Search
-
Prevent Osteoporosis: Take Control of Your Bone Health Today
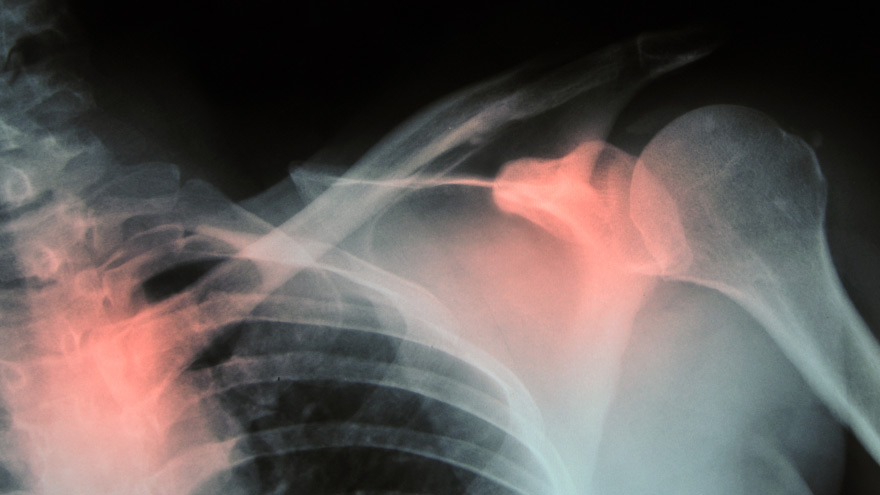
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
Baby's Ears and Altitude Changes
One of the best things about living in the Reno area is the beautiful mountain range that surrounds our city. Many families take advantage of the activities the mountains have to offer or travel over them to visit friends and family in neighboring areas. However, for parents of infants there is often angst over your baby’s ears and altitude changes and the associated potential for ear pain and/or “popping.” Fortunately, there are things you can do to protect your infant’s ears the next time you drive over the mountain or hop on a plane with your little one. Baby’s Ears and Altitude Changes: What Causes Them to “Pop” The simple answer is pressure. The problem originates in the middle ear where there is an air pocket that is vulnerable to changes in pressure. The Eustachian tube, which runs behind the nose to the middle ear, is constantly absorbing and resupplying air to this pocket to keep it balanced. When the pressure is not balanced, your ears feel “clogged” or like they need to “pop.” In some cases this sensation can cause significant ear pain and even temporary hearing loss. Rapid changes in elevation or altitude, like driving over a mountain, or ascending or descending on an airplane, can cause rapid changes in pressure. In order to avoid problems, the Eustachian tube needs to open widely and frequently to equalize those pressure changes. The problem often intensifies during descents as you go from an area of lower atmospheric pressure to an area of higher atmospheric pressure. This is why you hear babies screaming on planes during descent or why your infant is wailing in the car seat as you head down the mountain. What can you do to make it a more comfortable trip for your child? First, be prepared. Babies cannot intentionally “pop” their ears like adults can, but we can help them by encouraging them to swallow. Offer your baby a pacifier or bottle while making ascents and descents. If possible, it may be helpful to have an adult ride in the back seat with baby if you’re in the car to ensure this can happen. Don’t let your baby sleep during descent on a plane. Help your little traveler out by offering him or her a pacifier during this process, as descent is the most likely time for pain associated with altitude changes. If your baby is congested prior to travel involving altitude changes, seek the advice of your pediatrician since they may have other solutions, including medications such as decongestants. If you return from a trip and notice your infant is still fussy and uncomfortable, contact your child’s doctor for a thorough ear evaluation. Safe travels!
-
Think Outside the Box: Healthy, Creative School Lunch Hacks
Gone are the days of soggy PB&Js on white bread: Today’s school lunch is your chance to create a healthy, colorful midday meal! Here are a few simple tips, a week of lunch ideas and a shopping list to help you pack a lunch that won’t be offered up for trade during tomorrow’s lunch hour. While school lunches are getting healthier, packing and taking a lunch to school will ensure that your child is getting a healthy, well-balanced meal. Making lunches should be a team effort. Your kids can help pack their lunches by spreading on condiments or putting food in containers. To save time in the morning, pack lunches the night before. The following are a few suggested items you can use to ensure your child is eating a tasty but nutritious lunch: Main dishes Lunch meat and lowfat cheese roll ups English muffin pizzas Sandwich wraps – meat, cheese and veggies in a whole grain tortilla Pita pockets stuffed with grilled chicken and vegetables Soup Chef salad with spinach, veggies, cheese, lunch meat and dressing Tuna or chicken salad on a mini bagel Snacks and sides Fresh or dried fruit Natural apple sauce Baked tortilla chips and salsa Veggie sticks and hummus Cheese slices or string cheese with whole grain crackers Homemade trail mix with nuts, seeds and raisins Pudding Homemade fruit roll ups Popcorn (add different toppings such as salt, garlic, cinnamon, sugar or cayenne pepper) Drinks Water If you child doesn’t like plain water, try adding a few slices of fresh fruit (strawberries, lime, lemon) for more flavor. School Lunch Menu: Day-By-Day We’ve put together a week’s worth of colorful, fun and healthy school lunch ideas your kids will love. And we’ve also created a shopping list to help you easily locate all the ingredients on your weekend shopping trip. Monday: Turkey BLTA Roll-ups Roll-up Ingredients Turkey, cold cuts Bacon Avocado Tomatoes Side Dish Choices Blueberries Cucumbers Carrot sticks Tuesday: Bacon & Cucumber Sandwich Sandwich Ingredients Whole wheat English muffin Cucumber Bacon Side Dish Choices Apples slices Strawberries Vanilla yogurt mixed with sprinkled cinnamon Wednesday: DIY Lunchables Lunchables Ingredients Crackers Turkey, cold cuts Cheese Side Dish Choices Blueberries Carrots Cucumber Thursday: Veggie Grilled Cheese Veggie Grilled Cheese Ingredients English muffin Cheese Tomato Spinach leaves Avocado Side Dish Choices Apples slices Strawberries Vanilla yogurt mixed with sprinkled cinnamon Tomatoes Friday: DIY Pizzas DIY Pizza Ingredients 2 toasted English muffins Pizza sauce Cheese Turkey pepperoni Side Dish Choices Celery Black olives Shopping List (under 20 items) Cold section: Dairy 1 large container of vanilla yogurt 1 package of your favorite cheese Cold section: Deli meats 1 package of turkey pepperoni 1 package bacon 1 package turkey cold cuts Inside aisles Whole wheat English muffins 1 can of whole black olives 1 jar of pizza sauce 1 box of whole wheat or multigrain crackers Produce department 1 cucumber 1 stalk of celery 2 apples 1 container of strawberries 1 avocado 2 tomatoes 1 bunch of spinach leaves 1 container of blueberries 2 carrots For more healthy school lunch box options, visit our Kids Health & Nutrition board on Pinterest.
Read More About Think Outside the Box: Healthy, Creative School Lunch Hacks
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
Early Onset of Puberty in Girls on the Rise
Many factors are contributing to the rise of early onset puberty in girls. Learn what they are below and how you can support your daughter. The number of girls experiencing early puberty has increased dramatically over the last few years and continues to grow. More and more girls in the U.S. are starting to show signs of development before the age of 8. Recent studies show that up to 10 percent of Caucasian girls and 23 percent of African American girls are showing signs of puberty by age 7. What’s Contributing to Early Puberty in Girls? Determining the exact cause is difficult. But experts agree that several factors may be contributing to these growing numbers. Increasing rates of childhood overweight and obesity. Excess body fat alters the levels of hormones responsible for the acceleration of pubertal timing. Physical inactivity may decrease melatonin levels, which can also trigger pubertal development. Increased animal protein intake. Higher total protein, animal protein and meat intake in children ages 3 to 7 have been associated with earlier onset of menstruation. High protein intake elevates IGF-1 levels and promotes growth, which could accelerate the onset of puberty. Poor diet. Children with lower-nutrient diets tend to enter puberty earlier. A diet rich in processed foods and meats, dairy, and fast food is disruptive to normal physical development. Exposure to EDCs (endocrine-disrupting chemicals). EDCs are synthetic chemicals found in plastics, pesticides, fuels and other industrial chemicals that inhibit or alter the action of natural hormones. Because EDCs accumulate in the fatty tissues of animals, animal foods contain higher levels of these chemicals than plant foods. Exposure to BPA (bisphenol A). BPA is an industrial petrochemical found in a variety of products including plastics, tin-can linings and even cash register receipts. Because it acts as a synthetic estrogen it may speed up pubertal development. Soy products. Soy contain isoflavones which are converted to phytoestregens in the body, and are similar to the hormone estrogen, Dr. Chelsea Wicks says. “Soy consumed from natural food sources is likely safe and will not cause abnormal hormones levels. However, when consumed in large amounts, such as with soy supplements or in more processed foods, there have been links to chronic medical problems due to elevated estrogen levels. I feel a good answer to this is to continue working on eating fresh foods and trying to avoid the processed, packaged foods as this will be best for overall general nutrition as well,” she adds. What You Can Do While some genetic factors play a role in the early onset of puberty, parents can help lessen environmental causes of the condition. Encourage and help your child to maintain a healthy weight with proper nutrition and exercise. Avoid exposure to hormones such as estrogen and testosterone that may be found in hair products, medications and nutritional supplements. Avoid exposure to EDCs and BPA. Offer your child a diet centered around whole plant foods rather than animal foods, which will help keep protein intake within a safe range and reduce consumption of EDCs. Create a supportive environment for your daughter. Avoid commenting on her appearance and instead focus on her achievements, academic successes or artistic talents. Speak to her openly and honestly about the physical changes she’s experiencing — that although these changes are normal, she’s simply developing early — and that ultimately her peers will undergo the same changes. Encourage your daughter to continue participating in social activities and pursuing her interests, and reassure her you are always open to discuss any questions or worries. If you are concerned that your child may be going through these changes before expected, speak with your pediatrician. Sources: Early Puberty: Causes and Consequences When Is Puberty Too Early? Precocious Puberty (Early Puberty) Precocious Puberty
-
Ask the Expert: What is Scoliosis?
Posture is important, but for those children diagnosed with scoliosis (spinal curvature) it can be a difficult issue. The Washoe County School District Student Health Services Department screens 7th grade students for scoliosis as growth spurts often reveal the condition and, if diagnosed early, scoliosis can stop progressing. We asked Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis to answer some frequently asked questions about scoliosis. What is scoliosis? There are many types of scoliosis: early onset (occurs before age 10), congenital scoliosis is when the bones of the spine do not form correctly, neuromuscular scoliosis which is due to children’s neurologic and muscle disease, and the most common is Adolescent Idiopathic Scoliosis. The term “idiopathic “ means the exact cause is unknown, although we do know it runs in families. This type of scoliosis occurs in 2-3 percent of adolescents and is mainly seen during their growth spurt. This is why middle school screenings are recommended. Both genders get scoliosis but girls are 8 times more likely to have their curves progress and become larger. What are the signs that my child may have scoliosis? A few signs for parents to watch for are: One shoulder might be higher than the other. One leg may seem longer. A hip may be higher or look more prominent. The waist may not look the same from side to side (asymmetry). The trunk or rib cage may be more prominent on one side or shifted. When they bend forward they may have a bump on their back. How is scoliosis diagnosed? It can be noticed by a pediatrician at a physical, school screening nurse, PE teacher or parents. Once the curve is suspected the child is usually referred to a pediatric orthopedic surgeon scoliosis expertise. At the initial visit the doctor will perform a thorough physical including a complete neurologic exam to assess the amount of curvature. Once the exam is completed the physician will determine if a spinal x-ray is needed. The curve on the x-ray is measured utilizing the cobb angle (a measurement in degrees) which helps guide the treatment. What are common treatments for scoliosis? The treatment depends on the size of the spinal curve and the amount of growth the child has remaining. An x-ray of the child’s hand is used to determine the amount of growth remaining. This allows the determination of the child’s bone age, and based on the hands growth plates it can determined if the child is in their rapid phase of growth. Treatments include: Observation - For curves less than 20-25 degrees. This entails visits every 6-9 months with a repeat scoliosis x-ray. Since scoliosis curves increase only 1-2 degrees per month, and variations in measurements can be 3-5 degrees, an x-ray is not recommended before 6 months. If the curve remains less than 25 degrees the child is followed until their growth is completed (usually age 16-18). Progressing Curve - If growth is finished and the curve is less than 40 degrees, the risk of more curvature into adulthood is small. If growth is completed and the curve is over 45 degrees, the child is followed for several years as these curves can progress into adulthood. If the patient is still growing and the curve has progressed greater than 25 degrees but still in the non-operative range (less than 45-50 degrees) bracing is used to stop the progression of the curve. Bracing - Indicated for curves over 25 degrees but less than 45 degrees. If a brace is required you will be referred to an orthotist (bracing specialist). The orthotist assesses your child, reviews the x-ray and then fits the brace. (Having a brace made usually takes 2-3 weeks.) Once the brace is fit, your child will visit the scoliosis specialist for an x-ray in the brace to ensure it fits correctly. The primary goal of bracing is to halt progression of the curve and prevent the need for surgery. The brace must be worn for about 16 hours per day to be effective. In a recent bracing study 72% of the patients who wore their braces as prescribed prevented the need for surgery compared to the group who did not wear their brace. Surgery: When a curve reaches 45-50 degrees, and a child is still growing, surgery is usually recommended because the curve is likely to continue progress. If a curve is over 50 degrees and the child is done growing surgery also may be recommended. This is because when curves are over 50 degrees they tend to increase 1-2 degrees per year for the rest of your life. As curves get larger the amount of lung function tends to decrease which could cause breathing problems later in life. The goals of surgery are to stop the progression of the curve and safely correct any misalignment. This is accomplished by attaching implants (rods, screws, hooks and bands) to the spine. Bone graft is then placed around the implants to encourage the spine to fuse (grow together). This then forms a solid column of bone with metal rods in place, preventing the curve from changing. Most patients are back to their regular sports and activities six months post surgery.
-
Children's ER, Urgent Care or Wait it Out? Here's Your Guide
We’ve all been there: Your child gets sick right after urgent care closes — or worse, in the middle of the night. So do you wait it out, or do you load up and head to the Children’s ER? Pediatric Emergency Physician Joey Gassen, MD, with Northern Nevada Emergency Physicians, has insight. As parents, we often wish we had all the answers. And while a short-and-sweet comprehensive parenting guide is elusive, we can help if your questions involve whether to go to the children’s ER or wait it out. Here, a pediatric emergency physician explains when you should take your child to the Children’s ER at Renown Children’s Hospital, and what makes a children’s ER different. How do you know when it’s time to take your child to the ER? Having a sick or injured child is stressful. If you have a true emergency, you should go straight to the ER or call 911. When to go to the ER: Allergic reactions Asthma or severe shortness of breath Fever (infants less than two months old) Choking or poisoning Coughing up or vomiting blood Fainting, confusion or seizures Fractures or broken bones Head injuries Severe bleeding If you determine your child’s condition isn’t life-threatening but needs to be taken care of right away, urgent care is the best choice. Those conditions include: Cold and flu Coughs and sore throat Fevers Vomiting, diarrhea, stomach pain Cuts and severe scrapes Minor injuries and burns What is different about Renown Children’s ER compared to the adult ER? The difference starts when you first bring your child in. We have a lobby dedicated to our community’s smallest patients. The 24/7 lobby incorporates a child-friendly atmosphere with vibrant colors to help decrease anxiety that can accompany emergency situations. Our children’s ER also has equipment sized just for kids of any age. We offer a distraction machine, as well as games and movies, to help children cope with what can be a traumatic experience, like getting an IV. In addition, we have Child Life Specialists available to provide the emotional support to both children and their families. Why is it important to have an emergency room and lobby open 24/7 dedicated to children? Children aren’t just little people. They have special needs that require specialized care. Our children’s ER is staffed with skilled physicians and pediatric nurses certified in advanced pediatric emergency care to give your child the highest level of support. Renown Children’s Hospital From newborns to teens, Renown Children’s Hospital offers many different services and treatments designed specifically to take care of our community’s children. We provide a range of specialized services — from a dedicated Children’s ER and Pediatric ICU to a children’s imaging center and child’s asthma program. Explore Children’s Services
Read More About Children's ER, Urgent Care or Wait it Out? Here's Your Guide
-
A Day in the Life of a Child Life Specialist
March is Child Life Month, meaning this is the perfect time to ask: What exactly does a Child Life Specialist do? To find out, we “virtually” tagged along with one for a day. This is what a typical day looks like in this important role. For Child Life Specialist Brittany Best, play is a natural part of her work day. She approaches her role with a keen understanding of how the seemingly small tasks she performs every day — comforting children prior to a procedure, writing thank-you notes to donors, training interns — positively impact the lives of the children she serves and their families. So what does it take to work in Renown’s Child Life Program? Best shares some of the highlights from a “typical” shift. A Child Life Specialist’s Day 7:30 a.m. Clock in, put my belongings in my office, and print the patient census information. This helps me to get a sense of the day ahead, as I’m covering three areas today. 8-9 a.m. I look over the census sheets for all three areas and check in with the nurses in each area and then try to prioritize my day. 9:00 a.m. I attend Interdisciplinary Rounds for the Pediatric Intensive Care Unit, where the most critically ill or injured children are treated. Additionally, Interdisciplinary Rounds enable several key members of a patient’s care team to come together and offer expertise in patient care. 10:00 a.m. I come up to the specialty clinic/infusion center to check on the patients that have arrived already and see how things have been going since I had last seen them. We see patients frequently up here, as they are receiving treatment for cancer or other disease processes. 10:55 a.m. I’m notified by an RN that a patient needs an IV started, so I go meet with the patient and their family. I meet with a 6-year-old and mother to explain what an IV is and why it is needed. We go through an IV prep kit, looking at all the different items the nurse will use including cold stinky soap, a tight rubber band and also a flexible straw. I also teach this patient a breathing exercise to help them relax during the procedure with a simple exercise known as “smell flowers, blow out candles.” I demonstrate how to take a deep breath in through the nose — like smelling flowers — then how to blow that breath out — like blowing out birthday candles. 11:10 a.m. I walk with the patient and mom to the procedure room on the Children’s Patient Floor for an IV procedure. The Vecta distraction station is set up and running with its bright lights and water tube that bubbles with plastic fish swimming. The parent holds the patient in their lap, and with the distraction and medical preparation, we are successful! I give the patient a toy and provide emotional support to both the young patient and his mom. It’s easy to forget that these procedures can be stressful for the parents as well. 11:30 a.m. I finish rounding with staff to catch up on patients. In addition, I introduce myself to patients and put my contact number on the board in each room so the families know how to get a hold of me should they need anything. With support from volunteers, we distribute movies, games, and “All About Me” forms to patients and their families. These forms help us get to know our patients with things like their favorite foods and televisions shows. 12:45 p.m. I help with a lab draw in Children’s Specialty Care. A 3-year-old patient is very anxious about the “shot,” so I meet with the patient and parents to discuss coping techniques. The patient holds the Buzzy Bee and does well during the lab draw. The mom is relieved, and the patient is excited for a toy. The Buzzy Bee actually helps block the transmission of sharp pain on contact through icy numbing and also tingly vibration. 1 p.m. Joan, an artist with our Healing Arts Program, arrives on the Children’s Patient Floor to perform art therapy with patients. She helps two young patients who are interested in watercolor paintings. 1:15 p.m. Time for lunch and also a trip to Starbucks. 1:45 p.m. I finishing rounding and introducing myself and our services to the patients I have not met yet. 3 p.m. At this time, I meet with the parents of a newly diagnosed diabetic patient who is in intensive care. A new chronic diagnosis is always difficult, so I am there to provide emotional support. It’s instances like this that remind me every day why I love the work I do. 3:30 p.m. I meet with a new volunteer, discuss their role and also give the new volunteer a tour of the units. We are very thankful for all our volunteers on the floor, as their contributions help us provide a variety of basic services to a larger number of children. This also allows the Child Life Specialist to devote time to children who require more intense or specialized service. 4-5 p.m. I finish charting on patients and help two newly admitted families before I start to wrap up for the day. This evening we have a volunteer covering the times during shift change, which is helpful as it makes for a smooth transition for families during the meal time and change of shift. During this time, I write a note for this volunteer indicating the patients I want her to focus on. 5-5:30 p.m. Check in with critical patients and families before leaving for the day. All-in-all, it was a good day.
Read More About A Day in the Life of a Child Life Specialist
-
Get Moving: How to Exercise with Arthritis
An arthritis diagnosis doesn’t mean your exercise routine has to end. In fact, a consistent routine can actually improve mobility. Although stiff and painful joints can make it difficult to keep moving, staying active is essential for easing pain. October 11 is World Arthritis Day, so we asked Michelle Higgins, MPT at Renown Physical Therapy & Rehab some advice about exercising with arthritis. According to the Arthritis Foundation, arthritis affects one in five adults and 300,000 children. As a matter of fact arthritis is the nation’s leading cause of disability. Your joints certainly don’t need to suffer when you exercise. In general exercise is actually necessary for those with arthritis. Not only does it reduce joint pain, but it also increases strength and flexibility. Furthermore those adopting a regular exercise routine also have more energy, deeper sleep and find it easier to maintain a healthy weight. “Exercise is a necessary component to managing your arthritis,” says Higgins. “Consistent participation in an exercise program has been shown to promote long-term pain relief, increased body function and an improved quality of life. Alternatively, a lack of exercise can actually increase joint pain or stiffness and eventually lead to long term disability and suffering.” Exercising With Arthritis Exercise truly is the most effective non-drug arthritis treatment available for reducing pain and improving movement. And it can even include daily activities like gardening, dancing or walking your dog. Of course talk to your doctor or physical therapist about what exercises fit into your specific treatment plan. With this is mind, the four specific components below are important to an effective arthritis exercise program: Range of motion Moving joints through their full available range of movement is important. This frequently increases function and decreases joint stiffness and pain. For this reason, aim to complete these exercises daily. Examples include bending, straightening, and rotating specific joints, or static and dynamic stretching. Strengthening These exercises target muscles supporting and protecting our joints and bones. Strengthening is also necessary for weight control, so two-to-three sessions per week are recommended. In order to allow your body to adapt, begin with light resistance and start slow. Strength exercises include weightlifting and using resistance bands. Low-impact aerobic exercise Aerobic exercise is certainly necessary for overall well-being, weight management and heart health. Aim for two-to-three sessions a week. Low-impact exercises include walking, swimming, cycling, elliptical machine exercises and water aerobics. Balance Good balance is also vital for an effective arthritis program. On the positive side, solid balance prevents falls by increasing your ability to stay upright whether you are moving or sitting still. Likewise, it improves your confidence with walking and daily activities. In order to keep excellent balance, incorporate daily balance exercises. Examples of balance exercises include the use of an exercise ball, Tai Chi and exercises such as standing on one foot. Start Slow, Finish Strong As you begin your exercise program, remember to listen to your body. Start slowly – it can take several weeks for your body to adjust to exercise. Consult your doctor, or physical therapist, if you experience increasing pain or swelling which doesn’t go away with rest. Above all, incorporate fun and motivating activities so you’ll stick to them long term and improve your results. Renown Physical Therapy & Rehab 775-982-5001 Through outpatient physical, occupational and speech therapy, Renown Physical Therapy & Rehab gives you hands-on, individualized treatment in convenient Reno/Sparks locations. We have the latest, most advanced physical therapy and rehab equipment, specialty services and treatments. Renown Physical Therapy & Rehab is now open on Robb Drive in addition to three additional locations in Reno and Sparks. Call 775-982-5001 or visit us online.
-
Not a Fall Sports Fan? Ways to Keep Kids Active
The mornings are crisp and it’s about time to pull out those scarves and boots, so what does that mean? Football, baby! But not all kids are fans of fall sports. Elaina Lantrip, an advanced practitioner with Renown Pediatrics talks about how to keep kids active if they’re not in love with fall sports. Fall in northern Nevada means tailgates, Saturdays at the field, football fun and prep time for basketball season. But oddly enough, we parents aren’t in control of our kids’ likes and dislikes — shocking, we know. This means sometimes kids don’t like the fall sports we enjoy. So how do we keep them active even if they’re not a fan of football, basketball or any sport ending in “-ball”? We asked Elaina Lantrip, APRN for Renown Pediatrics, for some tips. Activities for Kids Who Don’t Like Fall Sports What are some reasons kids may not be interested in sports? Team sports are often the go-to option to get your children more active. But there can be a number of reasons your child may not be interested. First, many fall sports are open to preschoolers, but it’s not until age six or seven that most kids have the attention span, physical skills and can fully grasp the rules. If your child is nervous about their abilities, try practicing at home before quitting the sport. You may find your child becomes more interested as they become more confident in their skills. Other kids may find team sports too competitive and feel too much pressure to play perfectly for their coach and teammates. If possible, evaluate the coach and league before signing up to find out how competitive they are. Doing so ahead of time may help you find the right fit for your little one. What do you suggest to keep kids moving when they don’t like fall sports? Some kids just don’t enjoy sports or would prefer to do something on their own, and that’s fine too. Kids can still get the 60 minutes of exercise they need each day in other ways. Free play such as shooting baskets, riding bikes, playing tag or jumping rope can be good options or they may be interested in individual sports such as swimming, horseback riding, dance lessons, roller skating or skateboarding, hiking, golf, tennis, gymnastics, martial arts, yoga, running or cheerleading. All of these are good options because they keep your child active and moving, but may fit better with what they’re interested in and truly enjoy. How can you work with your child to find which activity is best for them? Finding the right fit can be a challenge. It’s important to be patient as it may take several tries at different sports or activities to find the right activity. Start by explaining to your child they need to take part in some activity. Work with your partner to create a list of options you both agree on and see what interests your child. Once your child makes their pick, make them stick with it through one season or a full set of lessons to ensure they get a complete idea of what’s involved. One game or one lesson isn’t enough to decide it is or isn’t for them. What are some easy ways to be active indoors? Even though staying indoors can be a bit of a bummer, there are plenty of options to help your kids and yourself stay active while enjoying some quality time together. You can plan a scavenger hunt, build a fort, set up hopscotch in the hallway, throw a dance party and make everyone freeze each time the music stops, create an indoor obstacle course, hula hoop or play tag in the living room. As your kids get older, playing video games that require movement and mimic sports or physical competitions are good options. Your kids may even join in on a workout DVD or you can have a friendly contest to see who can do the most pushups and sit ups in one minute. BestMEDICINE Kids Subscribe to BestMEDICINE Kids and receive a monthly email featuring educational and inspirational stories dedicated to kids health and wellness from pregnancy through childhood. Join Today!
Read More About Not a Fall Sports Fan? Ways to Keep Kids Active
-
Why I Give: Sarah’s Story
As an avid soccer player, Sarah saw her fair share of doctors growing up. However, it wasn’t until she was diagnosed with celiac disease, an autoimmune disease affecting how the body ingests gluten, that she became passionate about healthcare. “I couldn’t figure out what was going on,” Sarah said. “I was getting sick, and my symptoms were getting worse.” Thankfully, after seeing a handful of doctors, she was on the path to recovery. “I remember being so relieved, and still am! Now I can focus on getting better,” said Sarah. The most important change people make after being diagnosed with celiac disease is the shift to a gluten-free diet. For many, Sarah included, living gluten-free is a lifestyle change. Thankfully, Sarah sees significant improvements in her health after adjusting her diet. “No one should just accept their symptoms as part of life,” said Sarah. Her increased awareness of health and nutrition motivated Sarah to study biology at the University of Nevada, Reno (UNR). “I want to be a pediatrician so I can help patients, especially kids, figure out treatment plans.” said Sarah who credits her experience living with celiac disease as her inspiration. Dancing for Kids’ Health Currently a senior at UNR, Sarah is a member of Phi Delta Epsilon, a co-ed international medical fraternity. Together with her classmates, she is bringing new energy and ideas to philanthropy. Sarah and the members of Phi Delta Epsilon are doing things differently and in many ways redefining what it means to give. This year, they are on a mission to raise funds for kids’ health at Renown Children’s Hospital. And they are doing this by dancing. The UNR Dance Marathon is part of the Miracle Network Dance Marathon, a student-led, year-round philanthropic movement that unites students across the United States and Canada. Collectively, they raise critical funds for Children's Miracle Network Hospitals. And Renown Children’s Hospital is our northern Nevada CMN partner hospital. Since 1991, over 400 college campuses and thousands of students have raised $300 million for kids. Sarah is the executive director of UNR’s chapter. “So far this year we’ve already raised $10,000 for Renown," said Sarah. Most of the fundraising happens on the day of the dance marathon. But throughout the school year, students hold mini fundraisers on campus and in the community. One hundred percent of the funds raised stay local, impacting Renown’s youngest patients. For every dollar donated, 18% helps provide charitable care, 15% goes to life-saving equipment, 12% supports medical research and 55% provides education, patient services and advancement services. “It's inspiring that we banded together to help kids in our community,” said Sarah. Last year they raised over $18,000. They are hoping to exceed that number at this year’s dance marathon in April.
-
Get Ready for Baby with Childbirth Classes
By taking our pregnancy and birth class, you will gain the tools necessary to have a safe and empowering birth experience for both you and your baby. Chris Marlo, Childbirth Educator at Renown Health explains why birth classes are important. For questions regarding classes or tours, contact Chris Marlo: chris.marlo@renown.org 775-982-4352 What is a Certified Childbirth Educator/Doula? If you are expecting a baby, Renown has a wide variety of classes to help prepare you for birth. Classes are taught by certified childbirth educators and doulas. A certified childbirth educator is a trusted resource who has a passion for educating expecting parents about childbirth, and will provide you with non-biased, evidence-based information. A doula is a professional labor assistant who provides physical and emotional support during pregnancy, childbirth and postpartum. As you prepare for birth, our certified educators will guide you each step of the way and ensure you receive the quality care you deserve. Why Should I Take Pregnancy and Birth Classes? For expecting parents, taking a childbirth education course is an important step in preparing for their new arrival. We cover topics such as labor and delivery, postpartum care, breastfeeding, nutrition, pain management techniques, and more. Our experienced instructors will provide you with the information you need to make informed decisions during your pregnancy and childbirth. With our classes, you can be sure that you have all the knowledge necessary to have a positive experience before, during, and after your baby’s arrival. Our classes will help ease your fears as we practice breathing, relaxation and the many tools you can utilize for birth. At Renown we understand that there is no right way to give birth, and our educators will offer a supportive environment where questions are encouraged, and everyone is respected. Childbirth Class Options: Baby and Family Suites Tour & Virtual Tour Breastfeeding Basics and Beyond Class Breathing & Relaxation Techniques for Birth Pregnancy and Birth – 5 & 7 Week Series Pregnancy and Birth Class Additional Resources: Baby Safe Class Babysitter Class Grandparents Virtual Class Infant CPR & Choking Class Newborn Care Nurturing Your Newborn Preparing for Postpartum Virtual Class