Search
-
Cancer Support FAQs: How to Help When It's Someone You Love
Every cancer journey is different — and so are the ways individuals deal with a cancer diagnosis. So if you’re a close friend or family member, how can you help? Bobbi Gillis, manager of cancer support services with Renown Institute for Cancer, explains more. Just as we are all unique, we all also have our own ways of dealing with difficult news. For some, receiving a cancer diagnosis is devastating, and they want family members rallying around them in support; for others, they want to be left completely alone. So how do you know what is helpful and what is hurtful? For advice, we reached out to Bobbi Gillis, manager of cancer support services with Renown Institute for Cancer. Support, Defined What are some ways to support a loved one when they find out they have cancer? First and foremost, let them know you are there for them. As we can all imagine, a cancer diagnosis is scary, and it’s helpful just to know you have support if and when you need it. Second, try to listen and give advice only when you are asked. In trying to help as much as possible, many family and friends take on the role of “researcher” to find out more treatment options, but it’s best to avoid saying “you should try this” or “you ought to do that.” Patients are already dealing with a lot of information at once from care providers and their own research. You don’t want to make them feel overwhelmed or question the treatment they’re planning. What are some words of encouragement or support people can use? Just as you would in any difficult situation, speak from the heart and be genuine. But also be careful not to show false optimism or to tell them to just stay positive; saying these things may discount their fears and concerns. Here are some ideas to get you started: “We’re going to get through this together.” “Count me in to help out.” “I’m not sure what to say, but I want you to know I care and I’m here.” What resources are available to patients? What about their families? For patients with cancer, we offer support groups in-person or online. There are also support groups specific to the type of cancer you or your loved one have. You can check these out on our website, renown.org, or ask your care provider. There are also support groups and emotional support services available for family and friends. How can family and friends help throughout cancer treatment? It’s great to offer help, but it’s important to be specific when you offer. Saying “call me if you need something” is very general, and people may feel like they’re putting you out when they do ask for something specific. Instead, offer help with certain tasks — like driving them to treatment, babysitting, making them dinner or buying groceries. As much as possible, keep things normal. For some patients, being able to do everyday things like walking the dog helps them feel better. Loved ones can try to do too much for a patient, and while well-intentioned, this can make them feel less useful after being diagnosed. Renown Institute for Cancer | 775-982-4000 At the Renown Health Institute for Cancer, our experienced team provides the support and care to maintain the highest quality of life and then achieve the best possible outcome, all in one location that’s close to home. Our dedicated team, clinical expertise and advanced treatment options allow us to tailor care to each patient. Learn about: Our Team Cancers We Treat Screening and Prevention Treatment Options Find a Doctor
Read More About Cancer Support FAQs: How to Help When It's Someone You Love
-
Keeping Research Close to Northern Nevada
Clinical research provides agency for our patients navigating a scary diagnosis, and the field has never been stronger in northern Nevada. This strength is thanks in part to the Affiliate Clinical Research Office (ACRO) formed by the 2021 affiliation between Renown Health and the University of Nevada, Reno School of Medicine. Since its creation, the ACRO team has been busy ensuring that community members have access to the latest care options and exceptional experiences as participants in both research and their healthcare. Here are just a few things that set this office apart from the rest. 1. A focus on engagement In 2022, the ARCO team focused on promoting a research culture with patients, clinicians, residents and students by intentionally engaging with healthcare providers, department administrators, internal research team members and leadership. They educated the community with learning materials that emphasized the importance of doing research. This team also worked with front-line staff to raise awareness and excitement about the clinical research options available for Renown Health patients. 2. Meaningful partnerships The most impactful partnership to date is between Renown Health and UNR Med. By identifying opportunities and leveraging resources across institutions, we have maximized our impact and built a solid and sustainable foundation. This gives the people of northern Nevada greater access to new interventions or novel treatments. This team is also investing in the community and national partnerships to provide training opportunities for our research staff and learning opportunities for our medical students. 3. Novel treatments across many disease areas Our research study offerings must reflect the healthcare needs of our community and the expertise of practicing clinicians. The department has over 80 active studies in neurology, pulmonology, oncology, cardiology, pediatrics and disease prevention. The ARCRO team strives to expand care opportunities to allow our community members to stay close to home when seeking care. This year, they will continue exploring our community's unmet healthcare needs by bringing new treatment options to the greater Reno area.
-
Getting to the HEART of Research
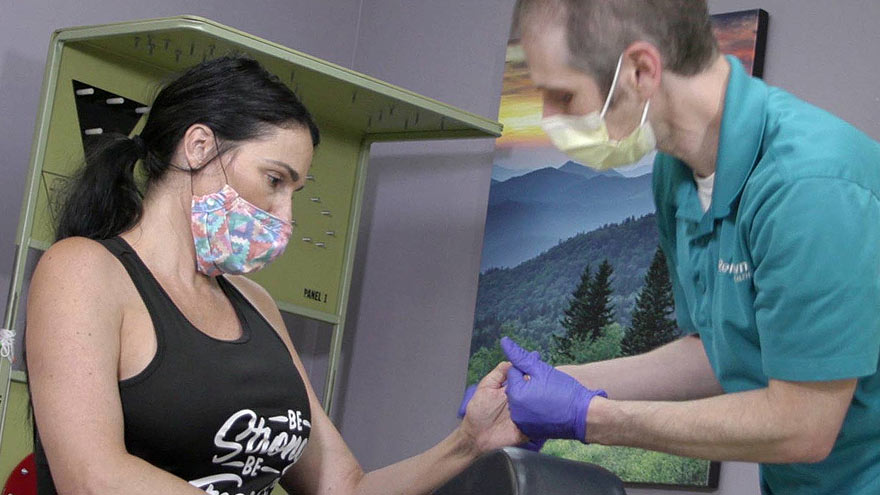
In February, we think about hearts not just in honor of Valentine’s Day but because it is American Heart Association Month. This is a great reminder to focus on our personal cardiovascular health. Renown Health helps patients think about their heart health with our world-class providers and cutting-edge treatments through our Cardiovascular Clinical Trials. “Research serves a vital role in the future care of cardiovascular diseases. Being involved in research will help our medical community to further discover new treatment plans in our quest for life preservation and extension,” Dr. Thomas To, Cardiologist and Researcher at Renown Health. For example, let’s talk about atherosclerosis. When our hearts are healthy, they are a strong muscle that pumps our oxygen-rich blood through our coronary arteries. Over time, cholesterol and fats can build up in our arteries. This is a condition known as atherosclerosis. This type of plaque buildup in the arteries can lead to a heart attack or stroke if not properly managed. If you are experiencing chest pain or discomfort, shortness of breath or pain in areas of the upper body, these can be the warning signs of a heart attack, and you should call 911. One contributing factor to atherosclerosis is elevated lipoprotein(a) levels and the accumulation of cholesterol in the arteries, which increases the likelihood of a heart attack or stroke. Lipoprotein(a) is tested separately from the standard panel that is completed for cholesterol management, and while your total cholesterol levels may be in a healthy range, lipoprotein(a) levels can still be elevated. "Increasingly we are realizing that lipoprotein(a) levels can be used as an important assessment in more carefully delineating an individual's risk of future cardiovascular events and treatment targets" said Dr. Michael Bloch, Lipid Specialist and Researcher at Renown Institute for Heart and Vascular Health. While it is clear that elevated lipoprotein(a) contributes to atherosclerosis, there are currently no approved medications for reducing cardiovascular disease risk through reducing lipoprotein(a) levels. This is why Renown Health’s Research Office is proud to offer a phase III clinical trial, called the OCEAN(a) study, to our patients with elevated lipoprotein(a) levels as a care option for management of their heart disease risk. Our teams of expert providers and researchers are here to support you on your healthcare journey. “I am thrilled to be able to be part of this study and bring opportunities like this to our patients. The highlight of my day is getting to hear life stories from my patients during our study visits,” Lisa Preciado, Primary Clinical Research Coordinator for the OCEAN(a) study said. Join us in raising awareness around American Heart Month by talking to your provider about lipoprotein(a) at your next appointment. At Renown Health, our goal is to make it easy for patients to access clinical research as a care opportunity where patients can access a variety of standard care treatment options for their health condition or choose to participate in a clinical trial. For more information about clinical trial opportunities available to you or to ask any questions, contact the Renown Research Office at Renown-CRD@renown.org or 775-982-3646.
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Stroke Survival as a Warrior – Kimi's Story
It seemed like a normal Wednesday, except Kimi Woolsey was feeling really stressed. On Sept. 4, 2019 she was rushing to get ready for an appointment when suddenly, she could not feel her legs. Kimi immediately knew something was wrong and called out to her fiancé, Paul, for help. After seeing a bright light in her right eye, she felt a severe, sharp pain in her head traveling down into her leg. Paul quickly called 911, the EMT’s arrived and her stroke survival journey began. At first the medical team thought she had a complicated migraine, but one of them suspected a stroke. On the way to the hospital Kimi felt numbness and her face drooping, then instantly, no pain. For a moment she thought she was dying, going from pain to numbness and realizing she couldn’t move or speak. Kimi didn’t know she was having another massive stroke in transit. Each year nearly 800,000 people in the U.S. suffer a stroke, or “brain attack” – that’s one every 40 seconds. Of those, about 75% occur in people over age 65. However, at only 45 years old, Kimi is proof that a stroke can happen at any age. Stroke Survival Begins for Kimi Upon arriving at the emergency department of Renown Regional Medical Center the Certified Comprehensive Stroke Center team went into action. Kimi received a brain MRI, then was wheeled into surgery for a thrombectomy (clot removal). She was in the intensive care unit for 11 days. She remembers someone telling her, “Generally people don’t survive this magnitude of stroke.” And a doctor saying, “You are here for a reason.” Kimi’s comeback journey began with the comprehensive care team at Renown Rehabilitation Hospital. “Literally I had the best day of my life that first day there…I was so happy because I couldn’t imagine being in a safer place with people that literally live for you,” she recalls. During her 41 days there, her biggest milestone was being able to get out of bed and walk. For Kimi the support she felt at the rehab hospital was key to her progress, ”I still feel loved and appreciated and they’re rooting for me still and I can feel it.” Although she left the rehab hospital on Oct. 18, 2019, she is still working on improving the left side of her body. Currently Kimi works with therapists in outpatient physical rehabilitation sessions, continuing to see improvement in both her hand and leg. Her advice to those currently in a rehab hospital setting is, “Stay as long as you can to get the most out of it and push, push, push.” Kimi’s Stroke Survival as a Warrior “Having a stroke is not for the faint of heart,” says Kimi. She experienced despair and felt discouraged. Many days she would ask herself, “Why am I here?” Today she proudly calls herself a stroke warrior and refuses to be a victim of her stroke. Alongside her tenacious spirit, Kimi actively helps others on their stroke survival journey. Before her stroke she never dreamed of starting a non-profit foundation. Now, each day you’ll find her texting inspiration to others, offering advice and connecting with other struggling stroke survivors on her Facebook page, Stroke Warrior Recovery Coach. Her goal is to become the person she needed to talk to after her stroke; she currently coaches several stroke survivors. “Stroke survivors need to know that they aren’t alone. Mental support and encouragement are so important for each person’s stroke journey,” Kimi said. Along with the physical changes, Kimi feels the stroke magnified her empathy. “I was always in a hurry in my life. People didn’t go fast enough for me – on the road, at the grocery store, in a line. Now I have more patience with myself and others." Kimi realizes most people cannot wrap their brain around the concept of a stroke. In fact, the brain fog, physical challenges and frustration are hard to explain… unless you’ve experienced them. “You need to find your tribe,” she explains. “I have a passion for helping people through this process.” Most of all, she encourages people to keep going and never stop. After her stroke, Kimi has a greater appreciation for her family, health and life. She is one of the patients featured in the current “Fight The Good Fight” trauma and physical rehab advertising campaign. “I wake up every day and fight,” she asserts. “Each day you have to fight for your recovery and fight for yourself.”
-
Heart Attack Survivor Fights the Good Fight
Something wasn’t right. Even though it was the holiday season, on December 23, 2018, Mondo Corona didn’t feel good…not to mention his sudden earache. Although Christmas was a happy celebration with his family. He still felt tired. Was it the flu? And that darn earache wouldn’t go away. On that cool winter day, Mondo could not imagine he was near death. Or that he would become a heart attack survivor. Know Your Heart A few days later, on December 27, he wasn’t feeling any better. He decided to go to the emergency room at Renown Regional Medical Center. That’s when a simple blood test revealed shocking results. “I thought about death a lot. I was calling people to ask them to help take care of my family if I wasn’t going to be here anymore,” he emotionally confesses. Although Mondo loves his job as a railroad engineer, it involves on-call shifts and an erratic sleep schedule. At that time his exercise and eating habits weren’t the best either. Yet he never imagined he would have a massive, often lethal, type of heart attack called ‘the widowmaker.’ In fact, his family had been concerned about his health for awhile. “He worked so much and he didn’t take care of himself and he didn’t exercise – he was burning the candle at both ends,” shares his wife, Alison. His daughter Justice, an avid exerciser, was always encouraging him to join her at the gym, but could never quite convince him. Mondo remembers the time before he became a heart attack survivor. “I didn’t have any exercise whatsoever in my life. At that point my eating habits were just terrible,” he shares. He went to the emergency room due to his earache, but nothing was found until one of the doctors ordered some tests. Specifically blood work showed high troponin levels. Troponin is a blood protein often released in large amounts when the heart muscle has damage, sometimes by a heart attack. Heart Attack Survivor “My surgeon came in and told us that it was going to be a triple bypass – that three of the four…major arteries were clogged 100 percent,” Mondo explains. Amazingly his heart was pumping on only 10 percent blood flow. Heart surgeon, Joseph Brandl, MD, told him he survived a widowmaker heart attack. This type of heart attack happens when there is a 100 percent blockage in the critical left anterior descending artery (LAD) of the heart. Frequently the symptoms can often be mistaken for the flu. According to the Centers for Disease Control and Prevention (CDC), every 40 seconds a person in the U.S. has a heart attack. And 1 in 5 heart attacks are “silent” – meaning you can be a heart attack survivor, but not know it. For Mondo’s children, seeing their strong father struggle after heart surgery was difficult. Justice tearfully shares, “It was really hard seeing him so vulnerable. He really needed anybody’s and everybody’s help at that point.” A Heart Attack Survivor Program After leaving the hospital on January 5, 2019, he was extremely weak. On February 12, Mondo began Renown Health’s Intensive Cardiac Rehabilitation (ICR) Program called the Healthy Heart Program. This program, requiring a doctor referral, includes 12 weeks of supervised exercise along with nutrition education and stress management skills. In spite of heart disease being the leading cause of death in the U.S. – more than all cancers combined, the risk can be lessened with daily lifestyle habits. Mondo credits the ICR program with motivating him and getting his focus back on his health. He saw the team members setting an example and also caring about his health. He describes one of his favorite recipes, “In ICR Sara showed us how to make this incredible fruit salad, with jicama, watermelon, grapes, oranges, red onion, and ginger!” Of course, the recovery process was not overnight. “It did take a long time to really realize that he was going to be back to normal, that he was going to be okay and that he was going to be that strong provider for me and my children,” Alison reflects. “Mondo’s had an amazing outcome and he’s not limited in his activities at all and should hopefully have a life that’s not limited at all from heart disease as we’re monitoring everything and everything’s looking good,” reports his heart doctor Jayson Morgan, MD. Mondo describes his care experience being a heart attack survivor as life-changing. “The care teams at both Renown and ICR were incredible. There wasn’t a single person we came across who didn’t immediately become a part of the family. They truly cared for us, all of us, including the extended family that came to visit. They were informative and supportive. I felt like I created lasting bonds with so many of them, especially the gang in ICR. What amazing people.” Lynice Anderson, Director of Intensive Cardiac Rehab, Healthy Heart Program, shares,” Mondo is one of the most genuine, thoughtful and humble people I have ever met. His love for his family is palpable. His impact on me personally and our team is forever.” She acknowledges family support is key to his success, “Mondo’s family is his rock and they are his. I have never met a family that was so ‘all in’ in the support of their loved one. His new heart healthy lifestyle is modeled through his family every day.” Fighting The Good Fight Of course, Mondo may look familiar to you. That’s because he is featured in Renown Health’s “Fight The Good Fight” brand campaign. For this reason, you may have seen him in advertising working out on a treadmill, shirtless, with his open heart surgery scar in full view. When asked how he feels about showing his scar he confidently says, “I don’t mind showing it to people. I don’t. I earned that scar.” He is a proud heart attack survivor. Today, he’s grateful to be alive and takes his health commitment seriously. “Things have a different feel now. The skies and lakes are bluer and the trees greener. My family is so much more a part of my day. We go on so many more outdoor adventures, trying to incorporate a little exercise into our fun. We watch what we eat more and are trying to teach our children and loved ones about healthy choices. And I think with a few we’ve even been successful!” he observes. “Don’t take life for granted.” “Unconditional love. I get nothing but support from my family without them I wouldn’t be where I’m at. What happened to me definitely makes me a fighter for sure. I’m fighting for my life – the good fight – I think life is good,” he adds.
-
Helpful Caregivers Make a Wedding Dream Come True
A wedding is a big day for the wedding couple, but it’s also special for loved ones. A patient at Renown, Ken, got to take part in his daughter’s special day as her wedding plans changed to accommodate his medical condition. Grab some tissues and read how Renown’s team of compassionate caregivers and chaplains planned a wedding in Fianna’s Healing Garden. Ken was hospitalized at Renown Regional Medical Center where he was battling a lung problem – which was unrelated to COVID-19 – and his condition worsened rapidly on Wednesday, Aug. 12. His family made the decision to transition him to palliative care, which helps patients near the end of their lives remain comfortable, while supporting their dignity and quality of life. Ken’s medical condition altered wedding plans for his daughter, Chandra, and her fiancé, Tyler, who were planning to tie the knot later in 2020. Chandra wanted her father there, but knew he could not leave the hospital. That’s why Chandra’s sister, Heather, approached Ken’s care team with a request to have a small wedding ceremony at the hospital. Planning the Wedding A member of Ken’s care team, Amy Heston, registered nurse (RN), began planning how the wedding could be held outdoors in Fianna's Healing Garden in the E. L. Wiegand Pavilion, which was donated by the E. L. Wiegand Foundation. In 24 hours, Amy planned a wedding ceremony with the help of her colleague, Breyanna Aufiero, RN; the Renown Spiritual Care team; and nursing leaders on the coronary intensive care unit (ICU). Together, they decorated the aisle in the garden with flowers and battery-operated candles. They also made a sign for Ken’s hospital bed, which read, “Father of the Bride,” and crafted a bow tie for him to wear for the special occasion. With visitor restrictions in place at the hospital due to coronavirus (COVID-19), having the wedding outside in the Healing Garden allowed for more members of Ken’s family to attend including his wife, Charlotte, and his dog, Bella. Every step in planning the wedding required thoughtful and thorough care coordination so Ken could participate. His breathing was supported by oxygen and special arrangements were made to transport the oxygen tanks he needed to take part in his daughter’s wedding. Amy worked with respiratory technician, Kasey Benfield, and critical care technician, Ruben Duckworth, to ensure Ken’s oxygen needs were met using portable machines. Celebrating Love and Life Together Ken’s team of caregivers bathed him and shaved his face so he could look and feel his best for the ceremony. They put on his bow tie, covered his bed in decorations and his favorite blue, flannel blanket, and wheeled his bed outside for the ceremony. Renown associate chaplains Terri Domitrovich and Susan Palwick coordinated music and performed the ceremony for Chandra and Tyler on Thursday, Aug. 13, 2020. The bride and groom shared their first dance in the garden and Ken’s care team provided water and treats to give the family a full wedding experience. Shortly after the ceremony, Ken passed away. This wedding provided Ken and his family meaningful memories for their big life-changing moments as they celebrated and said goodbye. “Seeing Ken surrounded by family he never would have gotten to see again while in the hospital, watching him get to share a father-daughter dance with Chandra on her wedding day, and having him tell me that this day meant more to them than we would ever know were some of the most moving moments I’ve witnessed as a nurse,” Amy said. “I am so thankful for the team we have here. I know that this beautiful day wouldn’t have happened without the help of every single person who gave their time, money, creativity and passion to make it a day to remember.”
Read More About Helpful Caregivers Make a Wedding Dream Come True
-
Cancer Nutrition - Helpful Tips to Support Your Loved One to Eat Healthy
Eating healthy is a daily challenge for many, but for those with cancer it is an even harder struggle. A cancer diagnosis not only impacts those diagnosed, but family members and friends too. One key area of concern is making sure your loved one stays well by eating healthy food every day. Here are some essential cancer nutrition tips from Renown Health registered dietitians Jessica Blauenstein and Amy Laster. Help to Prepare Meals and Snacks for Daily Cancer Nutrition Make it grab and go. Easy-to-make meals help reduce the burden of having to cook and prepare food. Having easy to grab snacks on the counter or in the fridge can help ensure your loved one has access to those nutrients when needed. Sit outside of the kitchen. This allows your loved one to avoid cooking smells which can make them feel sick as a side effect of cancer treatments. Also try serving them cold foods such as sandwiches, cheese and crackers, or shakes which have a mild scent. Try drinkable meals. Some people with cancer find it easier to sip their calories over the course of 30 minutes to an hour. Consider smoothies or supplemental shakes such as Ensure Enlive or Boost Plus as snacks not meal replacements. A great foundation for a smoothie is a protein source (Greek yogurt, protein powder, nut butters or milk) with a carbohydrate (fruits, juice or berries). Add other ingredients as desired, such as spinach, kale, and ground flaxseed or chia seeds to give it more vitamins, minerals, and fiber. Snack Ideas for Those Undergoing Cancer Treatment The following ideas are both quick and easy to make for your loved one. Chicken or tuna salad with whole grain crackers or as a sandwich on whole grain bread Greek yogurt mixed with cereal, fruit and/or nuts Cottage cheese with banana, cinnamon and/or peanut butter Favorite fruit with 100% natural peanut or almond butter spread - Try peanut butter with bananas, apples, or even celery Their favorite veggies dipped in a salad dressing of your choice - For example, carrots with hummus or ranch dressing Cheese and whole grain crackers - Add tomato slices with a dash of oregano on top for more flavor Eggs scrambled with cheese, vegetables and/or salsa Peanut butter and jelly sandwich on whole grain bread A baked sweet potato with some favorite toppings Hard boiled eggs and/or egg salad with whole grain crackers, or as a sandwich on whole grain bread Oatmeal or cream of wheat prepared with milk, fruit and/or nuts Sometimes your loved one may not feel like eating or refuse to eat. If treatment side effects are impacting your loved one’s ability to eat, please visit the websites below containing recipes tailored to treat side effects. Cook for Your Life ELLICSR Of course you may also consult a registered dietitian and/or the patients care team, if you have more cancer nutrition concerns. No Appetite? Assisting with Cancer Taste Changes Taste changes are common during cancer treatment. Patients experiencing these changes may not feel like eating, which can negatively impact their nutrition. Help your loved one overcome taste changes with these cancer nutrition strategies: Metallic or bitter taste in food - add something sweet such as maple syrup, honey or jelly. You may also try adding fat, such as a nut butter, avocado or regular butter. Pickles or vinegar could help with this too. A taste like cardboard - try adding salt and extra flavor to foods with seasonings and spices. Some examples are onion, garlic, chili powder, basil, oregano, rosemary, tarragon, barbecue sauce, mustard, ketchup, or mint. Lemon juice, citrus, vinegar, or pickles may also help with this as well Food tastes too sweet - try adding six drops of lemon or lime juice. Add small amounts until the sweetness is gone. Very salty taste - try adding ¼ teaspoon of lemon juice. Try plastic utensils instead of metal, especially if your loved one is struggling with foods tasting metallic. Dipping small bites of food into either lemon juice or vinegar can have a “palate cleansing” feel and may improve taste perception. This helps avoid getting tired of the flavor after a few bites. Try marinating food or meats in sweet fruit juices, salad dressings, or sweet-and-sour sauce. Other “palate cleansing” foods are lime juice, orange juice, mangos, lemongrass, parsley, cilantro, mint, ginger, basil, and pickled foods. Use aroma to make foods appealing, avoiding any smells that may cause nausea. In particular, cinnamon, nutmeg, cloves, coriander, cumin, ginger, and black pepper can add an aromatic flavor. Also include herbs such as oregano, rosemary and thyme. Think texture. Consider trying wafers, crunchy nut butters, carrots, celery, cucumbers, chips, rice crispies, corn flakes, crackers, panko crumbs, nuts, or seeds if you are able to chew and swallow them safely. Remember that patience with your loved one's changing appetite and tastes can be the strongest form of support you can provide. Nutrition Tips for Cancer Survivorship and Beyond If eating large meals is difficult for your loved one, encourage them to snack throughout the day. Aim for 4-6 snacks or small meals per day. Focus on consuming 2-3 protein-rich foods each day such as lean animal meats, fish, eggs, soy or a protein supplement with 20-30 grams of protein per serving. Eat a variety of brightly colored fruits and veggies. Aim to make half of each meal fruits and vegetables. Eat less than 18 oz. (cooked weight) of red meat per week. Limit cold cuts, bacon, sausage, and hot dogs. Avoid excess salt and saturated fats. Cut back on simple carbs. (i.e. desserts, candies, white bread/pastas, french fries, packaged foods, chips) Drink in moderation- if at all- one drink per day for women, two for men. Get enough vitamin D (through diet and/or supplement) Avoid tobacco of any kind. Keep a healthy weight and stay up on exercise. Other Ways to Help a Loved One with Cancer Assist with Chores Allow your loved one to relax as you help take care of chores around the house, such as cleaning, cooking and grocery shopping. This may reduce overall stress and can be helpful for those that get tired after their treatments. Physical activity can still be beneficial, so be sure to do an activity together that they enjoy and is approved by their doctor. Be Patient It can be very difficult to see a loved one go through cancer treatment. Remember to be patient with your loved one. There may be things we want them to do or eat that we know would be good for them, however, meet your loved one with grace and understanding. It is ultimately their decision on what to do, just be there to support and assist them as they go through this challenging time. Additionally, Renown hosts free “Eating Well After Cancer Treatment” nutrition classes for cancer survivors. Our next cancer nutrition class series starts Thursday, June 3, 2021, and will be hosted virtually. It is open to anyone in the community. For more information or to register please click here.
Read More About Cancer Nutrition - Helpful Tips to Support Your Loved One to Eat Healthy
-
Ovarian Cancer Survivor Shares Decision to Try Clinical Trial
While there used to be three basic treatment options for cancer -- surgery, radiation and chemotherapy, or a combination of the three -- there's a fourth option: clinical trials. Here, a Renown patient shares her successful battle with ovarian cancer, aided by a clinical trial. Shari Flamm's battle with ovarian cancer began in 2011. She was experiencing prolonged bleeding, irregular thyroid levels and anemia and was scheduled to undergo a hysterectomy. Before the surgery, her gynecologist ran routine tests to check for cancer as a precautionary measure. All tests were negative for cancer, expect her CA 125 test. A CA 125 test measures the amount of the protein CA 125 (cancer antigen 125) in the blood. In some cases, a CA 125 test may be used to look for early signs of ovarian cancer in women with a very high risk of the disease. In most laboratories, the normal level is 0 to 35 units/ml. Flamm's CA 125 level was 121. As Flamm can attest, early diagnosis played a key role in her battle with ovarian cancer. September is Gynecologic Cancer and Ovarian Cancer Awareness Month – an important time to learn the signs, symptoms and risk factors of this type of cancer so your doctor can diagnosis the disease as early as possible. Ovarian Cancer: Round One Despite the elevated CA 125 results, her doctor recommended they move forward with the hysterectomy. But when surgery began, doctors discovered a mass. She had stage 4 cancer. The procedure was halted, the mass was biopsied and she was immediately seen by Dr. Peter Lim of the The Center of Hope. Following diagnosis, Flamm underwent surgery with Dr. Lim to remove the cancer, which had spread to part of diaphragm, spleen, colon and other organs. Three months after surgery, Flamm had recovered enough to start six rounds of chemotherapy in her hometown of Carson City. She continued working at a doctor's office during her treatment, and was grateful for Dr. Lim’s ability to co-manage her care so she could stay close to work and family. “To me, chemo was the scariest part because I didn’t like feeling sick,” Flamm says. Thankfully, her body responded well to the treatments and she was back to the things she loved. “I stated working out at the gym, even if it was only for 10 minutes,” she says. She also stayed positive by spending time with her grandchildren, attending a San Jose Sharks hockey game, going for walks and enjoying concerts. Ovarian Cancer: Round Two In November 2014, Flamm had a cancer check-up. That’s when doctors discovered three cancerous tumors. For this round, Flamm choose another treatment option -- clinical trials at Renown Institute for Cancer. Clinical trials are the studies that test whether drugs work, and inform doctors' decisions about how to treat their patients. Flamm participated in a clinical trial that featured oral-targeted therapy stronger than IV chemotherapy. The hope was for the drug to shrink her tumors, however the result was stabilization -- meaning the lumps weren’t growing or spreading. The best part of the clinical trial, Flamm says, was the constant monitoring. Between the CT scans every six weeks, a heart scan every three months and monthly doctor visits, she was confident that if the cancer started growing or spreading, her healthcare team would catch it right away. For Flamm, the benefits of the clinical trial included less hair loss, less fatigue and more time to focus on what’s important in her life -- her family. “I decided I wasn’t going to be that sick grandma on the couch with cancer,” Flamm says. After taking the oral medication for one year, Flamm developed a rash and discontinued treatment due to discomfort. Clinical Trials, Setbacks and Survival In June 2016, two of the three tumors began to grow and had to be surgically removed. Despite the setback, Flamm was determined to maintain a positive outlook. "You have to stay positive because cancer feeds off anger, depression and stress," Flamm says. Flamm was released to go home with clear margins, meaning the tumors were removed and are surrounded by a rim of normal tissue that does not have cancerous cells. Flamm says her outlook on life has changed drastically since her first cancer diagnosis. “Your whole mentality changes when cancer disturbs your life," Flann says. "The things that weren’t important, are now ever so important. I’m a lot calmer now,” Flamm says.
Read More About Ovarian Cancer Survivor Shares Decision to Try Clinical Trial
-
From Cancer Survivor to Caregiver
Meet Haley Carroll Being a new nurse comes with many challenges and gaining experience is a journey, but Haley Carroll’s first day on the job was far from her first day in a hospital. Haley was diagnosed with lymphoma right before her senior year of high school, and she was declared cancer-free on December 2, 2015. Inspired by the incredible care she received during her cancer treatments and during her time at Renown Children’s Hospital, Haley enrolled in nursing school at the University of Nevada, Reno. She graduated in December 2020, just five years after beating cancer. “I’ve always been interested in nursing,” Haley says. “But once I was diagnosed and began to see everything that my nurses did for me, I knew that that’s what I wanted to do for patients, too.”
-
The Road to Recovery Close to Home
Meet Connor Smith Life was hectic for Connor Smith. He had just finished at the top of his class at both the fire academy and paramedic school and was looking forward to starting work in northern Nevada. It was winter 2019, and he was ready to have some fun. The plan was to ride ATVs at Sand Mountain with his brother Cody, dad Lance and some friends, but a jump would change everything. Connor’s ATV took off but landed awkwardly, and he remembers immediately knowing he was paralyzed. Connor’s mom, Dana Shugar, was at home when she received the upsetting call from Cody, who told her he had an accident. Connor was flown to Renown Regional Medical Center, the area’s only Level II Trauma Center. After a seven-hour emergency surgery, Dana learned that Connor would live but only had a slight chance of walking again due to a spinal fracture. “The surgeon saved his life. It’s amazing how your life can change in a matter of seconds,” she said. Once his condition stabilized, Connor moved to the Renown Rehabilitation Hospital and began physical rehabilitation. “Thank God for the people at rehab,” Dana said. “Dr. Pence, the therapists, nurses and all the employees were a wonderful support system, explaining everything and answering all our questions. The kindness they showed got me through.” Connor agrees, calling the Renown rehab team nothing short of amazing.
-
A Family's Legacy
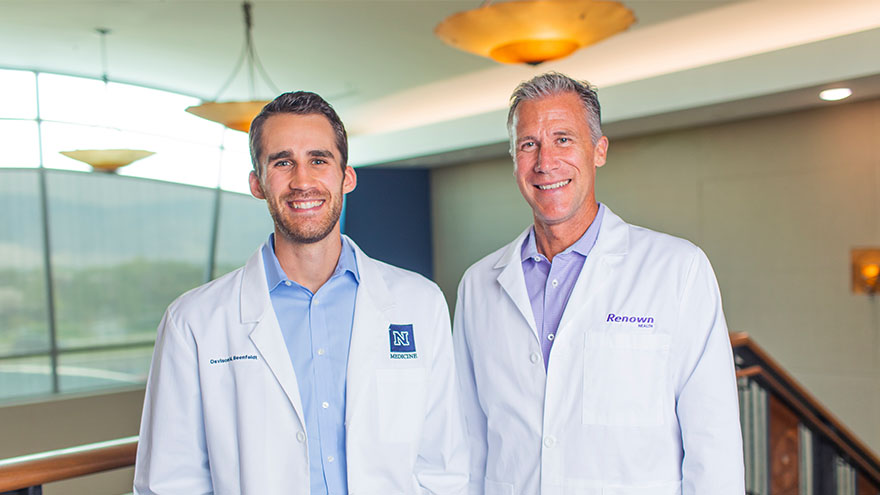
Dr. Derek Beenfeldt first joined the Renown family in 2014 as a family medicine physician after graduating from University of Nevada, Reno, School of Medicine (UNR Med) in 2011. His son Davis was only 10 years old when Dr. Beenfeldt decided to change careers and attend medical school. Ten years later, Davis is following in his dad’s footsteps as a third year student at UNR Med. “I am proud of Davis for taking on the challenges and the commitment that I know goes along with attending medical school,” Dr. Beenfeldt said. “I also feel lucky that we have a medical school with such a great reputation and resources close to home.” The affiliation is a great source of pride for Dr. Beenfeldt. Not just because two important organizations in his life are joining forces, but he also sees it as both entities taking on an immense responsibility – the challenge to be better for incoming students, and subsequently to improve healthcare in Nevada. Davis is currently going through his rotations and spending countless hours a week at Renown Regional. His dad is right there by his side supporting him along the way. “It has been really interesting to have discussions about the UNR medical school with Davis, I recognize the names of many of the professors and courses from when I was a student,” Dr. Beenfeldt said. “I tried to be empathetic, as I can relate to how difficult and stressful this time is for him. Dr. Beenfeldt currently works as chief medical officer for Renown’s insurance arm Hometown Health, and Davis is still browsing specialties. “I don’t know what kind of medicine I want to focus on yet, but I feel lucky that I can attend medical school so close to home and have the option to continue helping my fellow Nevadans after I graduate.” UNR Med at a Glance UNR’s Medical School was established in 1969 Over the last 50 years, UNR Med has educated 3,900+ physicians More than 30% of UNR Med physician graduates continue to practice in Nevada UNR Med is the state’s oldest medical school