Search
-
Prevent Osteoporosis: Take Control of Your Bone Health Today
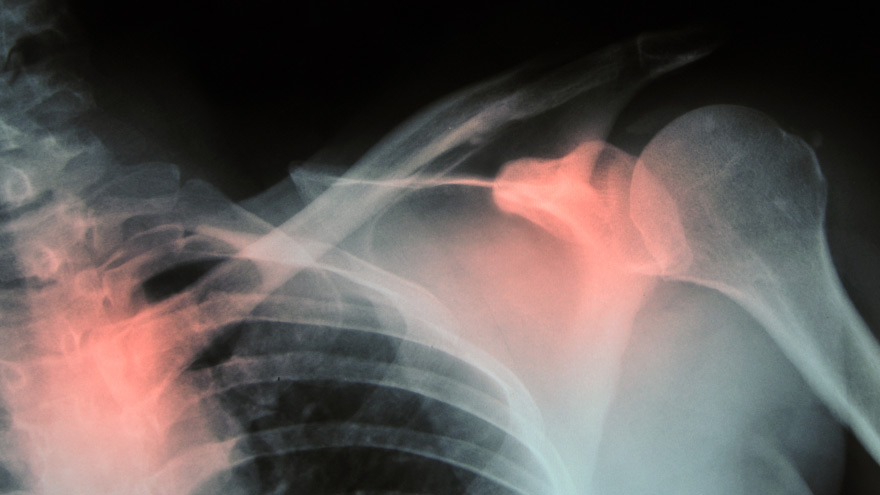
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
Ask the Expert: What is Scoliosis?
Posture is important, but for those children diagnosed with scoliosis (spinal curvature) it can be a difficult issue. The Washoe County School District Student Health Services Department screens 7th grade students for scoliosis as growth spurts often reveal the condition and, if diagnosed early, scoliosis can stop progressing. We asked Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis to answer some frequently asked questions about scoliosis. What is scoliosis? There are many types of scoliosis: early onset (occurs before age 10), congenital scoliosis is when the bones of the spine do not form correctly, neuromuscular scoliosis which is due to children’s neurologic and muscle disease, and the most common is Adolescent Idiopathic Scoliosis. The term “idiopathic “ means the exact cause is unknown, although we do know it runs in families. This type of scoliosis occurs in 2-3 percent of adolescents and is mainly seen during their growth spurt. This is why middle school screenings are recommended. Both genders get scoliosis but girls are 8 times more likely to have their curves progress and become larger. What are the signs that my child may have scoliosis? A few signs for parents to watch for are: One shoulder might be higher than the other. One leg may seem longer. A hip may be higher or look more prominent. The waist may not look the same from side to side (asymmetry). The trunk or rib cage may be more prominent on one side or shifted. When they bend forward they may have a bump on their back. How is scoliosis diagnosed? It can be noticed by a pediatrician at a physical, school screening nurse, PE teacher or parents. Once the curve is suspected the child is usually referred to a pediatric orthopedic surgeon scoliosis expertise. At the initial visit the doctor will perform a thorough physical including a complete neurologic exam to assess the amount of curvature. Once the exam is completed the physician will determine if a spinal x-ray is needed. The curve on the x-ray is measured utilizing the cobb angle (a measurement in degrees) which helps guide the treatment. What are common treatments for scoliosis? The treatment depends on the size of the spinal curve and the amount of growth the child has remaining. An x-ray of the child’s hand is used to determine the amount of growth remaining. This allows the determination of the child’s bone age, and based on the hands growth plates it can determined if the child is in their rapid phase of growth. Treatments include: Observation - For curves less than 20-25 degrees. This entails visits every 6-9 months with a repeat scoliosis x-ray. Since scoliosis curves increase only 1-2 degrees per month, and variations in measurements can be 3-5 degrees, an x-ray is not recommended before 6 months. If the curve remains less than 25 degrees the child is followed until their growth is completed (usually age 16-18). Progressing Curve - If growth is finished and the curve is less than 40 degrees, the risk of more curvature into adulthood is small. If growth is completed and the curve is over 45 degrees, the child is followed for several years as these curves can progress into adulthood. If the patient is still growing and the curve has progressed greater than 25 degrees but still in the non-operative range (less than 45-50 degrees) bracing is used to stop the progression of the curve. Bracing - Indicated for curves over 25 degrees but less than 45 degrees. If a brace is required you will be referred to an orthotist (bracing specialist). The orthotist assesses your child, reviews the x-ray and then fits the brace. (Having a brace made usually takes 2-3 weeks.) Once the brace is fit, your child will visit the scoliosis specialist for an x-ray in the brace to ensure it fits correctly. The primary goal of bracing is to halt progression of the curve and prevent the need for surgery. The brace must be worn for about 16 hours per day to be effective. In a recent bracing study 72% of the patients who wore their braces as prescribed prevented the need for surgery compared to the group who did not wear their brace. Surgery: When a curve reaches 45-50 degrees, and a child is still growing, surgery is usually recommended because the curve is likely to continue progress. If a curve is over 50 degrees and the child is done growing surgery also may be recommended. This is because when curves are over 50 degrees they tend to increase 1-2 degrees per year for the rest of your life. As curves get larger the amount of lung function tends to decrease which could cause breathing problems later in life. The goals of surgery are to stop the progression of the curve and safely correct any misalignment. This is accomplished by attaching implants (rods, screws, hooks and bands) to the spine. Bone graft is then placed around the implants to encourage the spine to fuse (grow together). This then forms a solid column of bone with metal rods in place, preventing the curve from changing. Most patients are back to their regular sports and activities six months post surgery.
-
Get to Know the Types of Car Seats
Parents often struggle with installing and choosing car seats for their children. Picking out a car seat for your child is a never-ending battle. Safe Kids Washoe County has made it simple for you to understand the types of car seats that will work for your child. Types of Car Seats Rear-Facing Only Seat. Your baby's first car seat is often used from 5 to 40 pounds. People usually buy this type of seat because it is portable. Convertible Car Seat. This seat is larger and stays in the car; it may be rear-facing until your child is two years or more. After that, it can change to a forward-facing seat. Forward-facing-only car seat. This type of seat is used in one direction and has a 5-point harness and top tether. Combination seat. This is a forward-facing seat with a 5-point harness and top tether and can change into a booster seat when you remove the harness. 3-in-1 car seat. This seat also stays in the car. You can use it rear-facing, forward-facing, and then later, as a booster seat. Booster seat. It boosts the child for a safer and more comfortable fit of the adult seat belt. Make sure your child has outgrown the weight or height limits allowed in the forward-facing car seat. The seat belt must lie flat across your child's chest, on the bony part of the shoulder, and low on the hips or upper thighs. Most children will be between the ages of 8 to 12 years old before they are ready for the seat belt alone. Have a trained car seat technician check your installation Why: 3 out of 4 car seats are installed improperly, with some studies show that the misuse rate is 90%, with the average car seat having three mistakes. Solution: Ensuring that your child's car seat is installed correctly by a certified car seat technician will ensure your child's safety.
-
Transitioning Your Child Out of Their Car Seat
Car seat technicians often find parents are moving their child to their next car seat stage too soon, as they get older. Here are a few reminders of when to transition your child from their booster seat to a seat belt. Moving to a booster seat too soon According to Safe Kids Worldwide, nearly 9 in 10 parents remove children from their booster before they’ve reached the recommended height, weight, or age of their car seat recommendations, which leaves the seat belt in a position on the child that could injure them. If the child is not the proper height, the seat belt can rise up on the belly, instead of the hips where it’s supposed to sit, which can lead to spinal cord damage or whiplash in the event of a car crash. Solution: You can switch from a car seat to a booster seat when your child has topped the weight allowed by the car seat manufacturer; typically 40 to 80 pounds (18 to 36 kilograms). Remember, however, that your child is safest remaining in a car seat with a harness for as long as possible. Booster seats must always be used with a lap and shoulder belt — never a lap-only belt. Transitioning to a safety belt too soon Older children need booster seats to help ensure the seat belt stays properly positioned on their body. The lap belt should lie low across the child's hips and pelvis with the shoulder belt crosses the middle of the child's chest and shoulder, so that in the event of a crash, the forces are applied to the hip bones and not the abdomen. If the lap belt is not positioned properly then it could lead to injuries to the spinal cord and abdominal organs. Solution: Most kids can safely use an adult seat belt sometime between ages 8 and 12. Always use a booster seat until the child passes the 6-step test Your child reaches a height of 4 feet, 9 inches (nearly 1.5 meters) Their back is flat against the seat back. Knees bend over the edge of the seat and feet are flat on the floor. The shoulder belt sits on their shoulder and chest (not face or neck.) The lap belt sits low on their hips and touches their upper thighs (not on their stomach.) Your child can sit comfortably this way for the entire trip. The American Academy of Pediatrics reminds us that the back seat is the safest place for children younger than age 13.
Read More About Transitioning Your Child Out of Their Car Seat
-
Why I Give: Sarah’s Story
As an avid soccer player, Sarah saw her fair share of doctors growing up. However, it wasn’t until she was diagnosed with celiac disease, an autoimmune disease affecting how the body ingests gluten, that she became passionate about healthcare. “I couldn’t figure out what was going on,” Sarah said. “I was getting sick, and my symptoms were getting worse.” Thankfully, after seeing a handful of doctors, she was on the path to recovery. “I remember being so relieved, and still am! Now I can focus on getting better,” said Sarah. The most important change people make after being diagnosed with celiac disease is the shift to a gluten-free diet. For many, Sarah included, living gluten-free is a lifestyle change. Thankfully, Sarah sees significant improvements in her health after adjusting her diet. “No one should just accept their symptoms as part of life,” said Sarah. Her increased awareness of health and nutrition motivated Sarah to study biology at the University of Nevada, Reno (UNR). “I want to be a pediatrician so I can help patients, especially kids, figure out treatment plans.” said Sarah who credits her experience living with celiac disease as her inspiration. Dancing for Kids’ Health Currently a senior at UNR, Sarah is a member of Phi Delta Epsilon, a co-ed international medical fraternity. Together with her classmates, she is bringing new energy and ideas to philanthropy. Sarah and the members of Phi Delta Epsilon are doing things differently and in many ways redefining what it means to give. This year, they are on a mission to raise funds for kids’ health at Renown Children’s Hospital. And they are doing this by dancing. The UNR Dance Marathon is part of the Miracle Network Dance Marathon, a student-led, year-round philanthropic movement that unites students across the United States and Canada. Collectively, they raise critical funds for Children's Miracle Network Hospitals. And Renown Children’s Hospital is our northern Nevada CMN partner hospital. Since 1991, over 400 college campuses and thousands of students have raised $300 million for kids. Sarah is the executive director of UNR’s chapter. “So far this year we’ve already raised $10,000 for Renown," said Sarah. Most of the fundraising happens on the day of the dance marathon. But throughout the school year, students hold mini fundraisers on campus and in the community. One hundred percent of the funds raised stay local, impacting Renown’s youngest patients. For every dollar donated, 18% helps provide charitable care, 15% goes to life-saving equipment, 12% supports medical research and 55% provides education, patient services and advancement services. “It's inspiring that we banded together to help kids in our community,” said Sarah. Last year they raised over $18,000. They are hoping to exceed that number at this year’s dance marathon in April.
-
Understanding the Risks of Colon Cancer
Colorectal cancer is the second-deadliest cancer in the United States – largely because it goes undiagnosed. Dr. Christi Matteoni, Division Chief of Gastroenterology at Renown Health, discusses the symptoms and key screenings used to detect this type of cancer, along with risk factors and lifestyle changes that could affect the likelihood of getting the disease. What are some of the signs and symptoms of colorectal cancer? Many cases go undiagnosed because polyps can develop and become cancerous without any symptoms. Additionally, since colorectal cancer begins as small polyps, symptoms usually aren’t seen until later stages. This is why screenings are especially important. For those who do experience symptoms, the signs are often tied to your bowel habits. This can include changes such as constipation or diarrhea, narrow or dark stool, rectal bleeding, abdominal cramping, weakness and fatigue or unintended weight loss. What are some of the risk factors associated with this type of cancer? There are risk factors that can and cannot be controlled. Uncontrollable factors include age, race, personal and family histories as well as certain genetic syndromes that are important to discuss with your provider. This type of cancer is more common in people over the age of 50, African Americans and those of eastern European Jewish (Ashkenazi) descent. This type of cancer is also more common in those who have been diagnosed with polyps, Crohn’s disease, ulcerative colitis and long-term inflammatory bowel disease. important to discuss any of these risk factors with your provider. There are also lifestyle factors that can help reduce your risk. Factors include being overweight, having a diet high in red and processed meat, as well as smoking and consuming excess alcohol. Conversely, diets high in fruits and vegetables and a regular exercise routine can help lower your risk. If someone has some of these risk factors, what should they do? Do they need to get tested? If you are 45 or older and have any of these risk factors, we recommend you speak with your primary care provider about a formal colorectal risk assessment. The most common form of screening is colonoscopy. This screening lets your doctor examine the length of your colon, map out any potential problem areas and remove polyps. For most people, colonoscopies are recommended every 10 years starting at age 50. However, depending on your results and risk factors, you may need to begin screening sooner or get screened more frequently. What do diagnosis and treatment look like for this type of cancer? There are several diagnostic options for colorectal cancer, including endoscopic ultrasound; CT, MRI and PET scans; and biopsy and pathology reports. These technologies allow your doctor to get images of your colon and evaluate what treatment is needed, as well as how the treatment is progressing. Treatment varies for each individual working with their doctor. In the case of colorectal cancer treatment, the William N. Pennington Institute for Cancer offers chemotherapy, radiation therapy, surgery and clinical trials.
-
How You Can be a COVID-19 Vaccine Ambassador
We get it – the entire world has been overwhelmed with COVID-19 vaccine information, questions and celebrations around vaccines developed to combat COVID-19 induring the past several months. It’s hard to know where to start in digesting all this news and information. But one thing is clear: healthcare experts agree that the authorized COVID-19 vaccines are safe, effective and recommended to help end this pandemic. If you are passionate about stepping up in your community to encourage the vaccination efforts, we’re offering a few ideas on how you can be an ambassador. Find the Facts Content on the vaccine is abundant, but and there’s a few resources that we can all rely on to help digest the information: The Centers for Disease Control (CDC) updates its website content around the vaccine regularly, and also offerings information in Spanish. Health departments across the U.S. are leading the way in distribution logistics planning, and partnering with other providers, like such as hospitals and pharmacies, to distribute give people doses. Their websites are great resources to understand options where you live. Locally, check out washoecounty.gov/health/programs-and-services/environmental-health/covid-19-guidance for vaccine updates in Washoe County. Many providers like Renown Health and other providers are sharing content around their recommendations for the vaccine. Get answers about the vaccine types from one of our pharmacists, read common concerns addressed by experts and view videos from many doctors and other specialists on our YouTube Channel.
Read More About How You Can be a COVID-19 Vaccine Ambassador
-
Renown Health Foundation Shines Bright
Renown Health Foundation and local community members raised over $1,000,000 at a charity concert with The Beach Boys and special guest NFL legend Steve Young, on Sunday, June 5, at Montreux Golf and Country Club. The event benefits the construction of Sophie’s Place, a new dedicated music therapy room coming to Renown Children’s Hospital. Over 500 donors attended the inaugural event hosted by radio personality Wink Martindale. The Beach Boys front man Mike Love, a Nevada resident, generously auctioned off two once-in-a-lifetime, private concerts bringing in $300,000. Steve Young auctioned off a Monday Night Football package and ZLINE Kitchen and Bath auctioned off a kitchen remodel. The proceeds raised will be transformative for Sophie’s Place and will impact children in our community for years to come. “I’m thankful to Renown and other children’s hospitals that are dedicating space, precious space, for Sophie’s Place,” says Steve Young, founder of Forever Young Foundation and co-founder of Sophie’s Place. View photos from the event here. What is Sophie’s Place? Sophie’s Place is a dedicated music therapy room in children’s hospitals across the country. Founded by the Forever Young Foundation and former San Francisco 49'ers quarterback, Steve Young, they provide a comprehensive music and healing arts program. Established in loving memory of musician Sophie Barton, the first Sophie’s Place opened in 2013 at Primary Children’s Hospital in Salt Lake City, Utah. Additional locations include Sutter Children’s Center in Sacramento, CA., Cardon Children’s Medical Center in Mesa, AZ., Lucille Packard Children’s Hospital in Palo Alto, CA., and Brenner Children's Hospital in Winston-Salem, NC. Renown Children’s Hospital will be the next location to break ground and will provide our youngest patients with a state-of-the-art music room. It will be the first of its kind in our community. “Sophie’s Place is a wonderful addition to what a hospital has to offer,” says Dr. Max Coppes, Pediatrics Chair, UNRSOM. Where will Sophie’s Place be Located? Sophie’s Place at Renown Children’s Hospital will be located on the ground floor of the Sierra Tower, next to The John & Sue Dermody Children’s Healing Garden. The family-centered space is designed for children to enjoy the healing aspects of music and encourage creativity and expression during their stay. “We really wanted kids to feel like they’re not in the hospital. It’s a place where they can escape,” says Barb Young, Founder of Forever Young Foundation and Co-founder of Sophie’s Place. The room includes a performance space, recording studio, musical instruments, editing software and an art and play area. “When you walk into a Sophie’s Place, you really feel like you’ve left the hospital and walked into a cool coffee shop,” says Sterling Tanner, President, Executive Director, Forever Young Foundation. How You Can Help Make a Difference Renown Health is focused on being the destination for all your family’s health and healthcare needs. As a not-for-profit health system, Renown relies heavily on community funding. If you are interested in supporting Sophie’s Place at Renown Children’s Hospital, please consider giving to Renown Health Foundation. Make a gift at renown.org/give Call Renown Health Foundation at 775-982-5545 Mail a check to Renown Health Foundation, 1155 Mill St., 02, Reno, NV 89502
-
Why I Give: Rebecca's Story
Giving back to the community is important to Rebecca Dickson. For over 35 years, she’s been unwavering in her support of Renown Health and Reno’s non-profit community. Hearing that she’s made a difference in someone’s life feels good. But for Rebecca, the greater reward is something more personal. “Giving back is a way of life,” Rebecca said, “that’s what you do.” Inspired by her parents, the act of generosity was instilled in her from a young age. Growing up, Rebecca remembers her mother’s thoughtful generosity with others. It was her mother, Fianna Dickson Combs, who inspired and helped plan Fianna’s Healing Garden in the heart of the Renown Regional Medical Center campus. The garden is Fianna’s legacy and gift to those in need of comforting, healing and quiet contemplation. Walking through the garden, Rebecca points out the fountain. She talks about choosing it for its calming sound. Birds chirp on the trees overhead. The space is beautiful; it’s tranquil and comforting. Fianna’s Healing Garden was completed in 2009. In 2020, to celebrate the tenth anniversary of the garden, Rebecca and her uncle, Harvey Fennell, led an expansion project to grow the space. Inside the garden, there are pathways, benches, sculptures, fountains and over 2,000 plants and trees. Roses are life “The rose garden is special,” said Rebecca. It was carefully curated in honor of Fianna and her sisters to create a peaceful space for reflection. There are 21 roses of differing sizes and colors. “The roses should be experiential. The fragrance, the colors; they are life with good days and bad. Fianna was a master gardener and felt that gardens tend to the mind, body and soul,” says Rebecca. Honoring Fianna’s Legacy Throughout the hottest days of summer, Rebecca and her partner, David Geddes, visit the garden. They maintain the roses, removing damaged branches and pruning them. “It’s not work,” says Rebecca, “it’s a joyful opportunity that makes us feel good.” Being in the garden reminds Rebecca of her mother and the need for healing gardens in healthcare. When her mother was in the hospital, her doctor encouraged her to get outside and into nature. At the time, Renown didn’t have an outdoor garden space. From then on, it was Fianna’s mission to create a healing garden for patients, caregivers and visitors. Nature reduces stress and anxiety. It also provides comfort and distraction. Healing gardens offer spiritual and healing benefits, and they’ve been proven to improve health outcomes. Before Fianna passed, her plans for at healing garden at Renown were already underway. Making an Impact Rebecca is a lifelong philanthropist. She serves on countless boards, volunteering her time to give back to the community. She currently sits on Renown Health Foundation’s Board. Through her volunteer work, Rebecca not only gets to experience the joy of helping others first-hand, but she also gets an inside view of how non-profits operate and what they need most. That information helps her decide how to direct her support in the most impactful way. Rebecca receives cards and phone calls thanking her for Fianna’s Healing Garden and the comfort it provides. But Rebecca insists that she’s not to thank. Rebecca remembers every person who has supported the garden. Fianna’s Healing Garden is donor-funded, and would not be possible without the support of the community, her uncle, Harvey Fennell, Fianna’s closest friends, Renown physicians and employees, Renown Health Foundation and countless community foundations and local donors. She says, “The garden is a collaborative project. It takes a village to build and maintain, but it’s worth it!” From all of us at Renown, thank you, Rebecca, for your inspiration and dedication to Renown! Fianna’s Healing Garden is located at Renown Regional Medical Center and is open for all to experience the healing power of nature. Click here to take a virtual tour of the garden. Renown Health Foundation’s Why I Give series recognizes donors, volunteers, corporations, foundations and others who provide philanthropic support to Renown. We are fortunate to have generous donors whose funding helps support and expand our efforts to meet the growing needs of the communities we serve. To learn more about how you can support Renown, please email foundation@renown.org or call 775-982-5545.