Search
-
-
11Jun
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
10Dec
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
13Aug
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
10Sep
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
9Jul
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
12Nov
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
-
8Oct
Renown Institute for Heart & Vascular Health proudly offers the free Cardiovascular Support Group. Please join us if you or anyone you know has been diagnosed with cardiovascular issues. Meet and get to know the Cardiovascular Quality Team from the Renown Institute for Heart & Vascular Health on the second Tuesday of every month from 2-3 p.m. This group is open to all cardiovascular patients and their families. Learn about managing and living with cardiovascular issues in a supportive group environment. Virtual attendees will receive instructions on how to join the meeting the day before the event. Complimentary refreshments and informative materials will be provided!
Read More About Cardiovascular Support Group
-
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Fall Recovery Gets Patient Back to Life and Movement
Standing at the top of the stairs to the basement Sharon Sturtevant was chatting with her grandson in the kitchen. Suddenly, Sharon stumbled and fell down the stairs. “The last thing I remember was my head hitting the floor before everything went black,” she recalls. Her grandson, Oliver, quickly called 911 and paramedics arrived on the scene, taking her by ambulance to Renown Regional Medical Center where she was diagnosed with a broken collarbone and a neck fracture that would require complex surgery involving fusion of her neck. Fall Recovery Begins After her surgery, Sharon was transported to the Renown Rehabilitation Hospital and her recovery process began. Sharon smiles as she describes the rehab hospital team “They are fabulous here, I learned so much about how my body moves, and the proper way to move it. At home I wouldn’t have known what to do,” she confesses. “They set me up for success to return home and not get injured again.” At Renown Rehabilitation Hospital, different therapists coordinated a custom plan to help Sharon recover from her injuries. Ultimately, the goal of her physical therapy was to help restore and improve her strength, reduce pain and increase her mobility for stamina and balance. Physical Therapy Key to Successful Treatment of Falls “My recovery after the operation was an eye-opener,” Sharon declares. “I had no idea how much went into regaining everyday moment.” During her rehabilitation hospital stay, she had to re-learn how to swallow, go up and down stairs, as well as successfully get in and out of a wheelchair, which involved transferring her body weight safely. Due to hormonal changes after menopause women are 50% more at risk for falls than men, according to research. Sharon now has a greater awareness of how to move her body and is significantly stronger than before entering her physical rehabilitation sessions. Not everyone knows that everyday mobility is impacted by four basic skills: stepping, trunk flexibility, upright posture and weight shifting. “I don’t know how I could have gotten this far without the wonderful therapists here,” she shares. “They are so thorough. Proper alignment was encouraged helping me to walk and stand correctly. They were all so nice and patient with me,” she states. “I actually had less pain because I didn’t hurt myself moving the wrong way.” Falls Are Common Among Aging Adults As we age balance becomes more important. Unfortunately falls are common among older adults with negative quality of life effects, even fatalities. According to the Centers for Disease Control and Prevention (CDC), one in four seniors fall each year in the U.S. A comprehensive physical therapy plan for sudden falls or chronic conditions is a safe, effective alternative treatment to medication such as opioids. Today Sharon is back at home with a new banister installed on the basement stairs. As a music lover she is enjoying her musical grandchildren Oliver and Eliana who play instruments. She looks forward to attending their upcoming school concerts. Sharon remembers the staff at Renown Rehabilitation Hospital fondly, “They were unfailingly patient, supportive, informative and understanding.” Her advice to those unexpectedly finding themselves in the rehabilitation hospital is, “Listen to your therapists carefully and follow their instructions.”
Read More About Fall Recovery Gets Patient Back to Life and Movement
-
Don’t Put Your Bladder Health on Hold
Millions suffer from urinary incontinence (urine leakage). Often people feel as if their bladders control their lives. But this doesn't have to be your story. Bladder control issues are treatable and you can take steps to help control your bladder. What is urinary incontinence? Men and women of all ages can have difficulty controlling their bladders. Urinary incontinence occurs when the muscles in the bladder that control the flow of urine contract or relax involuntarily. Is there more than one type of urinary incontinence? Yes, there are three main types: Stress incontinence is when the bladder leaks small amounts of urine as a result of physical stress or pressure on the muscles supporting the bladder caused by coughing, sneezing, laughing, lifting or any sudden physical exercise such as running or jumping. Urge incontinence is the inability to control a strong urge to go without advance warning, limiting the time needed to get to the bathroom. Overflow incontinence occurs when the bladder does not empty properly. As a result, over time, large quantities of urine are stored, causing the bladder to overflow (this is more common in men and is often the result of an enlarged prostate blocking the bladder opening). Are there any tests that can determine the cause and type of incontinence? Your doctor may have you track your fluid intake and output in a Bladder Diary. A urinalysis can be checked for infection, traces of blood, or other abnormalities. Blood tests can look for chemicals or substances that may relate to contributing causes. Other testing may be an ultrasound, cystogram or post voiding residual measurement. How is urinary incontinence treated? Exercises to strengthen the pelvic floor muscles or restrain the bladder to hold on for longer. Medication can relieve and control the troublesome symptoms. If there is an infection an antibiotic is used. Surgery can repair weakened muscles or remove blockage. Special products such as pants, pads, collection devices, and chair and bed protection may be needed if the problem cannot be controlled. How do you strengthen your pelvic floor muscles? To make your pelvic floor muscles stronger, alternate between squeezing and relaxing them. Following the steps below may help: Squeeze your muscles for one second and hold. Relax your muscles for two seconds. Each time you squeeze and relax, it counts as one set. Complete five sets. When you can do the exercises easily, increase to doing them 10 times per day. When that gets easy, try to squeeze and hold the muscles for three seconds and then relax the muscles for three seconds. As your pelvic muscles get stronger, you can progress to longer squeezes for about 10 seconds. Be sure to relax between squeezes so that your muscles can rest before squeezing again. You should do these exercises in three different positions. Do 10 sets lying down, 10 sitting and 10 standing. It is important that you develop the habit of doing the exercises every day. You may want to exercise just after you get up in the morning and right before you go to bed at night. What can I do to help control incontinence? Watch your weight, practice pelvic floor muscle exercises, eat plenty of fresh fruits, vegetables and fiber to prevent constipation. Most importantly, talk to your doctor regarding incontinence issues, don’t be embarrassed!
-
Your 9-Step Guide to Prevent Falls
According to the Centers for Disease Control and Prevention (CDC), one out of four adults aged 65 or older, fall each year. But less than half of those who fall talk to their healthcare provider about it. What’s more, among older adults, falls are the leading cause of both fatal and nonfatal injuries. Senior Care Plus, a Medicare Advantage Plan by Hometown Health, and Renown Health Nurse Educator, Nicholas Mannering, worked together to provide a list with simple tips to help you prevent falls. 1. Exercise Exercise strengthens both your muscles and bones and improves balance which is a key factor to preventing falls. The stronger you are, the less likely you are to fall. And, if you do fall, you are less likely to be injured. 2. Vision Check Vision is an import part of fall prevention, have your eyes check by an eye doctor at least once a year. Update your vision prescription and replace your eyeglasses as needed. 3. Install Safety Equipment in Your Bathroom Installing grab bars in your home bathroom provides a way for you to help yourself in and out of challenging situations. It also provides support if you suddenly feel week or unstable. Having a grab bar to lean on or hold onto when you feel yourself falling or slipping can help prevent falls. Rubber mats eliminate slick surfaces that increase your risk of falling. 4. Helpful Items in Your Bedroom A light within reaching distance is an important item to have in your bedroom. One reason adults fall is because they wander through a dark room, often to get to the bathroom at night, and can’t see where they are walking. Having a light within reach that is quick and easy to turn on before walking around a room can make it safer and decrease your risk of falling. Having a bedroom that is organized and furnished in a way that is easy to navigate is also important. If your bedroom is cluttered and hard to walk around without tripping or running into things, it might be worth reorganizing the area to define a clear walking path. 5. Helpful Items in Your Living Room Similar to your bedroom, your living room should have a light that is easily accessible. Sofas with armrests are helpful for support when getting up and sitting down. Avoiding clutter in your walkways, rugs that are not secured down and unstable furniture are important to consider when preventing falls. 6. Actions to Avoid in Your Home There are other ways to fall besides slipping or tripping while walking. Never stand on chairs, boxes or other unstable items in your home. Walkways should be tidy and free of objects that you could trip on. Spills should be cleaned up right away to prevent slipping. 7. Wear Appropriate Footwear Wearing shoes with non-slip soles and closed toes can help prevent you from falling. Having shoes that fit properly, are made from hard rubber (like tennis shoes) and provide good support help prevent tripping and falling. Shoes with a collar that support the ankle and a well-padded tongue for the top of your foot can also help prevent injury to your feet. 8. Review Your Health & Medications at your Annual Health Check-Up It is important to review your health and medications with your healthcare provider so they can assess if you are at risk for falls. You should discuss your vision, heart health and blood pressure at your annual health check-up. These things can play a role in the risk of falling. Reviewing your current medications is also important. If medications are making you dizzy, talk to your provider about adjusting the dosage so you can feel more stable and balanced. When talking to your doctor about medications be sure to include your vitamins and supplements. Finally, Have your healthcare provider check your feet and discuss proper footwear yearly. 9. Avoid Smoking and Alcohol Balance is important in preventing falls. Alcohol consumption negatively affects balance and increases your risk for falls and fractures. It also increases your risk for cancer, liver damage, osteoporosis, high blood pressure and strokes. Smoking is connected to frailty in older adults. It prevents the development of muscle tissue and breaks down healthy muscle tissue due to the lack of oxygen in your body.
-
3,000 Miles Away But Close to Home
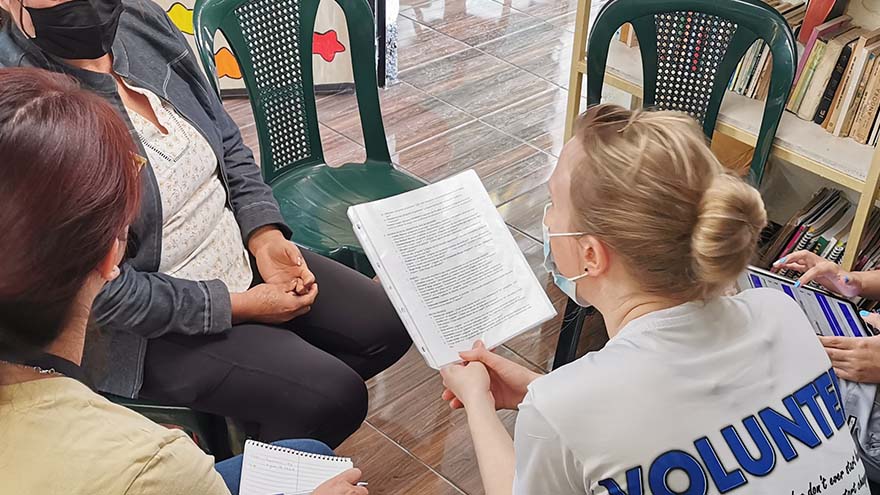
Overcoming poverty is not a task of charity, it is an act of justice. Like slavery and apartheid, poverty is not natural. It is man-made and can overcome by the actions of human beings. Sometimes it falls on a generation to be great. You can be that great generation. Let your greatness bloom. – Nelson Mandela, February 2005, Make Poverty History Campaign in London Lifting away the curtain that symbolized the front door, I entered a dark, cinderblock room and instantly became overwhelmed by an unpleasant odor. Working with oncology patients as a Child Life Specialist and an Occupational Therapist for over ten years, I recognized that smell. I had arrived in Guatemala – more than 3,000 miles from Reno – and it was my first day of a week-long trip where I would be serving alongside physicians in low-income communities providing free medical care for residents. My name is Brittany Jemmoua, I am an occupational therapist at Renown, and I recently volunteered with Kalan Kuxtal, a non-profit Guatemalan organization. I served alongside physicians by providing free primary care mobile clinics and home visits. The care we provided focused on prevention, intervention, education and lifestyle/medication management as we partnered with local entities, such as fire stations, community centers and schools to transform hundreds of lives. Speaking in both English and Spanish, I collected patient intake information, performed exams, tested for diabetes, and collaborated on a diabetes research project focused on daily risk assessment. Beyond these tasks, I immersed myself in the culture and learned more from the Guatemalan people than I could have ever imagined. Similar to Renown, Kalan Kuxtal Operates with Community at its Core Kalan Kuxtal, a Mayan expression meaning “life guardian,” is different from other volunteer medical trip organizations, and I took home valuable insights and lessons from their way of life that I now consider daily in my practice at Renown. I expanded my knowledge about diabetes, hypertension, pharmacology, infectious diseases, pregnancy complication, vector-borne illness and tuberculosis. We conducted home visits for socially neglected populations rather than expecting everyone to come to our clinics. I found that being welcomed into people’s homes gives you a different lens in which to view how their medical diagnoses interact with living conditions, occupations, and quality of life. This is when I met Mercedes and her mom. Her mom, Ms. Valencia, had jaundice skin and a substantial Basal Cell Carcinoma aggressively protruding from her face that impacted eating, hearing, seeing, sleep and social interactions. This opportunity to serve within their home led to an important palliative care conversation that would have been missed had we stayed in the clinic. We combed the rural neighborhoods assessing people’s risk for diabetes, taking glucose tests and educating families about their next steps. Many individuals had uncontrolled diabetes and misunderstandings regarding basic health management strategies. At the end of the day, many people demonstrated feelings of empowerment by actively offering solutions regarding how they will manage their day-to-day glucose with diet and exercise. Small actions can lead to big changes, and in the long-term, these health actions can help them avoid medication costs and focus on affording basic life necessities, such as water and electricity. Kalan Kuxtal organized a cultural day that included going to local businesses and community leaders to learn more about how they support the people of Guatemala. For example, Valhalla Macadamia Farm’s main goal is to help communities gain access to income, employment, and improved wellbeing by donating macadamia trees to families to grow and then sell macadamia products. A Weeklong Trip with Lifelong Impacts Each patient made a lasting impact on me, both personally and professionally. One specific family I saw in the clinic had a unique situation in that their two-year-old daughter, Margareth Elizabeth Cifuentes Bautista, was laboriously diagnosed with irregular corneal syndrome associated with glaucoma of congenital origin. Due to Guatemala’s limited prenatal screens and interventions, Elizabeth is nearly blind. While highly spirited and happy, she trips, bumps and feels her way through life. One barrier to her healthcare access is that her hard-working parents remain well below the poverty line, making less than $900/month. I am working to connect them with generous US Ophthalmologists and pediatric eye specialists to explore how we might save her sight and help her family. Their biggest dream is that she could recover her eyesight. “I know that this is not a life-threatening situation, but it is still something that never stops hurting me,” Jorge Cifuentes, Elizabeth’s father, said. “Unfortunately, our situation here is very hard. This country [Guatemala], although beautiful, it is very difficult to get ahead. We are people living in underprivileged conditions which complicates our situation even more. However, we are still trying to thrive by being kind and hardworking people. Thank you for helping us.” I have had the privilege of an opportunity for education, access to healthcare, employment and am aware that inequity and injustice prevail. This experience reinforced my understanding that medicine is a physically and mentally demanding profession that requires a commitment to service, continuous learning and adaptation both on local and global scales. I encourage everyone to please join me in serving the underserved by volunteering. Brittany is an experienced Occupational Therapist at Renown and volunteers with Kalan Kuxtal and other entities, such as The Robert Unsworth Foundation and Rock Steady Boxing to elevate communities. She loves being an Occupational Therapist; however, her life experiences confirm that her true calling is to become a physician. She is currently applying to medical school. Brittany is eager to earn the responsibility to improve lives and communities as their engaged physician. Brittany is tentatively scheduled to return to Guatemala at the end of this year to continue partnering with the people for a better future. You are welcome to join!