Search
-
Prevent Osteoporosis: Take Control of Your Bone Health Today
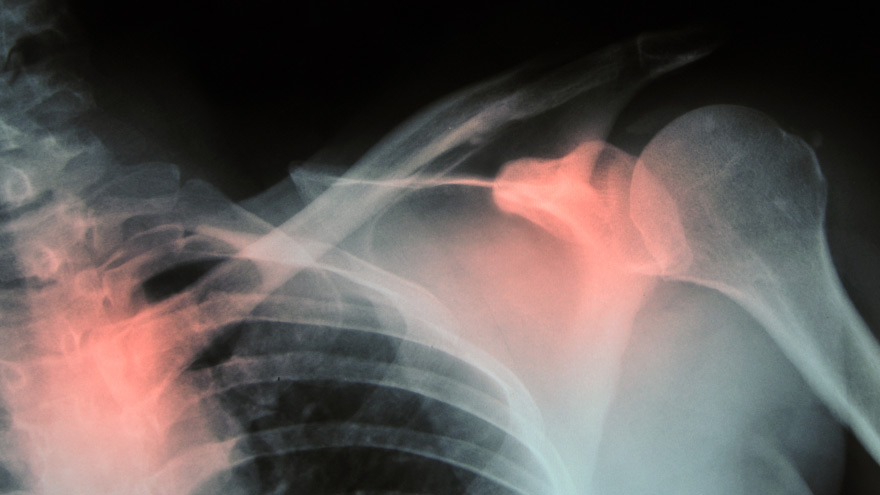
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
Ask the Expert: What is Scoliosis?
Posture is important, but for those children diagnosed with scoliosis (spinal curvature) it can be a difficult issue. The Washoe County School District Student Health Services Department screens 7th grade students for scoliosis as growth spurts often reveal the condition and, if diagnosed early, scoliosis can stop progressing. We asked Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis to answer some frequently asked questions about scoliosis. What is scoliosis? There are many types of scoliosis: early onset (occurs before age 10), congenital scoliosis is when the bones of the spine do not form correctly, neuromuscular scoliosis which is due to children’s neurologic and muscle disease, and the most common is Adolescent Idiopathic Scoliosis. The term “idiopathic “ means the exact cause is unknown, although we do know it runs in families. This type of scoliosis occurs in 2-3 percent of adolescents and is mainly seen during their growth spurt. This is why middle school screenings are recommended. Both genders get scoliosis but girls are 8 times more likely to have their curves progress and become larger. What are the signs that my child may have scoliosis? A few signs for parents to watch for are: One shoulder might be higher than the other. One leg may seem longer. A hip may be higher or look more prominent. The waist may not look the same from side to side (asymmetry). The trunk or rib cage may be more prominent on one side or shifted. When they bend forward they may have a bump on their back. How is scoliosis diagnosed? It can be noticed by a pediatrician at a physical, school screening nurse, PE teacher or parents. Once the curve is suspected the child is usually referred to a pediatric orthopedic surgeon scoliosis expertise. At the initial visit the doctor will perform a thorough physical including a complete neurologic exam to assess the amount of curvature. Once the exam is completed the physician will determine if a spinal x-ray is needed. The curve on the x-ray is measured utilizing the cobb angle (a measurement in degrees) which helps guide the treatment. What are common treatments for scoliosis? The treatment depends on the size of the spinal curve and the amount of growth the child has remaining. An x-ray of the child’s hand is used to determine the amount of growth remaining. This allows the determination of the child’s bone age, and based on the hands growth plates it can determined if the child is in their rapid phase of growth. Treatments include: Observation - For curves less than 20-25 degrees. This entails visits every 6-9 months with a repeat scoliosis x-ray. Since scoliosis curves increase only 1-2 degrees per month, and variations in measurements can be 3-5 degrees, an x-ray is not recommended before 6 months. If the curve remains less than 25 degrees the child is followed until their growth is completed (usually age 16-18). Progressing Curve - If growth is finished and the curve is less than 40 degrees, the risk of more curvature into adulthood is small. If growth is completed and the curve is over 45 degrees, the child is followed for several years as these curves can progress into adulthood. If the patient is still growing and the curve has progressed greater than 25 degrees but still in the non-operative range (less than 45-50 degrees) bracing is used to stop the progression of the curve. Bracing - Indicated for curves over 25 degrees but less than 45 degrees. If a brace is required you will be referred to an orthotist (bracing specialist). The orthotist assesses your child, reviews the x-ray and then fits the brace. (Having a brace made usually takes 2-3 weeks.) Once the brace is fit, your child will visit the scoliosis specialist for an x-ray in the brace to ensure it fits correctly. The primary goal of bracing is to halt progression of the curve and prevent the need for surgery. The brace must be worn for about 16 hours per day to be effective. In a recent bracing study 72% of the patients who wore their braces as prescribed prevented the need for surgery compared to the group who did not wear their brace. Surgery: When a curve reaches 45-50 degrees, and a child is still growing, surgery is usually recommended because the curve is likely to continue progress. If a curve is over 50 degrees and the child is done growing surgery also may be recommended. This is because when curves are over 50 degrees they tend to increase 1-2 degrees per year for the rest of your life. As curves get larger the amount of lung function tends to decrease which could cause breathing problems later in life. The goals of surgery are to stop the progression of the curve and safely correct any misalignment. This is accomplished by attaching implants (rods, screws, hooks and bands) to the spine. Bone graft is then placed around the implants to encourage the spine to fuse (grow together). This then forms a solid column of bone with metal rods in place, preventing the curve from changing. Most patients are back to their regular sports and activities six months post surgery.
-
Bone Fractures in Children Honest Expert Advice
Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis, answers some common questions about bone fractures. Is there a difference between broken bones and fractures? No, these are two different names for the same injury. Of course the common term is a broken bone. Using either name will describe your concerns. Medical personnel typically describe a broken bone as a fracture to a specific bone. For example, a broken wrist is also a fractured distal radius. To clarify, this describes the injured bone and the precise location. How do I know if my child has broken their bone? Many times children will fall and complain of their arm or leg hurting. In most cases the pain goes away and the child will return to their activities. When there is a deformity to the limb (curve in arm) and the child is complaining of pain, it is probably a fracture. If the arm or leg looks straight, look to see if there is any swelling or bruising. Both are signs of a possible fracture. Finally, if the limb looks normal but the child continues to complain, gently push on the bone. Likewise if it causes the same pain, then they likely have a fracture and should have an x-ray. My child fractured their growth plate, what does this mean? Growth comes from this area of the bone. In detail, these are located all over the body but typically at the end of the bones. With this in mind, fractures to these areas can result in the bone growing abnormally. Because of potential shortening of the arm or leg, or bones growing crooked, it is important to follow fractures closely (up to 1-2 years or longer). It is better to identify a problem early. Small problems can be treated with small surgeries. What if the bones of the x-ray do not line up? Because children are growing, unlike adults, their bones will remodel and straighten with growth. The amount of remodeling occurring depends on a child’s age, the bone fractured and the location. In many cases an angled bone will grow straight over the course of a year. For this reason, someone with experience in caring for children needs to follow bone growth. How long does it take fractures to heal? Factors deciding when a cast can come off include: Child’s age. Bone fractured. Fracture location. Young children heal faster than teens, teens heal faster than young adults, who heal faster than older adults. In young children most fractures heal in 4-6 weeks. However, teens generally take 6 weeks to heal, and adults can take much longer. Although your child is out of their cast, it may not be healed completely to return to all activities. Placing a splint is during this time is common. This typically gives them added protection for several weeks after their cast is removed - in case they forget their limitations. What if my child is still limping? Whether a child is in a walking or non-weight bearing cast, removing it often leaves them stiff and sore. Therefore many children will walk as though they still have a cast in place. In most cases this resolves in about three weeks. Regardless, if your child is still limping or walking abnormally after three weeks, contact the treating doctor. They may benefit from physical therapy or a repeat evaluation. (This article was original published in the July 2019 issue of South Reno Kids & Sports.)
Read More About Bone Fractures in Children Honest Expert Advice