Search
-
Prevent Osteoporosis: Take Control of Your Bone Health Today
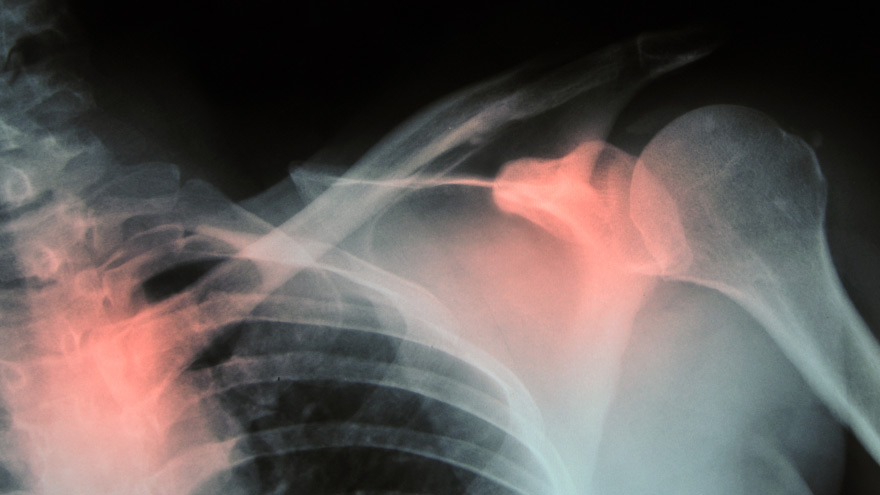
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
Get Moving: How to Exercise with Arthritis
An arthritis diagnosis doesn’t mean your exercise routine has to end. In fact, a consistent routine can actually improve mobility. Although stiff and painful joints can make it difficult to keep moving, staying active is essential for easing pain. October 11 is World Arthritis Day, so we asked Michelle Higgins, MPT at Renown Physical Therapy & Rehab some advice about exercising with arthritis. According to the Arthritis Foundation, arthritis affects one in five adults and 300,000 children. As a matter of fact arthritis is the nation’s leading cause of disability. Your joints certainly don’t need to suffer when you exercise. In general exercise is actually necessary for those with arthritis. Not only does it reduce joint pain, but it also increases strength and flexibility. Furthermore those adopting a regular exercise routine also have more energy, deeper sleep and find it easier to maintain a healthy weight. “Exercise is a necessary component to managing your arthritis,” says Higgins. “Consistent participation in an exercise program has been shown to promote long-term pain relief, increased body function and an improved quality of life. Alternatively, a lack of exercise can actually increase joint pain or stiffness and eventually lead to long term disability and suffering.” Exercising With Arthritis Exercise truly is the most effective non-drug arthritis treatment available for reducing pain and improving movement. And it can even include daily activities like gardening, dancing or walking your dog. Of course talk to your doctor or physical therapist about what exercises fit into your specific treatment plan. With this is mind, the four specific components below are important to an effective arthritis exercise program: Range of motion Moving joints through their full available range of movement is important. This frequently increases function and decreases joint stiffness and pain. For this reason, aim to complete these exercises daily. Examples include bending, straightening, and rotating specific joints, or static and dynamic stretching. Strengthening These exercises target muscles supporting and protecting our joints and bones. Strengthening is also necessary for weight control, so two-to-three sessions per week are recommended. In order to allow your body to adapt, begin with light resistance and start slow. Strength exercises include weightlifting and using resistance bands. Low-impact aerobic exercise Aerobic exercise is certainly necessary for overall well-being, weight management and heart health. Aim for two-to-three sessions a week. Low-impact exercises include walking, swimming, cycling, elliptical machine exercises and water aerobics. Balance Good balance is also vital for an effective arthritis program. On the positive side, solid balance prevents falls by increasing your ability to stay upright whether you are moving or sitting still. Likewise, it improves your confidence with walking and daily activities. In order to keep excellent balance, incorporate daily balance exercises. Examples of balance exercises include the use of an exercise ball, Tai Chi and exercises such as standing on one foot. Start Slow, Finish Strong As you begin your exercise program, remember to listen to your body. Start slowly – it can take several weeks for your body to adjust to exercise. Consult your doctor, or physical therapist, if you experience increasing pain or swelling which doesn’t go away with rest. Above all, incorporate fun and motivating activities so you’ll stick to them long term and improve your results. Renown Physical Therapy & Rehab 775-982-5001 Through outpatient physical, occupational and speech therapy, Renown Physical Therapy & Rehab gives you hands-on, individualized treatment in convenient Reno/Sparks locations. We have the latest, most advanced physical therapy and rehab equipment, specialty services and treatments. Renown Physical Therapy & Rehab is now open on Robb Drive in addition to three additional locations in Reno and Sparks. Call 775-982-5001 or visit us online.
-
What is Disordered Drinking?
An alcohol problem can affect anyone at any age. Many factors, including job stress, genetics or depression, may contribute to the start of disordered drinking. Drinking alcohol exists on a continuum. For example, if someone feels down in the dumps for some time, it doesn’t mean they are clinically depressed. So if someone goes through a period with above-normal alcohol consumption, it doesn’t necessarily mean they abuse alcohol. Although “alcoholic” and “alcoholism” are common, they are not clinical descriptions. Alcohol use disorder is the preferred term. Symptoms are often mild but can be the start of a more significant problem. According to the National Institutes of Health (NIH), over 16 million adults live with alcohol use disorder. Symptoms of Alcohol Use Disorder Do you recognize any of the following symptoms in yourself or someone you know? Drinking more or longer than intended Trying to cut down or stop drinking but not able to Having to drink more than you once did to get the same feeling Being annoyed when family members discuss your drinking Regretting your behavior while you were drinking
-
Clubfoot An Unexpected Story of Expert Baby Care
A clubfoot is where the foot is turned in on itself and points toward the ground. A clubfoot diagnosis during pregnancy is surprising and challenging during any circumstance. And in the case of parents anticipating surgery during a pandemic, options can be scarce. These parents took a deep breath, and with the help of Michael J. Elliott, MD, pediatric surgeon with Renown Children’s Hospital, their baby is on the road to recovery.
Read More About Clubfoot An Unexpected Story of Expert Baby Care
-
How Philanthropy Helps Address Gaps in Care
In Nevada, we are so fortunate to have a number of not-for-profits and philanthropists who are supporting our mission at Renown Health; we couldn’t do it without them. In the world of healthcare, we are doing well in driving community benefit programming through operations. However, the things our communities need investments in are so much broader than we might be able to afford on our own. That is why it is essential for us to be supported by the people who are so in love with this community and want to assure we get the kinds of services and care for those who can’t afford it or add new services that are contemporary and leading edge that have not been offered here before. Establishing Behavioral Health & Addiction Institute We are so excited to receive a very generous donation from Chuck and Stacie Mathewson for the Stacie Mathewson Behavioral Health & Addiction Institute. This institute is so sorely needed in northern Nevada. Renown Health has a very important role in being able to bring attention to this important problem of mental health and addiction challenges in northern Nevada. Keeping Pediatric Care Close to Home One of the most important areas where philanthropy comes in handy for us at Renown Health is by assuring that we have the foundational programs that we would not be able to afford with operations alone. For example, the William N. Pennington Foundation’s generous gift has allowed us to create 15 pediatric specialty areas here in northern Nevada so children who have an illness or injury no longer need to leave town. The William N. Pennington Foundation supported Renown Children’s Hospital in a way that we never would have been able to support on our own. We are eternally grateful, and their gift — that 100,000 children are assured access to contemporary health and healthcare services — is beyond comprehension.
-
What Is the Role of a Child Life Specialist?
What is the role of the child life specialist? Here are common questions and answers about how these special individuals give both parents and kids peace of mind. Let’s face it: A hospital can be an intimidating place for just about anyone. But add in being a small human with very little worldly experience — aka a child — and it’s easy to imagine how overwhelming a hospital visit can be. Enter the role of the child life specialist. Liz Winkler, a child life specialist with Renown Children’s Hospital, explains how a Renown program puts young patients and their families at ease. What does a child life specialist do? Child life specialists help young patients develop ways to cope with the anxiety, fear and separation that often accompany the hospital experience. They give special consideration to each child’s family, culture and stage of development. As professionals trained to work with children in medical settings, specialists hold a bachelor’s or master’s degree in the areas of child life, child development and special education or recreational therapy. Our child life specialists are also professionally certified and affiliated with the national Child Life Council. Child life specialists also offer tours of Renown Children’s Hospital for families whose children are scheduled to have surgery. Child life supports children and families by: Helping children cope with anxiety, fear, separation and adjustment Making doctors, needles and tests a little less scary Providing art, music and pet therapy Organizing activities Addressing your concerns Telling you what to expect Creating a therapeutic and medical plan Offering a hand to hold What else is available at the Children’s Hospital that helps ease some of the stress of a hospital visit? Whether it’s seeing a pediatrician, getting a sports physical or looking for advice, our care is centered on supporting and nurturing patients and families at our many locations. We have kid-friendly environments to help ease some of the stress of a hospital visit. These include colorful exam rooms, kid-friendly waiting and common areas, and medical equipment designed especially for children. Our children’s ER is open 24 hours a day, seven days a week. So parents and caregivers have access to emergency care tailored to little ones — anytime, day or night. We have several pediatric specialists on the Renown team in areas including diabetes, emergency medicine, neurology, pulmonology, blood diseases and cancer. How can parents start to ease their children’s mind when they know a hospital visit is in the future? As with many things in life, good preparation can help kids feel less anxious about the experience and even get through recovery faster. It’s important to provide information at your child’s level of understanding, while correcting any misunderstandings, and helping to eliminate fears and feelings of guilt. If you’re anxious and nervous, your child may reflect these feelings and behaviors. So make sure you educate yourself, feel comfortable with the process, and get your questions answered.
Read More About What Is the Role of a Child Life Specialist?
-
Bone Fractures in Children Honest Expert Advice
Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis, answers some common questions about bone fractures. Is there a difference between broken bones and fractures? No, these are two different names for the same injury. Of course the common term is a broken bone. Using either name will describe your concerns. Medical personnel typically describe a broken bone as a fracture to a specific bone. For example, a broken wrist is also a fractured distal radius. To clarify, this describes the injured bone and the precise location. How do I know if my child has broken their bone? Many times children will fall and complain of their arm or leg hurting. In most cases the pain goes away and the child will return to their activities. When there is a deformity to the limb (curve in arm) and the child is complaining of pain, it is probably a fracture. If the arm or leg looks straight, look to see if there is any swelling or bruising. Both are signs of a possible fracture. Finally, if the limb looks normal but the child continues to complain, gently push on the bone. Likewise if it causes the same pain, then they likely have a fracture and should have an x-ray. My child fractured their growth plate, what does this mean? Growth comes from this area of the bone. In detail, these are located all over the body but typically at the end of the bones. With this in mind, fractures to these areas can result in the bone growing abnormally. Because of potential shortening of the arm or leg, or bones growing crooked, it is important to follow fractures closely (up to 1-2 years or longer). It is better to identify a problem early. Small problems can be treated with small surgeries. What if the bones of the x-ray do not line up? Because children are growing, unlike adults, their bones will remodel and straighten with growth. The amount of remodeling occurring depends on a child’s age, the bone fractured and the location. In many cases an angled bone will grow straight over the course of a year. For this reason, someone with experience in caring for children needs to follow bone growth. How long does it take fractures to heal? Factors deciding when a cast can come off include: Child’s age. Bone fractured. Fracture location. Young children heal faster than teens, teens heal faster than young adults, who heal faster than older adults. In young children most fractures heal in 4-6 weeks. However, teens generally take 6 weeks to heal, and adults can take much longer. Although your child is out of their cast, it may not be healed completely to return to all activities. Placing a splint is during this time is common. This typically gives them added protection for several weeks after their cast is removed - in case they forget their limitations. What if my child is still limping? Whether a child is in a walking or non-weight bearing cast, removing it often leaves them stiff and sore. Therefore many children will walk as though they still have a cast in place. In most cases this resolves in about three weeks. Regardless, if your child is still limping or walking abnormally after three weeks, contact the treating doctor. They may benefit from physical therapy or a repeat evaluation. (This article was original published in the July 2019 issue of South Reno Kids & Sports.)
Read More About Bone Fractures in Children Honest Expert Advice
-
Reno Pediatric Scoliosis Expert Gives New Hope to Young Girl
For Michael J. Elliott, MD, a pediatric orthopedic surgeon specializing in scoliosis, it’s just another day helping patients. But to local five-year-old Makenna Christensen, her substantial spine correction is life-changing. Though her journey to body confidence was months in the making, her smiles are a reminder that a thorough, thoughtful treatment plan can yield amazing results. A Surprising Start Words don’t adequately describe the feelings you have when you unexpectedly learn your child has a birth defect. For Nicole and Nick Christensen it was a shocking surprise. During Nicole’s sonogram appointment something unusual was seen. After an amniocentesis, their baby girl was diagnosed with Noonan syndrome, which can affect a child’s height and bones. To prepare, the couple read all they could on the subject. Fortunately their daughter Makenna, was born full term and healthy. Shortly after birth, Makenna had some feeding issues and returned to the hospital. Although they resolved and she had no major complications, both parents felt unsure about their newborn’s future. With the help of Nevada Early Intervention Services , Makenna’s development was monitored until she was three years old. “Her posture has been an issue her whole life,” says Nicole. Nick also noticed when Makenna started walking her range of motion was poor. It was especially noticeable when she got dressed and raised her arms to put on clothing. Nicole observed Makenna was falling a lot in preschool. She asked Makenna’s pediatrician about physical therapy to support her coordination and muscle tone. Although physical therapy was helping Makenna, her therapist suggested Nicole seek the opinion of Dr. Michael Elliott, a pediatric specialist in orthopedics at Renown Children’s Hospital. Scoliosis Casting - A Successful Treatment Approach Dr. Elliott diagnosed Makenna with scoliosis, an abnormal curvature of the spine. While this condition is most common during a teenage growth spurt, it can also happen in early childhood. Affecting about four million people in the United States, it is estimated 20 percent of all spinal deformities in the U.S. are people living with scoliosis. Makenna’s spinal curve was significant – over 30 degrees. Through years of experience Dr. Elliott opted to put Makenna in a spinal cast, instead of multiple surgeries. “My approach is to postpone surgery as long as possible - it is tough for the patient and families,” he says. “Often excellent results can be achieved through non-invasive treatments such as, casting and bracing.” Nicole appreciated Dr. Elliott’s reassurance through the treatment plan. “It was obvious through the X-rays that there was a significant issue,” she shares. “He guided us through the timing and process and how correcting it sooner would help keep her future growth on track.” For seven months Makenna wore a cast that looked like a tank top, bracing her spine while allowing movement. Now she wears a hard plastic brace, specially fitted to her body. “Kids tolerate casting well,” explains Dr. Elliott. “It is a 45-minute procedure. The patient sleeps while their spine is put into traction as the cast dries.” She will continue to wear larger braces as she grows, eventually only wearing them at night. A Straight Path into the Future Dr. Elliott admits, “Not every cast is a cure. Two thirds of a child’s spinal growth happens by the age of five. Getting past the five-year mark means fewer surgeries. It’s wonderful to see Makenna’s body image improved.” Nicole agrees, “The way Makenna holds herself is completely different. She’s more confident on her feet and more balanced.” She can now play with her sister Aria, 4, and brother Lexi, 8 months, without the fear of falling. Nick is in awe of the improvements she has made, “Seeing her thrive more has been wonderful.” The Christensen’s are hopeful about the future. “Makenna is doing really good. She’s wearing her hard brace full time and her growth is consistent,” expresses Nicole. “She’s even starting swim lessons this week.” With mask wearing at every doctor visit during the COVID-19 pandemic, Makenna and Dr. Elliott look forward to seeing each other’s smiles in the future. Makenna’s story highlights the over 18 different specialty options for children locally at Renown Children’s Hospital.
Read More About Reno Pediatric Scoliosis Expert Gives New Hope to Young Girl
-
Healthy Aging 5 Tips to Improve Happiness and Quality of Life
There are a few simple ways to encourage healthy aging that can translate to an improved quality of life. Here are some expert tips. What does healthy aging mean to you? If you’re like most people, you’re looking forward to removing the negative from your life — negative energy, thoughts, people and activities that don’t contribute to your best life. And while that’s a noble goal, too often we forget about ways to strengthen the positive parts of our lives. Expert Herbert “Buddy” Coard III, Ed.D, psychologist with Renown Behavioral Health, provides us with five positive behaviors to focus on to improve happiness and life satisfaction. Healthy Aging in 5 Easy Steps: 1. Connect – Make connections with friends, family, colleagues and neighbors. When you build strong connections, they can help enrich your life with new experiences and opportunities. Besides, having a support system to call upon when you need a favor is valuable as you age. 2. Be Active – Make time to get moving and work those muscles. Being active can include walking, practicing yoga, playing a game of pickleball or dancing. Exercise makes you feel good and keeps you health. Pick a physical activity that you enjoy, and don’t make excuses. Not only will being active help you build stronger muscles, it also helps you build strong connections with others. If you need a workout buddy, Meetup is a great resource to find like-minded people that share common exercise goals. 3. Take Notice – Be mindful and become more curious. Like a child, see the wonder and beauty of the world. Notice the things around you — the weather, the landscape, the mood and feelings of the people around you. By taking notice, it’s easier to learn to appreciate the things that matter. 4. Keep Learning – We never stop learning. Keep trying something new — a new course you’ve always wanted to try or a more challenging task someone has solicited for your help. Challenges keep us on our toes and increase our confidence and excitement in our day. OLLI (Osher Lifelong Learning Institute at the University of Nevada, Reno), brings diverse educational and social opportunities to active older adult learners (50+). EPIC (Educational Programs Inspiring the Community), offers a divers curriculum ranging from art classes to Accelerated training certificate courses. 5. Give – Be generous with your time, your knowledge and your talents by giving to friends, family and even strangers. Some easy ways to give is to show thankfulness, smile at people and volunteer. Sharing of yourself to a wider audience gives you a greater reward than just doing things for yourself. Nevada Volunteers Volunteer at Renown Health Practice these five tips to improve happiness and quality of life at any age.
Read More About Healthy Aging 5 Tips to Improve Happiness and Quality of Life
-
How to Spot Depression in Men
Has a male in your life been affected by depression? It could be your father, husband, or son. Or maybe your brother, a friend – or even, your co-worker. They all have one thing in common, they’re men and they may not always be able recognize when they need help. Here’s how you can support the men in your life by understanding their unique signs of depression. Dr. Coard, Ed.D., Psychologist with Renown Behavioral Health, weighs in on the topic of depression and the warning signs. More than 6 million men are diagnosed with depression each year, and surprisingly, depression in men can differ from women. The signs of depression are not easily recognized and it’s common for men to be in denial about what they’re going through. They can demonstrate anger and aggression instead of sadness – making it difficult for loved ones, or even their providers, to recognize. Behavioral Signs of Depression in Men High levels of the hormone cortisol are released during stressful situations affecting the neurotransmitter, serotonin (a feel good hormone), contributing to depression. You can identify depression or suicidal tendencies by paying close attention to the following behavioral changes: Anger, irritability, or aggression Avoiding family or social situations Losing interest in family responsibilities, passions and hobbies Lack of sex drive Becoming controlling/abusive in relationships Risk-taking behavior such as; unsafe sex, overspending or gambling Not being able to concentrate or remember details Excessive drinking or drug use Having frequent thoughts about death Talking about suicide Attempting suicide Factors That Lead to Depression in Men Life Events Work stress or long-term unemployment can be huge contributing factors relating to depression. This type of life event can be overwhelming, making it impossible for a man to cope. Changes in Relationships The loss of a relationship can be a significant contributing factor to the emergence of depressive symptoms and past experienced physical, sexual, or emotionally abusive relationships. With this in mind, counseling can often help individual to overcome this type of trauma. Grief and Loss Overwhelming sadness due to the loss of a loved one can trigger depression. Although normal, each person goes through their own grieving period. For example, normal responses to death are insomnia, poor appetite and loss of interest in activities. Pay attention if grief seems prolonged or out of the ordinary. Health Problems In particular, depression coexists with medical conditions. As men age, this can be passed off as normal aging, but it could be more serious. In addition, illnesses such as thyroid disorders, Addison’s disease and liver disease can cause depressive symptoms. Diabetes, cancer, heart disease, or Parkinson’s disease can affect any age, thus triggering or worsening depression. Some older men also feel like they may be suffering from dementia because of difficulties with memory this may be a symptom of depression. A trip to the doctor may be in order to help alleviate concern and worry. Depression in Men and Suicide Frequently the emotional pain occurring with depression can distort a man’s ability to see a solution beyond suicide. Individuals with depression become very rigid and constricted in the way they solve problems. The statistics below speak for themselves, helping us understand the need to reach out to those who need our support. Male suicide rates are on rising – men die by suicide 3.53 times more often than women, accounting for 70% of all suicides. Sadly, every day 129 men commit suicide. White males accounted for 69.67% of suicide deaths in 2017. In 2017, firearms accounted for 50.57% of all suicide deaths. Middle aged Men who are middle aged have the highest suicide rates. 40% of those identifying as transgender have attempted suicide in their lifetime. Males who are guy or transgendered are at an increased risk for suicide attempts, especially before age 25. Veterans often suffer from post-traumatic stress disorder (PTSD) and depression, and are more likely to act on a suicide plan. How You Can Help Now that you can identify some of the warning signs of depression, here’s how you can help: Talk about your concern and communicate that you’re there to help him. Let him know depression is a medical condition and will usually get better with treatment. Suggest professional help from a Primary Care Provider, Psychologist or Therapist. Help set up appointments and offer to accompany him – let him make the decision, but make it clear you’re there for him, no matter what he decides. If you feel he is in a dire or life-threatening situation, contact 911. Call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to talk to a trained counselor. Call the Veteran’s Crisis Line at 1-800-273-TALK (1-800-273-8255) and press “1”
-
Fighting Depression with rTMS Therapy
If you ask most people who suffer from depression what it's like, it can be difficult to fathom. We spoke with the courageous and fearless Kathryn, who has endured major depressive disorder (MDD) most of her life. She recollects what it was like, and how grateful she is for a new rTMS therapy treatment she recently completed. Kathryn is a local resident who shares her story to provide hope and support to others surviving depression. From her accounts of the grueling years she faced this disorder to how hard she fought to find treatment, Kathryn is a true hero. According to the National Institute of Mental Health, major depression is one of the most common mental disorders in the U.S. The disease causes people to experience sadness and helplessness, and in some cases, may prevent people from carrying out their daily routines. No two people are affected the same way, meaning there's no "one-size-fits-all" for treatment. Finding help is typically a long and exhaustive journey for most surviving depression. The Long and Confusing Road to Finding Help Kathryn is no different from most major depressive disorder (MDD) survivors, fighting for a better future. Her mental health treatment journey started as early as 12 years old; however, she wasn't diagnosed with depression until much later in life. In her late 20s, a friend told Kathryn she was depressed, but like so many individuals battling the illness, Kathryn didn't know what depression was. The waiting lists to get into mental health treatment was devastating. She found mental health resources scarce, an issue far too familiar throughout the U.S. After being prescribed more than twenty different depression disorder medications, she wasn't sure who she was or if she'd survive. Determination to Fight Kathryn's darkest moments lead to experiences that are unspeakable to relive. But in her persistence to not give up, she began researching a more promising treatment. “I was looking for an evidence-based therapy,” says Kathryn. “In my research, I found Transcranial Magnetic Stimulation Therapy to be most promising.” After a yearlong waiting list for repetitive transcranial magnetic stimulation (rTMS) therapy in another state, Kathryn moved to Reno, Nevada, still searching for a location that offered this therapy. Thankfully, Kathryn's arduous journey led her to the Stacie Mathewson Behavioral Health & Addiction Institute at Renown. That is where she received news from her doctor, Gunjan Lehil, MD, that rTMS is offered for people looking for a new way to fight depression. How rTMS Therapy Works rTMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression – typically used when other depression treatments haven't been effective. This treatment involves delivering repetitive magnetic pulses, referred to as repetitive TMS or rTMS. During an rTMS session, an electromagnetic coil is placed against the person's scalp near their forehead. The electromagnet painlessly delivers a magnetic pulse that stimulates nerve cells in the region of the person's brain involved in mood control and depression. It's thought to activate areas of the brain that have decreased activity in depression. Though the biology of why rTMS works isn't completely understood, the stimulation appears to impact how the brain works, which seems to ease depression symptoms and improve mood. On average, patients undergo rTMS treatments for four to six weeks, five days a week for about 40 minutes a day. A patient's doctor will determine a treatment plan that's best for the patient in all cases. Life After rTMS Therapy After completing six weeks of rTMS therapy, Kathryn feels as though she is coming back to life. She has noticed her posture is different, and she is more animated. She is also more interactive at work, and her coworkers are more perceptive and positive towards her. Life at home is also improving, as Kathryn's family is noticing a difference. She notes that while she still faces feeling depressed, it's so much different from it used to be. The difference is, she can better decipher a bad day and work through the challenging moments. She has hope - which she never felt before. rTMS Therapy has given Kathryn a chance at life, and she's excited to start living! The Future is Fearless Kathryn says the way to success is never to give up and to keep pushing herself forward every day. Currently a veterinarian technician in training, Kathryn is working on getting her license. She loves working with all animals, but her true passion is falconry and helping injured birds of prey. She loves falcons because they are utterly fearless, just like her. "It's time for me to be brave and show up. I couldn't do that before," says Kathryn. "I'm grateful to have rTMS treatment, and I share my story in hopes of helping others."