Search
-
-
12Dec
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. If you have questions about this workshop, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
-
15Aug
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. If you have questions about this workshop, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
-
20Jun
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. If you have questions about this workshop, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
-
10Oct
Space is limited for this event, and registration is required. This workshop is focused on understanding and completing a Nevada Durable Power of Attorney of Healthcare, also known as an Advance Directive. What to expect: A brief presentation about the document, its contents and purpose. Time for questions. Staff will be on hand to assist with document completion. A notary will be present for notarization. Participants may have their document uploaded into their Renown electronic medical record and/or submitted to the Nevada Living Will Lockbox on their behalf. Please come prepared with names, addresses, and phone numbers of those you want to appoint in the document and a photo ID if notarization is desired. All required paperwork will be provided by our staff. If you have questions about this workshop, please call Jessica Elmore, LMSW at 775-982-5098. There is no charge to attend this workshop.
Read More About Advance Directive Workshop
-
-
Here's How to Commemorate National Healthcare Decision Day
National Healthcare Decision Day is forthcoming. Here’s an easy and free way to commemorate the occasion: openly discussing how we want to be cared for at the end of our lives. Join Renown Health’s experts at a workshop about making decisions about an advance directive. Among the random national holidays, this one has significance: April 16 is National Healthcare Decision Day. And experts agree that the best time to discuss your views about end-of-life care and to learn what choices are available is before a life-limiting illness or crisis occurs. By preparing in advance, you can help reduce the doubt and anxiety related to decision making for your family if you cannot speak for yourself. “Completing your advance directive is a gift you give your family,” says Mary-Ann Brown, RN, MSN, director of Palliative Care. “The stress associated with these difficult decisions is decreased if everyone knows what is important to you and what you want the end of life.” What Are Advance Directives? An advance directive is a document that states your choices about medical treatment and names another person to make medical decisions on your behalf if you are unable to. This document allows you to make legally valid decisions about future medical care. Find more information about advance directives and the form online. The Conversation The first step in completing an Advance Directive is to think about what’s important to you and talk to your loved ones. The Conversation Project provides helpful tools to guide you and your family through this challenging topic. Getting this information together will help you fill out and complete your advance directives. Some things to consider and discuss with your family include: When you think about the last phase of your life, what’s most important to you? Who do you want involved in your care? Who should make decisions on your behalf if you’re not able to? Where do you want or not want to receive care? Are there specific treatments you would or would not want? Complete Your Advance Directive Planning In order to complete an advance directive, you will need either two witnesses or a notary to sign the form. Be sure to note restrictions on the witness process. When an advance directive is complete, you should keep the original. Copies should be given to your agent named in the form, your family, your doctor(s) and the location that you receive care. Renown Health offers four advance directive workshops every month to cover the details of filling out this document. A healthcare team is available to answer questions and work through the process with you. A notary is also present to finalize the process, which means you can complete your advanced directives during this workshop. Find the workshop by calling 775-982-RSVP for more information. Advance Care Planning Workshop April 17, 1-2:30 p.m. | Free Join Renown Health’s experts for a workshop about making decisions regarding end-of-life care. You will learn how to fill out an advance directive, receive one-on-one assistance and have your documents signed by a notary. Workshops are typically held several times each month. To RSVP, call 775-982-7787
Read More About Here's How to Commemorate National Healthcare Decision Day
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Making Patient Safety the Priority It Deserves to Be
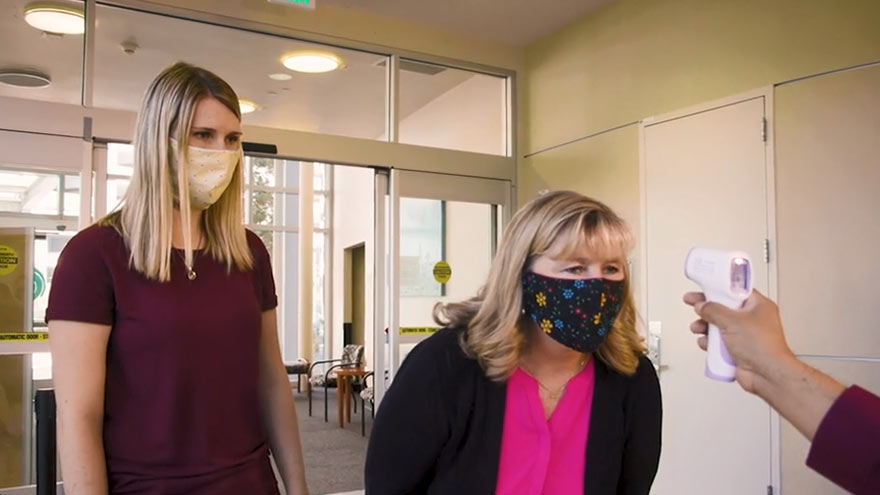
I am regularly amazed by medical advancements and innovation in the United States. However, even as we make significant progress in many areas of medicine, there is still much more work to be done in others. One such area is patient safety. What is Patient Safety? When we talk about patient safety, we are discussing how hospitals and healthcare organizations protect patients from errors, injuries and infections. Anyone can make a mistake at work, but in healthcare these mistakes can result in serious outcomes. In 1999, the Institute of Medicine released a report that estimated 98,000 deaths per year result from medical examination or treatment. The most recent study in 2013 suggested these numbers could range from 210,000 to 440,000 deaths per year. Many of these deaths result from preventable medical errors. This is inexcusable and shows how much more work our industry still needs to do to improve patient safety. Making Patient Safety a Priority Patient Safety is our number one priority at Renown Health. We dedicate a lot of time to establishing, reviewing, and revising our processes to prevent errors. Despite the obvious importance of patient safety, this issue is largely left to individual hospitals and health systems to manage. There is a surprising lack of national attention around this truly important issue. However, a silver lining of the COVID-19 pandemic is that it is igniting interest in hygiene and infection prevention. Patients want to learn more about the processes that are in place to prevent the spread of infections. In addition to the many protocols that guide our treatment of injuries and illness, Renown Health has implemented the following measures to prevent the spread of communicable diseases: Requiring everyone entering Renown sites to wear a mask or face covering. Establishing new processes to help patients and visitors practice social distancing. Limiting the number of visitors in our facilities. Screening all employees and patients for symptoms. Enhancing our already-thorough cleaning and disinfection processes. I hope patient safety and infection prevention remain in the national spotlight long after the COVID-19 pandemic has ended. The healthcare industry must come together to develop stronger systems and regulations to minimize preventable medical errors. We have a responsibility to our patients to do better.
Read More About Making Patient Safety the Priority It Deserves to Be
-
Addressing the Threat of Workplace Violence in Hospitals
In recent years, workplace violence against healthcare workers has been on the rise. According to the Occupational Safety and Health Administration (OSHA), about 75 percent of nearly 25,000 reported annual workplace assaults occur in healthcare and social service settings. Those who don’t work in healthcare may be surprised to learn that violent altercations are so common in our field. Hospital settings can create fear and stress for patients and their families. Pain, mind-altering medications and drugs, and difficult prognoses can amplify these feelings. While inappropriate responses may be understandable, violence cannot be tolerated. As the leader of a health system, protecting our employees is an issue that I take seriously. Reporting Workplace Violence Unfortunately, sometimes employees don’t report dangerous incidents fearing they might be blamed, or not realizing it’s a reportable offense. At Renown Health, we take these events seriously. We have clear, mandatory policies and protocols for reporting and investigating violent incidents. Each incident is investigated to ensure follow through and accountability. We also teach de-escalation skills to our hospital security teams, clinicians, and other frontline employees. As an added layer of protection, Renown Health has a first-rate security team that closely monitors activity on our campuses, addressing potential issues before they escalate. Our organization values our partnerships with community organizations including local law enforcement agencies like the Washoe County Sheriff’s Office and the Reno Police Department. Renown Health maintains a close relationship with these partners, and we alert them when our care teams experience an increase in violent incidents. I also recognize that workplace violence is a national problem that demands collaborative solutions. That’s why I am also proud to serve as a member of the American Hospital Association’s Hospitals Against Violence Advisory Committee. Nurses, doctors, paramedics, and frontline health workers care for us every day. It’s our responsibility to support them by ensuring they feel safe at work.
Read More About Addressing the Threat of Workplace Violence in Hospitals
-
Estate Planning Mistakes to Avoid
August is National Make-a-Will month. We talked to Renown Health Foundation Planned Giving Officer, Abbey Stephenson, to learn more about wills, trusts, and estate plans and why you should feel motivated this month to get started. Did you know that 2/3 of Americans don't have a will or trust? If this is you, don’t worry, you’re not alone. Although there are laws in place to determine who inherits your assets if you die without a will or trust, having a will or trust ensures your assets go where you want them to go after you are gone. They can also help minimize disputes between family members and heirs about who gets what. In Nevada, the laws that govern who gets what if you die without a will or trust can be found in Chapter 134 of the Nevada Revised Statutes. There are other documents that people often prepare at the same time as their will or trust – like an advance health care directive and durable power of attorney for assets. These documents all together are called an estate plan. Although they have other purposes too (like nominating a guardian for a child, planning for disability or avoiding probate, which is a court process), wills and trusts are documents that say who will receive your assets after you are gone. The most common type of trust is often called a revocable living trust or a family trust. People who have a trust usually still have a will, although it is a shorter form of will called a pour-over will. It’s a good idea to talk to an estate planning attorney about whether or not a trust makes sense for your family or circumstances. Now that you’re ready to get started, here are some mistakes to avoid: 1. Failing to plan Not setting aside the time to plan may be the biggest mistake. Failing to prioritize preparing or updating your estate plan means your last wishes and desires may not be fulfilled. The right documents memorialize what you would like to happen upon your disability and death so that other people can know and follow your wishes with respect to your care and your assets. 2. Failing to coordinate beneficiary designations Certain types of assets like life insurance and retirement accounts are not covered by your will or trust and need to be addressed separately. These types of assets are referred to as non-probate assets because they transfer under contract principles and don’t require court supervision or probate to be distributed to the named beneficiaries. By completing beneficiary designation forms provided by the retirement account custodian, insurance company or financial institution, you can direct your assets to one or more beneficiaries. 3. Failing to title your assets properly Asset titling refers to how you own your asset – such as in your individual name, jointly with someone else, or in a trust or entity. For example, assets titled for two people with a “right of survivorship” will automatically go to the surviving owner. Review your asset titling and make changes, if needed, to ensure your property and assets are passed down the way you intend. 4. Failing to include charities meaningful to you In addition to providing for family members and other important people in your life, you many also choose to give to charities meaningful to you in your estate plan. When you include a charity in your estate plan, that gift is called a planned gift and many charitable organizations, including Renown, recognize such donations through their legacy giving societies. As you prepare to make your own will or a more comprehensive estate plan, we recommend you consult with a lawyer. Here are some free resources that may be helpful too: Renown Health Foundation is proud to sponsor the Family Estate Planning Series put on by PBS Reno and the Community Foundation of Northern Nevada. The free, 8-week course of 90-minute, in-depth workshops is a great place to learn much more and to help you get started in the planning process. The next course begins on September 7, 2022. More information can be found here. Renown Health offers periodic advance health care directive workshops where attendees can learn about, complete, and sign their directive. The next workshop is scheduled for September 14th. More information can be found here. The American College of Trust and Estate Counsel provides information on a number of commonly asked estate planning questions here. If you are interested in including a charitable gift to Renown in your estate plan, we would be happy to talk to you about how your gift will make a difference for our mission. Please contact Abbey Stephenson at abbey.stephenson@renown.org or visit renown.org/LegacyGiving to learn about Renown Health Foundation’s Legacy Giving Society and ways to give.
-
What is Dry Drowning?
Whether you're a parent, grandparent, caregiver or sibling, you should know drowning is the second leading cause of death among children. Yet, while we are vigilant about protecting children from water accidents and drowning, a condition known as dry drowning or delayed drowning can go unnoticed. In fact, most people aren't even aware it exists. Dry drowning defined Dry drowning is a side-effect of a near-drowning experience and includes spasms of the vocal cords and larynx — known as a laryngospasm. This occurs when the body attempts to shut down the passage of any liquid into the lungs. Unfortunately, it can also shut down the passage of air into the lungs and force fluid into the stomach and lungs. Often the condition is not discovered until it's too late — severe cases can cause death within one to 24 hours after a water incident occurs. Who is susceptible? Novice or first-time swimmers are at increased risk, as are children with asthma and known breathing issues. In addition, children who have had pneumonia or experienced acute respiratory distress syndrome are also at greater risk. To reduce these factors, caregivers should be exceptionally watchful of inexperienced swimmers. According to Leland Sullivan, MD, of Northern Nevada Emergency Physicians, children under the age of 5 are most susceptible to drowning and often drown in residential swimming pools. Infants less than 1-year-old most often drown in bathtubs. What are the signs of a dry drowning episode? If your child has a near-drowning incident, a few moments of coughing until they calm down is normal. However, you should know the more severe signs and symptoms to watch for during the 24 hours following the incident, including: Persistent coughing Difficulty breathing and/or shortness of breath Chest pains Extreme fatigue and/or lethargy Change in typical behavior Face becomes pale What is the treatment and prognosis for dry drowning? Dr. Sullivan recommends that all victims of near-drowning incidents seek medical attention, even if they have no symptoms. If caught early, dry drowning can be treated. If you think your child is experiencing a dry drowning episode, go to the nearest emergency room as quickly as possible — do not attempt treatment at home. Healthcare professionals will work to supply oxygen to your child's lungs to restore and regulate breathing.
-
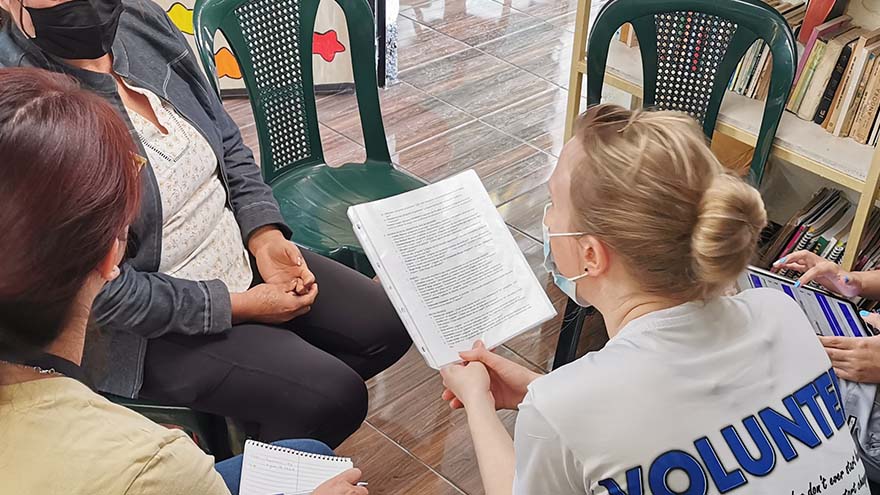
3,000 Miles Away But Close to Home
Overcoming poverty is not a task of charity, it is an act of justice. Like slavery and apartheid, poverty is not natural. It is man-made and can overcome by the actions of human beings. Sometimes it falls on a generation to be great. You can be that great generation. Let your greatness bloom. – Nelson Mandela, February 2005, Make Poverty History Campaign in London Lifting away the curtain that symbolized the front door, I entered a dark, cinderblock room and instantly became overwhelmed by an unpleasant odor. Working with oncology patients as a Child Life Specialist and an Occupational Therapist for over ten years, I recognized that smell. I had arrived in Guatemala – more than 3,000 miles from Reno – and it was my first day of a week-long trip where I would be serving alongside physicians in low-income communities providing free medical care for residents. My name is Brittany Jemmoua, I am an occupational therapist at Renown, and I recently volunteered with Kalan Kuxtal, a non-profit Guatemalan organization. I served alongside physicians by providing free primary care mobile clinics and home visits. The care we provided focused on prevention, intervention, education and lifestyle/medication management as we partnered with local entities, such as fire stations, community centers and schools to transform hundreds of lives. Speaking in both English and Spanish, I collected patient intake information, performed exams, tested for diabetes, and collaborated on a diabetes research project focused on daily risk assessment. Beyond these tasks, I immersed myself in the culture and learned more from the Guatemalan people than I could have ever imagined. Similar to Renown, Kalan Kuxtal Operates with Community at its Core Kalan Kuxtal, a Mayan expression meaning “life guardian,” is different from other volunteer medical trip organizations, and I took home valuable insights and lessons from their way of life that I now consider daily in my practice at Renown. I expanded my knowledge about diabetes, hypertension, pharmacology, infectious diseases, pregnancy complication, vector-borne illness and tuberculosis. We conducted home visits for socially neglected populations rather than expecting everyone to come to our clinics. I found that being welcomed into people’s homes gives you a different lens in which to view how their medical diagnoses interact with living conditions, occupations, and quality of life. This is when I met Mercedes and her mom. Her mom, Ms. Valencia, had jaundice skin and a substantial Basal Cell Carcinoma aggressively protruding from her face that impacted eating, hearing, seeing, sleep and social interactions. This opportunity to serve within their home led to an important palliative care conversation that would have been missed had we stayed in the clinic. We combed the rural neighborhoods assessing people’s risk for diabetes, taking glucose tests and educating families about their next steps. Many individuals had uncontrolled diabetes and misunderstandings regarding basic health management strategies. At the end of the day, many people demonstrated feelings of empowerment by actively offering solutions regarding how they will manage their day-to-day glucose with diet and exercise. Small actions can lead to big changes, and in the long-term, these health actions can help them avoid medication costs and focus on affording basic life necessities, such as water and electricity. Kalan Kuxtal organized a cultural day that included going to local businesses and community leaders to learn more about how they support the people of Guatemala. For example, Valhalla Macadamia Farm’s main goal is to help communities gain access to income, employment, and improved wellbeing by donating macadamia trees to families to grow and then sell macadamia products. A Weeklong Trip with Lifelong Impacts Each patient made a lasting impact on me, both personally and professionally. One specific family I saw in the clinic had a unique situation in that their two-year-old daughter, Margareth Elizabeth Cifuentes Bautista, was laboriously diagnosed with irregular corneal syndrome associated with glaucoma of congenital origin. Due to Guatemala’s limited prenatal screens and interventions, Elizabeth is nearly blind. While highly spirited and happy, she trips, bumps and feels her way through life. One barrier to her healthcare access is that her hard-working parents remain well below the poverty line, making less than $900/month. I am working to connect them with generous US Ophthalmologists and pediatric eye specialists to explore how we might save her sight and help her family. Their biggest dream is that she could recover her eyesight. “I know that this is not a life-threatening situation, but it is still something that never stops hurting me,” Jorge Cifuentes, Elizabeth’s father, said. “Unfortunately, our situation here is very hard. This country [Guatemala], although beautiful, it is very difficult to get ahead. We are people living in underprivileged conditions which complicates our situation even more. However, we are still trying to thrive by being kind and hardworking people. Thank you for helping us.” I have had the privilege of an opportunity for education, access to healthcare, employment and am aware that inequity and injustice prevail. This experience reinforced my understanding that medicine is a physically and mentally demanding profession that requires a commitment to service, continuous learning and adaptation both on local and global scales. I encourage everyone to please join me in serving the underserved by volunteering. Brittany is an experienced Occupational Therapist at Renown and volunteers with Kalan Kuxtal and other entities, such as The Robert Unsworth Foundation and Rock Steady Boxing to elevate communities. She loves being an Occupational Therapist; however, her life experiences confirm that her true calling is to become a physician. She is currently applying to medical school. Brittany is eager to earn the responsibility to improve lives and communities as their engaged physician. Brittany is tentatively scheduled to return to Guatemala at the end of this year to continue partnering with the people for a better future. You are welcome to join!
-
Plan Early: Completing Your Advance Directive
We plan for the birth of a child, weddings and retirement, but rarely do we discuss how we want to be cared for at the end of our lives. Getting through this challenging conversation and completing an Advance Directive can give you peace of mind that your loved ones will not have to make difficult choices on your behalf. The best time to complete an Advance Directive is now – don’t wait until a life-limiting illness or crisis occurs to discuss your views about end-of-life care and to learn what choices are available. By preparing in advance, you can help reduce the doubt and anxiety related to decision-making for your family if you cannot speak for yourself. What are Advance Directives? An Advance Directive is a document that states your choices about medical treatment and names another person to make medical decisions on your behalf if you are unable to. This document allows you to make legally valid decisions about future medical care. “Completing your Advance Directive is a gift you give your family,” says Director of Palliative Care, Mary-Ann Brown RN, MSN. “The stress associated with these difficult decisions is decreased if everyone knows what is important to you and what you want at the end of life.”
Read More About Plan Early: Completing Your Advance Directive