approach is tailored specifically to each patient. “Therapy is more of a habilitative approach for infants in the NICU, while it is more of a rehabilitative approach for kids and adults following injury or illness,” said Sara Carolla, Physical Therapist at Renown Regional. Each team member in the Acute Care Rehab Therapy department is dedicated to each patient, helping them make progress from start to finish and giving them the tools to succeed along the way. “I enjoy the variety of the patients we get to see and the ability to see them make gains from the wonderful treatment they get in the hospital from my team,” said Kelly Schwarz, Occupational Therapist at Renown South Meadows. “We provide education as each patient’s acute issues evolve,” added Nicole Leeton, Speech Language Pathologist at Renown Regional. “One of my favorite parts of my work is the patient and family education aspect, and that includes other healthcare provider education as well. It’s a moving picture.” Moreover, every team member gives each patient tools to learn how to be themselves again and empowers them to continue striving for the best possible result of their therapy “We get the opportunity to make a person’s bad experience in life better even by spending one session with them, giving them the keys to unlock something that they didn’t think they had the ability to do,” said Dana Robinson, Occupational Therapist at Renown Regional. On the Road to Independence Our dedicated therapists in the Acute Care Rehab Therapy team set the stage for a patient’s recovery process after trauma, showing them their potential for independence. With a multitude of patients coming into the hospital with many degrees of medical complexity, each day is different while the end goal is always the same: to optimize function as early as possible while overcoming any barriers and paving the way for a comfortable and effective quality of life. “Early intervention is a big piece,” said Nicole Leeton. “Us seeing patients early can get them recovered and independent more quickly and help prevent future illness and injuries. For example, in speech therapy, getting in early and facilitating communication skills for patients with impaired speech can make a huge difference.” Acute Care Rehab therapists dig deeply to see the whole picture of each patient’s situation to foster their independence – their history, social skills, support system and more. “Sometimes, we are the difference between independence and dependence,” said Dana Robinson. “We are the eyes and ears because we have so much time with the patients. Our team is extremely collaborative and develops a great rapport with patients, so they feel comfortable telling us everything going on with them.” “For kids, we teach parents ways they can help their kids by setting up their homes and the equipment they need to succeed,” added Rhonda Yeager. According to the team, one of the biggest keys to independence is repetition. A continual flow of getting up and trying again is crucial for recovery. “Repetition helps people regain their quality of life back sooner and control their recovery process,” said Megan Hough, Physical Therapist at Renown Health. “Helping people continue to get stronger and more independent makes my job so rewarding,” added Sam Brown, Physical Therapist at Renown Regional. Knowing that they have made a difference and help shape a patient’s overall development inspires each therapist to never give up, regardless of how difficult an injury presents. There is no set schedule for recovery, and the therapists are always in the patient’s corner. “This team has the most passionate, caring and dedicated individuals that I know,” said Kendra Webber, Manager of Acute Inpatient Rehab Therapy Services at Renown Regional. They give 110 percent to every patient every time to ensure they have what they need to regain function and independence.” “By tailoring therapy to the individual, the bounds are virtually limitless for what we can accomplish,” added Dana Robinson. It Takes a Village Since acute inpatient therapy is never a one-size-fits-all approach, it truly takes a village for this team to move the mountains they do for patients every day. These teams are fact-finding masters, gathering all the necessary information from the patient, their family and their care team to figure out their precise needs. “We are a consistent presence for our patients, identifying a lot of different needs and meeting those needs to help patients grow in their treatment process,” said Kelly Schwarz. “By collaborating with each patient’s diverse care team, we are able to employ the clinical judgment to help patients overcome physical, emotional and environmental struggles and set them up with the proper resources once they leave our setting.” “Our team has steady communication with physicians, nurses, acute care technicians, respiratory staff, physician assistants, case managers and more to ensure the best possible care,” added Jet Manzi, Physical Therapist at Renown Regional. Constant communication and collaboration are also necessary beyond the acute treatment process. These skills are vital in order to facilitate discharge planning, and the Acute Care Rehab therapists are an essential resource in the discharge process alongside our Hospital Care Management team. “Often times, a patient’s family needs a lot of guidance in helping their loved ones determine the next level, and we help them navigate those steps and the resources available to them,” said Mark Stumpf, Occupational Therapist at Renown Regional. “And it’s all a team effort.” “Our therapists are the most committed, generous, hardworking people,” added Courtney Phillips-Shoda, Supervisor of Rehab Therapy Services at Renown Regional. “Despite being short-staffed, we come to work every single day and give everything to our patients. They are the priority.” If you take away one thing, know this for certain: Renown’s Acute Care Rehab occupational, speech and physical therapists will always be there to help patients continue on a positive trajectory to physical, mental and emotional recovery. “Whether you are a patient or a provider, if there is a problem, never hesitate to reach out to us,” said Nicole Leeton. “We are always receptive to anyone seeking our help.” With the Acute Care Inpatient Therapy team on their side, a patient’s journey to recovery is only just beginning.
Read More About Department Spotlight: Acute Care Rehab Therapy
-
Department Spotlight: Clinical Engineering
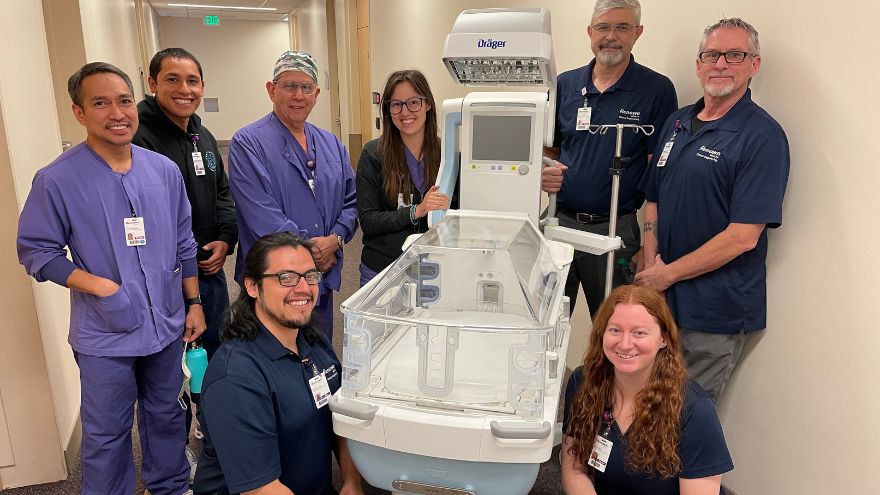
Renown Health strongly supports and advocates for innovative medical technology. Our diverse lineup of medical equipment enables our care leaders to provide quality care to every patient. But what if a piece of technology breaks down? What happens when our care teams are ready for technological upgrades? Where do employees go when they have a question about a complicated piece of equipment? Enter the Clinical Engineering department. This sophisticated team is staffed with intelligent, science-minded individuals who are ready to jump in and help at any given second. From newborn incubators to robots that clean the hospital floors, these team members are the med-tech masters that keep our health system running. Equipment Experts Upon entering the Clinical Engineering department’s workshop, you are welcomed with an abundance of high-tech equipment undergoing repairs and upgrades. The department takes care of more than 26,000 pieces of equipment throughout the entire healthcare network, including the technologies at the University of Nevada, Reno School of Medicine, which they just took over this past year. To the average person, this may seem overwhelming; however, for this team, this is the exact environment they thrive in to make the technology magic happen. “I am motivated and engaged every day at work,” said Tony Martinez, Supervisor of Clinical Engineering for Renown. “Our department is fast-paced and rewarding, and that’s a big plus.” While some team members enter the department as equipment generalists, this team offers training to develop their skills on certain pieces of equipment, eventually becoming specialists. “Every month, we encourage our colleagues to undergo specific training on more delicate equipment,” said Tony. “Once we get to that point in their training, we assign different equipment to our team members every month. They pick up the experience very quickly.” As a Clinical Engineering Technician for Renown, Rylie Nickerson took advantage of the training and educational opportunities offered to her and is now a ventilator specialist especially for Renown’s neonatal intensive care unit (NICU). “Regardless of whether I’m working on ventilators or on another piece of equipment I’m assigned to, I’m always thinking about how I can help the patients, nurses and doctors,” said Rylie. Raul Hernandez, a Clinical Engineering Specialist for Renown, is the go-to person for anesthesia, heart-lung bypass, red cell saver and life support equipment. He embraces the fact that, regardless of whether you are a specialist or a generalist, there is no typical day working in this department. “Every day brings different challenges,” said Raul. “I really enjoy the mental exercises I do every day. They keep me grounded and focused.” On top of their day-to-day work and any special projects or emergencies that come up, the team is on an ongoing preventative maintenance schedule. Think of this work like your car’s oil change – routine maintenance to prevent something from breaking down in the future. “At any point, we might have 100-200 extra pieces of equipment to handle during preventative maintenance,” said Taylor Gray, a Clinical Engineering Technician for Renown. “We are always helping each other through any issues.” Our Clinical Engineering team shows exactly what it means to be collaborative. Even though their to-do lists are ever-growing, this team never feels alone. They know they can always lean on each other for support, regardless of the workload. “We always have each other’s backs,” said Taylor. “I feel so happy and satisfied in my job, and my coworkers are a large part of that.” Celebrating the Genuine Difference The Clinical Engineering department is driven by their desire to help and take care of the entire health system, and in turn, make a genuine difference for the communities we serve, from the medical staff to the patients. “The satisfaction you get in our field when we impact patients’ lives and their healing process is so motivating and engaging,” said Tony Martinez. “It’s a great feeling.” The team knows the common saying ‘Walk a mile in someone’s shoes’ very well; so well, in fact, that they take it to the next level, doing everything they can to prevent frustrations and extended down times. “We try to walk a mile in someone’s shoes before they get angry,” said Reagan Jordan, Director of Clinical Engineering for Renown. “Your satisfaction is our mission, and our team continually works to improve their outcomes every day.” This department is where the entrepreneurial spirit and science-focused mind meet. For people like Raul Hernandez, who came from a business background as well as decades of medical technology experience, Renown helps him bring both his personal and business skills into focus. “This environment is very beneficial for Renown, me, and of course, the patients,” added Raul. Being members of a team that is committed to excellence and purpose inspires them to reach new heights in patient care. “I am constantly reminded of the positive impact we have by witnessing the individual experiences we have and hearing the enthusiasm and thankfulness in their voices,” said Raul. “It gives me a great sense of pride to work at Renown.” "There is a strong feeling of mutual respect here,” added Ed Trejo, a Clinical Engineering Technician at Renown. “We are always here to help.” The proof is in the data. The Clinical Engineering team scored as one of the top departments in the recent Renown employee engagement survey, with their results sitting at more than 94 percent. “This speaks to not only our department leadership but also the team as a whole,” said Reagan. “I am extremely proud of them. Despite the pandemic, they are knocking it out of the park.” For this department, coming to Renown is easy; staying at Renown is even easier. “Staying at Renown is the easy choice,” said Raul. “And this team is only going to grow.” Workflow Whizzes and Kindness Champions “Rolling with the punches,” as Tony Martinez says, comes naturally to the Clinical Engineering team. With the constant workflow of equipment coming into the shop, every team member has learned how to be experts at prioritizing, especially based on the needs of our organization. Even though their jobs can bring a lot of intensity, this department’s positive attitude radiates throughout the hospital. Upon entering the workshop, everyone is greeted with a smile from every team member, along with an immediate willingness to dive into the complex world of engineering. “The experience of helping other people with their unique needs is invaluable,” said Taylor Gray. If this work environment sounds enticing, great news – the Clinical Engineering team is growing. Motivated, aspiring engineers with a passion for healthcare and an associate’s degree in a related field are welcome. Military experience is also valued very highly in this team. As many of our military servicemen and servicewomen gain specialized engineering experience while enlisted, the military-to-engineer career ladder at Renown is especially strong. In fact, according to Paul Joseph, a Clinical Engineering Technician at Renown, the majority of their teammates come from a military background. Above all, being capable of prioritizing on the fly, thinking critically, having an open-mined outlook and being self-driven are the top skills that this department values. As Ed Trejo states, “If you’re willing to wear different hats, you will do very well here." “Go with the flow, and expect the unexpected,” added Rylie Nickerson. Those who join this team feel at home. The warm embrace of the team’s kind nature and the supportive environment they all foster inspires an efficient workflow that helps our entire hospital system function at the top of its game. At the end of the day, everyone who joins the team, or anyone who even interacts with the team in any capacity, will be in good hands. Mandy Noriega, a Clinical Engineering Technician for Renown, closes these thoughts with a great reminder to each and every one of us: “After all, teamwork makes the dream work.”
-
Are You at Risk for Stroke?
Did you know an estimated 1.9 million neurons and 14 billion synapses are lost per minute during a stroke? That’s why every second counts. Anyone can have a stroke, but your chances increase if you have certain risk factors. That’s why the best way to protect yourself or your loved ones from a stroke is to know the risks and how to manage them. You can make changes to your lifestyle to lower your risk of stroke by asking yourself the following questions: 1. Is my blood pressure normal? High blood pressure is the leading cause of stroke and the most important controllable risk factor. If you’ve had a stroke, lowering your blood pressure can help prevent future strokes. 2. Can I quit smoking? Smoking damages blood vessels, clogs arteries and raises blood pressure — doubling your risk of stroke. If you want to reduce your risk of stroke and heart attack, quitting smoking is the first step — and Renown can help you with this. Learn more: Renown Health Quit Tobacco Program. 3. Do I make time to exercise 30 minutes a day? Many studies link consistent exercise habits with lower stroke risk. Also, being overweight contributes to high cholesterol, high blood pressure, heart disease and diabetes, all increasing your stroke risk. You don’t need to run a marathon — just commit to making time to move each day. 4. Do I regularly eat processed food and sugar? Eating less cholesterol and fat, especially saturated and trans fats, may reduce the fatty deposits (plaque) in your arteries. Also, eating five or more servings of fruits and vegetables per day may reduce your stroke risk. If you are diabetic, follow recommendations to get your diabetes under control.