Search
-
Foods to Avoid When Taking Heart Medications
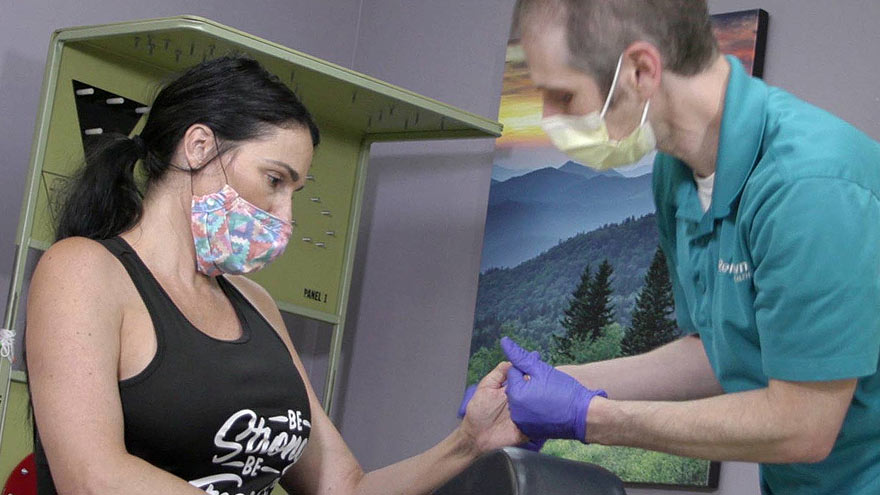
Did you know certain medications can interact with everyday food and drink? We asked Pharmacy Manager Adam Porath how to take these important medications safely. One in five Americans between the ages of 40 and 75 are currently taking a statin drug to reduce their cholesterol level or to prevent atherosclerosis (hardening of the arteries). Many others also take anticoagulants (blood thinners) to prevent blood clots from forming, which can increase the risk of stroke. Adam Porath, pharmacy manager with the Renown Institute for Heart and Vascular Health’s Anticoagulation Program, explains how to safely take these medications. What is a statin? A statin is a drug that can lower cholesterol by helping your body absorb cholesterol or by blocking a substance your body needs to make it. The American Heart Association cites a global study reporting the benefit of statins to help reduce heart attacks and strokes. Common statins include atorvastatin (Lipitor), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor). Which foods or drinks should be avoided while taking statin drugs? Grapefruit juice is the only food or drink that has a direct interaction with statins. Statins do not directly interact with any food but people taking statins should moderate their intake of saturated fats to help lower their LDL cholesterol and overall risk of cardiovascular disease. What is a blood thinning drug? Blood thinning drugs, such as warfarin, rivaroxaban (Xarelto), apixiban (Eliquis), dabigatran (Pradaxa) and edoxaban (Savaysa), are used to prevent stroke. Which foods or drugs should be avoided while taking blood thinning drugs? If taking warfarin, alcohol and cranberries (including juice) should be avoided. Patients taking warfarin should be aware of foods that contain Vitamin K (green leafy vegetables) and try to maintain a consistent diet of these foods. Warfarin interacts with many over the counter and prescription medications. Patients should consult a pharmacist when starting, stopping, or changing doses of any medication when taking warfarin. Also, patients taking any blood thinning medication should avoid over-the-counter pain relievers (i.e. aspirin, ibuprofen, etc.) How do I know whether to take my medication with food or not? Consulting with a pharmacist is the best resource to determine if a medication should be taken with or without food. In general, all statins and blood thinners can be taken with or without food. The only exception is Xarelto (rivaroxaban), which should be taken with the largest meal of the day If you are a Renown patient you can also review your prescriptions online, request a refill or ask a question via MyChart. With MyChart, you can access all your healthcare information securely 24/7.
Read More About Foods to Avoid When Taking Heart Medications
-
Stroke Survival as a Warrior – Kimi's Story
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Heart Attack Survivor Fights the Good Fight
Something wasn’t right. Even though it was the holiday season, on December 23, 2018, Mondo Corona didn’t feel good…not to mention his sudden earache. Although Christmas was a happy celebration with his family. He still felt tired. Was it the flu? And that darn earache wouldn’t go away. On that cool winter day, Mondo could not imagine he was near death. Or that he would become a heart attack survivor. Know Your Heart A few days later, on December 27, he wasn’t feeling any better. He decided to go to the emergency room at Renown Regional Medical Center. That’s when a simple blood test revealed shocking results. “I thought about death a lot. I was calling people to ask them to help take care of my family if I wasn’t going to be here anymore,” he emotionally confesses. Although Mondo loves his job as a railroad engineer, it involves on-call shifts and an erratic sleep schedule. At that time his exercise and eating habits weren’t the best either. Yet he never imagined he would have a massive, often lethal, type of heart attack called ‘the widowmaker.’ In fact, his family had been concerned about his health for awhile. “He worked so much and he didn’t take care of himself and he didn’t exercise – he was burning the candle at both ends,” shares his wife, Alison. His daughter Justice, an avid exerciser, was always encouraging him to join her at the gym, but could never quite convince him. Mondo remembers the time before he became a heart attack survivor. “I didn’t have any exercise whatsoever in my life. At that point my eating habits were just terrible,” he shares. He went to the emergency room due to his earache, but nothing was found until one of the doctors ordered some tests. Specifically blood work showed high troponin levels. Troponin is a blood protein often released in large amounts when the heart muscle has damage, sometimes by a heart attack. Heart Attack Survivor “My surgeon came in and told us that it was going to be a triple bypass – that three of the four…major arteries were clogged 100 percent,” Mondo explains. Amazingly his heart was pumping on only 10 percent blood flow. Heart surgeon, Joseph Brandl, MD, told him he survived a widowmaker heart attack. This type of heart attack happens when there is a 100 percent blockage in the critical left anterior descending artery (LAD) of the heart. Frequently the symptoms can often be mistaken for the flu. According to the Centers for Disease Control and Prevention (CDC), every 40 seconds a person in the U.S. has a heart attack. And 1 in 5 heart attacks are “silent” – meaning you can be a heart attack survivor, but not know it. For Mondo’s children, seeing their strong father struggle after heart surgery was difficult. Justice tearfully shares, “It was really hard seeing him so vulnerable. He really needed anybody’s and everybody’s help at that point.” A Heart Attack Survivor Program After leaving the hospital on January 5, 2019, he was extremely weak. On February 12, Mondo began Renown Health’s Intensive Cardiac Rehabilitation (ICR) Program called the Healthy Heart Program. This program, requiring a doctor referral, includes 12 weeks of supervised exercise along with nutrition education and stress management skills. In spite of heart disease being the leading cause of death in the U.S. – more than all cancers combined, the risk can be lessened with daily lifestyle habits. Mondo credits the ICR program with motivating him and getting his focus back on his health. He saw the team members setting an example and also caring about his health. He describes one of his favorite recipes, “In ICR Sara showed us how to make this incredible fruit salad, with jicama, watermelon, grapes, oranges, red onion, and ginger!” Of course, the recovery process was not overnight. “It did take a long time to really realize that he was going to be back to normal, that he was going to be okay and that he was going to be that strong provider for me and my children,” Alison reflects. “Mondo’s had an amazing outcome and he’s not limited in his activities at all and should hopefully have a life that’s not limited at all from heart disease as we’re monitoring everything and everything’s looking good,” reports his heart doctor Jayson Morgan, MD. Mondo describes his care experience being a heart attack survivor as life-changing. “The care teams at both Renown and ICR were incredible. There wasn’t a single person we came across who didn’t immediately become a part of the family. They truly cared for us, all of us, including the extended family that came to visit. They were informative and supportive. I felt like I created lasting bonds with so many of them, especially the gang in ICR. What amazing people.” Lynice Anderson, Director of Intensive Cardiac Rehab, Healthy Heart Program, shares,” Mondo is one of the most genuine, thoughtful and humble people I have ever met. His love for his family is palpable. His impact on me personally and our team is forever.” She acknowledges family support is key to his success, “Mondo’s family is his rock and they are his. I have never met a family that was so ‘all in’ in the support of their loved one. His new heart healthy lifestyle is modeled through his family every day.” Fighting The Good Fight Of course, Mondo may look familiar to you. That’s because he is featured in Renown Health’s “Fight The Good Fight” brand campaign. For this reason, you may have seen him in advertising working out on a treadmill, shirtless, with his open heart surgery scar in full view. When asked how he feels about showing his scar he confidently says, “I don’t mind showing it to people. I don’t. I earned that scar.” He is a proud heart attack survivor. Today, he’s grateful to be alive and takes his health commitment seriously. “Things have a different feel now. The skies and lakes are bluer and the trees greener. My family is so much more a part of my day. We go on so many more outdoor adventures, trying to incorporate a little exercise into our fun. We watch what we eat more and are trying to teach our children and loved ones about healthy choices. And I think with a few we’ve even been successful!” he observes. “Don’t take life for granted.” “Unconditional love. I get nothing but support from my family without them I wouldn’t be where I’m at. What happened to me definitely makes me a fighter for sure. I’m fighting for my life – the good fight – I think life is good,” he adds.
-
Making Patient Safety the Priority It Deserves to Be
I am regularly amazed by medical advancements and innovation in the United States. However, even as we make significant progress in many areas of medicine, there is still much more work to be done in others. One such area is patient safety. What is Patient Safety? When we talk about patient safety, we are discussing how hospitals and healthcare organizations protect patients from errors, injuries and infections. Anyone can make a mistake at work, but in healthcare these mistakes can result in serious outcomes. In 1999, the Institute of Medicine released a report that estimated 98,000 deaths per year result from medical examination or treatment. The most recent study in 2013 suggested these numbers could range from 210,000 to 440,000 deaths per year. Many of these deaths result from preventable medical errors. This is inexcusable and shows how much more work our industry still needs to do to improve patient safety. Making Patient Safety a Priority Patient Safety is our number one priority at Renown Health. We dedicate a lot of time to establishing, reviewing, and revising our processes to prevent errors. Despite the obvious importance of patient safety, this issue is largely left to individual hospitals and health systems to manage. There is a surprising lack of national attention around this truly important issue. However, a silver lining of the COVID-19 pandemic is that it is igniting interest in hygiene and infection prevention. Patients want to learn more about the processes that are in place to prevent the spread of infections. In addition to the many protocols that guide our treatment of injuries and illness, Renown Health has implemented the following measures to prevent the spread of communicable diseases: Requiring everyone entering Renown sites to wear a mask or face covering. Establishing new processes to help patients and visitors practice social distancing. Limiting the number of visitors in our facilities. Screening all employees and patients for symptoms. Enhancing our already-thorough cleaning and disinfection processes. I hope patient safety and infection prevention remain in the national spotlight long after the COVID-19 pandemic has ended. The healthcare industry must come together to develop stronger systems and regulations to minimize preventable medical errors. We have a responsibility to our patients to do better.
Read More About Making Patient Safety the Priority It Deserves to Be
-
Parkinson's Disease Know The Important Symptoms
Parkinson’s disease – you may have heard of it because Neil Diamond and Ozzy Osbourne were recently diagnosed with it. Or perhaps you know Michael J. Fox is a strong advocate and funds research through his foundation. Neurologist Jonathan Spivack, MD, discusses this disease, while physiatrist Stephanie Jones, DO, explains how physical therapy can help as a supplemental treatment. According to the Parkinson’s Foundation about ten million people worldwide currently have this disease. What is Parkinson’s Disease? “Parkinson’s disease is a neurodegenerative disease that progresses slowly and definitely, though at variable rates,” explains Dr. Spivack. “Symptoms go beyond the classic motor changes. It results from a loss of specific dopamine-producing brain cells. Specifically, this loss is likely due to a mix of genetic and environmental factors,” he adds. Dopamine allows communication between particular nerve cells responsible for movement. If you have Parkinson’s dopamine levels gradually drop, causing a loss of motor skills. Generally, most patients with the disease are over age 65. Early Signs and Symptoms Diagnosing Parkinson’s can be difficult as some of the symptoms happen during the natural aging process. The Parkinson’s Foundation identifies the following 10 early signs of PD: Tremors or shaking of your hand, fingers or chin Small handwriting Loss of smell Sudden movements during sleep Stiffness when walking or moving Constipation Softer or lower voice volume Mad facial expression Feeling dizzy or faint Hunching or stooping posture A single sign may not point to the disease, but if you (or a loved one) has multiple signs, talk to your healthcare provider.
Read More About Parkinson's Disease Know The Important Symptoms
-
Addressing the Threat of Workplace Violence in Hospitals
In recent years, workplace violence against healthcare workers has been on the rise. According to the Occupational Safety and Health Administration (OSHA), about 75 percent of nearly 25,000 reported annual workplace assaults occur in healthcare and social service settings. Those who don’t work in healthcare may be surprised to learn that violent altercations are so common in our field. Hospital settings can create fear and stress for patients and their families. Pain, mind-altering medications and drugs, and difficult prognoses can amplify these feelings. While inappropriate responses may be understandable, violence cannot be tolerated. As the leader of a health system, protecting our employees is an issue that I take seriously. Reporting Workplace Violence Unfortunately, sometimes employees don’t report dangerous incidents fearing they might be blamed, or not realizing it’s a reportable offense. At Renown Health, we take these events seriously. We have clear, mandatory policies and protocols for reporting and investigating violent incidents. Each incident is investigated to ensure follow through and accountability. We also teach de-escalation skills to our hospital security teams, clinicians, and other frontline employees. As an added layer of protection, Renown Health has a first-rate security team that closely monitors activity on our campuses, addressing potential issues before they escalate. Our organization values our partnerships with community organizations including local law enforcement agencies like the Washoe County Sheriff’s Office and the Reno Police Department. Renown Health maintains a close relationship with these partners, and we alert them when our care teams experience an increase in violent incidents. I also recognize that workplace violence is a national problem that demands collaborative solutions. That’s why I am also proud to serve as a member of the American Hospital Association’s Hospitals Against Violence Advisory Committee. Nurses, doctors, paramedics, and frontline health workers care for us every day. It’s our responsibility to support them by ensuring they feel safe at work.
Read More About Addressing the Threat of Workplace Violence in Hospitals
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
A Family's Legacy
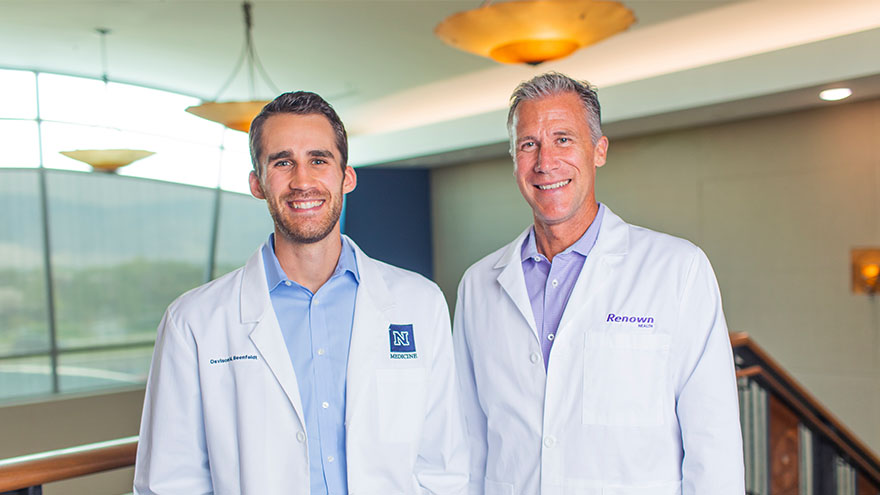
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school
-
The Road to Recovery Close to Home
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.
-
Reliable Care From Home
Renown Health has always been on the frontlines of technological advancement, and that innovation remained unwavering during the COVID-19 pandemic. Our telehealth teams heeded the call to provide home monitoring for our patients, transforming how we provide care. The care providers at Renown successfully monitored lower acuity COVID-19 patients from the comfort of their own homes. Bernard Lee was diagnosed with COVID-19 and pneumonia, and was able to return home to continue his recovery with a home monitoring system. While at home, Bernard’s health took a turn for the worse while he was sleeping, but thanks to the continuous monitoring of Health at Home, his worsening vitals did not go unnoticed. “This monitoring system really saved my life,” Bernard said. “It was telling me that my sats were low, but I didn’t even feel the common COVID symptoms; I just felt tired.” Because of his low oxygen saturation (sats) and the continuous monitoring, he woke up to providers calling to check on him in the early morning. He was immediately transferred to the Renown Intensive Care Unit to be cared for and monitored by our expert care teams. Today Bernard is recovering, feeling great and continuously refers to the team and the home monitoring system as his guardian angels.
-
Avoid Heat Exhaustion With This Simple Checklist
Young children under 4 and adults over 65 are especially vulnerable to heat exhaustion. Avoid heat exhaustion this summer with some expert tips. Northern Nevada summers can be downright hot, and although the balmy temperatures can feel great, they may cause heat-related illness, also known as heat exhaustion. Infants and children under 4 and adults over 65 are particularly vulnerable to heat exhaustion because their bodies adjust to heat more slowly. Without proper intervention, heat exhaustion can progress to heat stroke, which can damage the brain and other vital organs and even cause death. The Warning Signs of Heat Exhaustion Heavy sweating Elevation of body temperature Paleness Muscle cramps Tiredness, weakness, dizziness Headache Fainting Nausea or vomiting Cool and moist skin Fast and weak pulse Fast and shallow breathing Heat stroke happens when the body’s temperature rises rapidly and the body loses its ability to sweat. The Symptoms of Heat Stroke Body temperatures rising to 106 degrees or higher within 10 to 15 minutes Red, hot and dry skin (no sweating) Rapid, strong pulse Throbbing headache Dizziness or nausea Prevention and Treatment Make sure your air conditioner works Stay indoors and drink plenty of fluids Limit strenuous outdoor activities to mornings and evenings Drink plenty of water throughout the day Avoid caffeine and alcohol Do outdoor activities in the shade and wear light, loose clothing Take plenty of breaks and drape a wet bandanna around your shoulders to cool down If you suspect you or someone else is headed toward heat exhaustion or heat stroke, call 911 immediately.
Read More About Avoid Heat Exhaustion With This Simple Checklist
-
What is Dry Drowning?
Whether you're a parent, grandparent, caregiver or sibling, you should know drowning is the second leading cause of death among children. Yet, while we are vigilant about protecting children from water accidents and drowning, a condition known as dry drowning or delayed drowning can go unnoticed. In fact, most people aren't even aware it exists. Dry drowning defined Dry drowning is a side-effect of a near-drowning experience and includes spasms of the vocal cords and larynx — known as a laryngospasm. This occurs when the body attempts to shut down the passage of any liquid into the lungs. Unfortunately, it can also shut down the passage of air into the lungs and force fluid into the stomach and lungs. Often the condition is not discovered until it's too late — severe cases can cause death within one to 24 hours after a water incident occurs. Who is susceptible? Novice or first-time swimmers are at increased risk, as are children with asthma and known breathing issues. In addition, children who have had pneumonia or experienced acute respiratory distress syndrome are also at greater risk. To reduce these factors, caregivers should be exceptionally watchful of inexperienced swimmers. According to Leland Sullivan, MD, of Northern Nevada Emergency Physicians, children under the age of 5 are most susceptible to drowning and often drown in residential swimming pools. Infants less than 1-year-old most often drown in bathtubs. What are the signs of a dry drowning episode? If your child has a near-drowning incident, a few moments of coughing until they calm down is normal. However, you should know the more severe signs and symptoms to watch for during the 24 hours following the incident, including: Persistent coughing Difficulty breathing and/or shortness of breath Chest pains Extreme fatigue and/or lethargy Change in typical behavior Face becomes pale What is the treatment and prognosis for dry drowning? Dr. Sullivan recommends that all victims of near-drowning incidents seek medical attention, even if they have no symptoms. If caught early, dry drowning can be treated. If you think your child is experiencing a dry drowning episode, go to the nearest emergency room as quickly as possible — do not attempt treatment at home. Healthcare professionals will work to supply oxygen to your child's lungs to restore and regulate breathing.