Search
-
-
11Jun
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
10Dec
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
13Aug
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
10Sep
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
9Jul
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
12Nov
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
8Oct
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
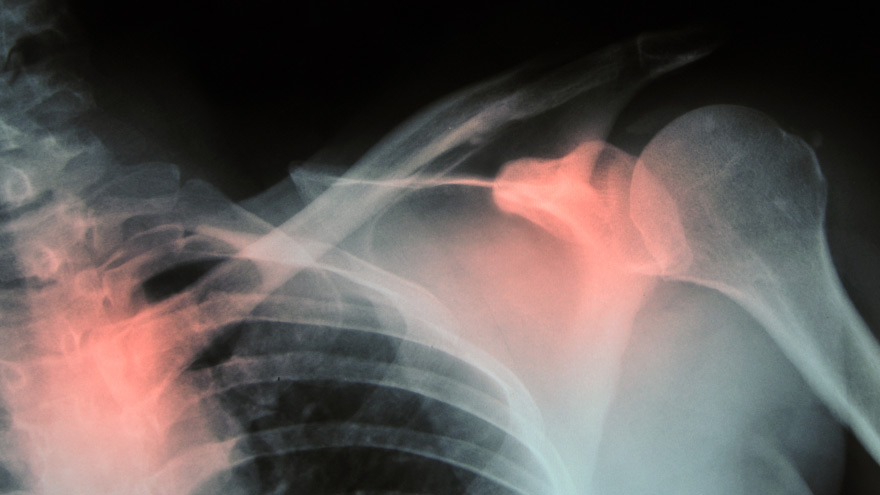
Prevent Osteoporosis: Take Control of Your Bone Health Today
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Fall Recovery Gets Patient Back to Life and Movement
Standing at the top of the stairs to the basement Sharon Sturtevant was chatting with her grandson in the kitchen. Suddenly, Sharon stumbled and fell down the stairs. “The last thing I remember was my head hitting the floor before everything went black,” she recalls. Her grandson, Oliver, quickly called 911 and paramedics arrived on the scene, taking her by ambulance to Renown Regional Medical Center where she was diagnosed with a broken collarbone and a neck fracture that would require complex surgery involving fusion of her neck. Fall Recovery Begins After her surgery, Sharon was transported to the Renown Rehabilitation Hospital and her recovery process began. Sharon smiles as she describes the rehab hospital team “They are fabulous here, I learned so much about how my body moves, and the proper way to move it. At home I wouldn’t have known what to do,” she confesses. “They set me up for success to return home and not get injured again.” At Renown Rehabilitation Hospital, different therapists coordinated a custom plan to help Sharon recover from her injuries. Ultimately, the goal of her physical therapy was to help restore and improve her strength, reduce pain and increase her mobility for stamina and balance. Physical Therapy Key to Successful Treatment of Falls “My recovery after the operation was an eye-opener,” Sharon declares. “I had no idea how much went into regaining everyday moment.” During her rehabilitation hospital stay, she had to re-learn how to swallow, go up and down stairs, as well as successfully get in and out of a wheelchair, which involved transferring her body weight safely. Due to hormonal changes after menopause women are 50% more at risk for falls than men, according to research. Sharon now has a greater awareness of how to move her body and is significantly stronger than before entering her physical rehabilitation sessions. Not everyone knows that everyday mobility is impacted by four basic skills: stepping, trunk flexibility, upright posture and weight shifting. “I don’t know how I could have gotten this far without the wonderful therapists here,” she shares. “They are so thorough. Proper alignment was encouraged helping me to walk and stand correctly. They were all so nice and patient with me,” she states. “I actually had less pain because I didn’t hurt myself moving the wrong way.” Falls Are Common Among Aging Adults As we age balance becomes more important. Unfortunately falls are common among older adults with negative quality of life effects, even fatalities. According to the Centers for Disease Control and Prevention (CDC), one in four seniors fall each year in the U.S. A comprehensive physical therapy plan for sudden falls or chronic conditions is a safe, effective alternative treatment to medication such as opioids. Today Sharon is back at home with a new banister installed on the basement stairs. As a music lover she is enjoying her musical grandchildren Oliver and Eliana who play instruments. She looks forward to attending their upcoming school concerts. Sharon remembers the staff at Renown Rehabilitation Hospital fondly, “They were unfailingly patient, supportive, informative and understanding.” Her advice to those unexpectedly finding themselves in the rehabilitation hospital is, “Listen to your therapists carefully and follow their instructions.”
Read More About Fall Recovery Gets Patient Back to Life and Movement
-
Bone Fractures in Children Honest Expert Advice
Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis, answers some common questions about bone fractures. Is there a difference between broken bones and fractures? No, these are two different names for the same injury. Of course the common term is a broken bone. Using either name will describe your concerns. Medical personnel typically describe a broken bone as a fracture to a specific bone. For example, a broken wrist is also a fractured distal radius. To clarify, this describes the injured bone and the precise location. How do I know if my child has broken their bone? Many times children will fall and complain of their arm or leg hurting. In most cases the pain goes away and the child will return to their activities. When there is a deformity to the limb (curve in arm) and the child is complaining of pain, it is probably a fracture. If the arm or leg looks straight, look to see if there is any swelling or bruising. Both are signs of a possible fracture. Finally, if the limb looks normal but the child continues to complain, gently push on the bone. Likewise if it causes the same pain, then they likely have a fracture and should have an x-ray. My child fractured their growth plate, what does this mean? Growth comes from this area of the bone. In detail, these are located all over the body but typically at the end of the bones. With this in mind, fractures to these areas can result in the bone growing abnormally. Because of potential shortening of the arm or leg, or bones growing crooked, it is important to follow fractures closely (up to 1-2 years or longer). It is better to identify a problem early. Small problems can be treated with small surgeries. What if the bones of the x-ray do not line up? Because children are growing, unlike adults, their bones will remodel and straighten with growth. The amount of remodeling occurring depends on a child’s age, the bone fractured and the location. In many cases an angled bone will grow straight over the course of a year. For this reason, someone with experience in caring for children needs to follow bone growth. How long does it take fractures to heal? Factors deciding when a cast can come off include: Child’s age. Bone fractured. Fracture location. Young children heal faster than teens, teens heal faster than young adults, who heal faster than older adults. In young children most fractures heal in 4-6 weeks. However, teens generally take 6 weeks to heal, and adults can take much longer. Although your child is out of their cast, it may not be healed completely to return to all activities. Placing a splint is during this time is common. This typically gives them added protection for several weeks after their cast is removed - in case they forget their limitations. What if my child is still limping? Whether a child is in a walking or non-weight bearing cast, removing it often leaves them stiff and sore. Therefore many children will walk as though they still have a cast in place. In most cases this resolves in about three weeks. Regardless, if your child is still limping or walking abnormally after three weeks, contact the treating doctor. They may benefit from physical therapy or a repeat evaluation. (This article was original published in the July 2019 issue of South Reno Kids & Sports.)
Read More About Bone Fractures in Children Honest Expert Advice