Search
-
CEO Blog: Improving Health Through Genetics and Big Data
Renown Health President and CEO Tony Slonim, MD, DrPH, discusses efforts nationwide to develop a more effective and efficient way to deliver care. explains the benefits of Renown Health’s population health study with the Desert Research Institute and 23andMe.
Read More About CEO Blog: Improving Health Through Genetics and Big Data
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
How Philanthropy Helps Address Gaps in Care
In Nevada, we are so fortunate to have a number of not-for-profits and philanthropists who are supporting our mission at Renown Health; we couldn’t do it without them. In the world of healthcare, we are doing well in driving community benefit programming through operations. However, the things our communities need investments in are so much broader than we might be able to afford on our own. That is why it is essential for us to be supported by the people who are so in love with this community and want to assure we get the kinds of services and care for those who can’t afford it or add new services that are contemporary and leading edge that have not been offered here before. Establishing Behavioral Health & Addiction Institute We are so excited to receive a very generous donation from Chuck and Stacie Mathewson for the Stacie Mathewson Behavioral Health & Addiction Institute. This institute is so sorely needed in northern Nevada. Renown Health has a very important role in being able to bring attention to this important problem of mental health and addiction challenges in northern Nevada. Keeping Pediatric Care Close to Home One of the most important areas where philanthropy comes in handy for us at Renown Health is by assuring that we have the foundational programs that we would not be able to afford with operations alone. For example, the William N. Pennington Foundation’s generous gift has allowed us to create 15 pediatric specialty areas here in northern Nevada so children who have an illness or injury no longer need to leave town. The William N. Pennington Foundation supported Renown Children’s Hospital in a way that we never would have been able to support on our own. We are eternally grateful, and their gift — that 100,000 children are assured access to contemporary health and healthcare services — is beyond comprehension.
-
Reno Widow Inspires New Visitor Policy for Renown
Renown Health is one of the country’s first health systems to lift visitor restrictions for patients with COVID-19 and encourage the family to be at the patient’s bedside. Read Darlene and Dave’s story to understand why we’re updating our visitor policy. Dave and Darlene Randolph found joy in exploring antique shops and garage sales to find damaged or discarded vintage pieces. Dave would spend many hours scraping, cleaning, sanding, and refinishing items, transforming them into functional, beautiful pieces of furniture. Every piece in their home rekindles a memory and has a story to tell. On Thanksgiving, when Dave was too ill to gather around their antique dining room table, Darlene called the ambulance. Ailing with COVID-19 for two weeks, Dave had not been improving. When the EMTs reached her home and asked Darlene what underlying conditions he had, she said, “all of them.” David was seriously ill. Hospitalized for COVID-19, their communications options were limited. The only way Darlene could communicate with Dave was on a video call or by telephone. Dave spent 17 days hospitalized at Renown Regional Medical Center in Reno. Darlene spent 17 days waiting by the phone for more information on his condition. Darlene said he had “up days and down days,” but thought he might be home, sitting at their antique dinner table for Christmas. Sadly, Dr. David Randolph lost his battle with COVID-19 on December 13, 2020, and died as he slept in a hospital bed. When Darlene wrote his obituary for the newspaper, she gave thanks to the “tremendous nurses and doctors at Renown Regional Medical Center, for providing his care during a time when the family could not be with him.” Taking Action to Inspire Change Darlene wished she could have been there. Over their 45-year marriage, she had always been there. Darlene said, “I had always been at his bedside, as his advocate, to help communicate and straighten things out.” As a registered dietician, she worked in hospitals, knew the protocol, and knew that Renown had a restricted visitor policy to stop the virus’s spread- to other patients, staff, and their family members. Still, she wished she could have spent more time with him. On Christmas Eve, she sat down and wrote to Renown leadership. “As the wife of a COVID patient who recently passed away in your hospital, I want to express my thanks to you and your staff for the care he received in the last days of his life. I am aware that the nurses and staff are working under dangerous conditions and risking their health and lives by caring for multiple COVID patients. The staff is gracious, concerned, and doing everything they can.” She continued, “I know procedures are changing every hour to try to stay ahead of this dangerous virus, and I am sharing my experiences, hoping they will be helpful when establishing policies that impact families.” Darlene explained that despite receiving assurances that Dave’s nurse or a doctor would call daily, sometimes they would forget. She explains in her letter, “how important it is, in these times when the family cannot visit, and has only infrequent communication and is anxiously waiting at home for information about their loved one, how much it means to get a call from someone caring for him at the hospital. If there is a way you can help assure nurses have time to make calls or assist patients in making calls because it is an important part of patient care.” A Person-Centered Visitor Policy After receiving her letter, Renown leadership called Mrs. David Randolph to thank her, offer his sympathies and ask if Renown could help in any way. Darlene asked if he might reconsider allowing families to visit hospital patients during treatment for COVID-19. As the COVID-19 situation has evolved, the policy has as well. Renown hospitals and medical practices now encourage limited visitors for all patients, including those diagnosed with COVID-19. Renown also has extra safety measures to protect the health of patients, visitors and healthcare employees. Darlene is very pleased that her letter inspired this shift in visitor policies for patients with COVID-19. She says, “I have always tried to think of ways I could help other families. Especially those senior couples where one has been hospitalized and the other is home. My wish is to help others.” Renown Health Visitor Policy Renown Health patients may identify two healthy adult “patient supporters” to accompany them on their hospital stay. For more details, visit our Patient Supporter Guidelines page.
Read More About Reno Widow Inspires New Visitor Policy for Renown
-
Workplace Violence: Protecting Healthcare Workers
Over the past year, the safety of healthcare providers has received more public attention than ever before. Throughout the COVID-19 pandemic – and particularly in the early days – the public learned about the vital role of personal protective equipment (PPE) and other important processes that keep healthcare workers safe and healthy. However, people may be surprised to learn that germs and viruses are just one of the many risks that healthcare professionals face every day. Many people are fortunate enough not to have to worry for their physical and mental wellbeing when they go to work. Unfortunately, this is not the case for countless healthcare workers across the nation, for whom workplace violence is a daily concern. According to the American Hospital Association, healthcare workers are four times more likely to experience serious workplace violence as people in other industries. This is particularly troubling knowing that healthcare workers have dedicated their careers to serving others, putting their communities first day in and day out. Responding to the Challenge of Workplace Violence At Renown, we have no tolerance for abuse against our employees. As an organization, we have several systems in place to support and protect our staff. During staff orientation, we provide classes to prepare employees to prevent and de-escalate verbal or physical abuse. We also offer ongoing education to train our staff to respond to violent situations. If an incident does occur, our violence prevention task force reviews incidents and ensures the impacted employees receive resources and counseling to help them process what has occurred. As a leader, I am continually impressed by our team’s desire and ability to support one another. However, I know that it is my responsibility to protect our team. No one should have to face harassment or abuse – in any form – in their workplace, and I think about the risks our employees face every day. I believe so much in this cause that I volunteer on the American Hospital Association’s Hospitals Against Violence steering committee, which works to understand the causes behind violence against healthcare workers and develops tools and processes to prevent these incidents from occurring.
Read More About Workplace Violence: Protecting Healthcare Workers
-
Hiking Through Life After TAVR
Renown Health patient, Alden Nash, hiking Death Valley National Park just three months after a Transcatheter Aortic Valve Replacement. Alden Nash isn’t your average 80-year-old. For much of his life, he could be found outdoors enjoying nature and hiking some of the west coast’s highest elevations. A husband and father of two, Alden turned his passion into a career as a Yellowstone park ranger in 1965. Alden believes his passion for the outdoors is responsible for his many years of health – until the unavoidable happened. The Hardest Climb The number one doctor recommendation for a healthy heart – lead a healthy, active lifestyle. Any cardiologist would be thrilled to have Alden as a patient due to his robust physical activity regimen. “Don’t have a TV set or a lounge chair in your house and you’re all set,” said Alden when asked how he has remained so fit throughout his senior years. Unfortunately, many other factors come into play when it comes to heart health, one of which is the reason we are telling Alden’s story today. Familial history - it’s a hot topic in the world of medicine. Understanding your genetic risk factors can help care providers develop updated care plans based on your results. Alden’s family has a long history of high cholesterol, which he avoided for much of his life by staying active. This combined with his age resulted in his first heart attack in December 2021. Doctors later determined that Alden was suffering from a type of heart valve disease known as aortic valve stenosis. Aortic stenosis is the narrowing of your aortic valve opening that impedes normal blood flow. Over time, the leaflets of your aortic valve become stiff, reducing their ability to fully open and close. When the leaflets don’t fully open, your heart must work harder to push blood through the aortic valve of your body. Eventually, your heart gets weaker, increasing the risk of heart failure. People who are most at risk for aortic stenosis include those who have had certain heart conditions present at birth, have chronic kidney disease or have heart disease risk factors such as high cholesterol and high blood pressure. However, generally, aortic stenosis is a degenerative process of aging with no modifiable risk factors. The incidence of aortic stenosis increases rapidly with age and is very common above the age of 80 – with 1/10 having the condition and 1/50 with a problem severe enough to warrant surgery. When symptoms are present, the disease can be rapidly disabling or even deadly, often progressing over several months unless treated.
-
Kindly Care for Those Who Care for You
Over the past year, the safety of healthcare providers has received more public attention than ever before. Throughout the COVID-19 pandemic – and particularly in the early days – the public learned about the vital role of personal protective equipment (PPE) and other important processes that keep healthcare workers safe and healthy. However, people may be surprised to learn that germs and viruses are just one of the many risks that healthcare professionals face every day. Many people are fortunate enough not to have to worry for their physical and mental well-being when they go to work. Unfortunately, this is not the case for countless healthcare workers across the nation, for whom workplace violence is a daily concern. According to the American Hospital Association, healthcare workers are four times more likely to experience serious workplace violence than people in other industries. This is particularly troubling knowing that healthcare workers have dedicated their careers to serving others, putting their communities first- day in and day out. What is Considered Workplace Violence? The World Health Organization (WHO) defines workplace violence as, “Incidents where staff are abused, threatened, or assaulted in circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being, or health.” WHO considers both physical and psychological harm, including attacks, verbal abuse, bullying, and both sexual and racial harassment, to be workplace violence. Responding to the Challenge of Workplace Violence At Renown Health, we have no tolerance for abuse against our employees. As an organization, we have several systems in place to support and protect our staff. During staff orientation, we provide classes to prepare employees to prevent and de-escalate verbal or physical abuse. We also offer ongoing education to train our staff to respond to violent situations. If an incident does occur, our Violence Prevention Task Force reviews incidents and ensures the impacted employees receive resources and counseling to help them process what has occurred. We are among the first in the nation to have instituted a Zero Tolerance policy on workplace violence. This policy is in place to let our employees know that we have their backs in preventing workforce violence and we will address it assertively if the environment becomes unsafe. As a leader, I am continually impressed by our team’s desire and ability to support one another. However, I know that it is my responsibility to protect our team. No one should have to face harassment or abuse – in any form – in his or her workplace. I believe so much in this cause that I volunteer as Chair of the American Hospital Association’s Hospitals Against Violence steering committee, which works to understand the causes behind violence against healthcare workers and develops tools and processes to prevent these incidents from occurring. Violence was already a concern facing health care organization leaders prior to the COVID-19 pandemic. Now, the ongoing health crisis has elevated tensions. Health care is an industry like no other, with our most precious resource being our employees. As a community, as patients and family members, we have an obligation to ensure that all healthcare workers are safe while they go about their work. This starts with understanding, communication and unequivocal support for the profession. This month we launched the Be Kind campaign across Renown, a reminder to all of the importance of values like patience, kindness and gratitude. If you would like to join us in recognizing a healthcare hero, please submit your thoughts here. Thank you for working with us, and all healthcare providers, to create and maintain places of health and healing for all – and for kindly caring for those who care for you.
-
Plan Early: Completing Your Advance Directive
We plan for the birth of a child, weddings and retirement, but rarely do we discuss how we want to be cared for at the end of our lives. Getting through this challenging conversation and completing an Advance Directive can give you peace of mind that your loved ones will not have to make difficult choices on your behalf. The best time to complete an Advance Directive is now – don’t wait until a life-limiting illness or crisis occurs to discuss your views about end-of-life care and to learn what choices are available. By preparing in advance, you can help reduce the doubt and anxiety related to decision-making for your family if you cannot speak for yourself. What are Advance Directives? An Advance Directive is a document that states your choices about medical treatment and names another person to make medical decisions on your behalf if you are unable to. This document allows you to make legally valid decisions about future medical care. “Completing your Advance Directive is a gift you give your family,” says Director of Palliative Care, Mary-Ann Brown RN, MSN. “The stress associated with these difficult decisions is decreased if everyone knows what is important to you and what you want at the end of life.”
Read More About Plan Early: Completing Your Advance Directive
-
Getting Care During The Holidays
Although coined the most wonderful time of the year, the holiday season can unfortunately bring with it injuries and illness. Woke up on Christmas morning with the gift of a sore throat and fever? Sliced your finger carving the delicious turkey you spent all day preparing? While no one ever wants to cut their festivities short, the reality is we should all be prepared with how and where we will receive care should we need it. Are Renown Urgent Care Facilities Open During the Holidays? Renown Urgent Care sees patients 365 days a year, with limited hours on holidays, for medical concerns that are urgent but not life-threatening. Urgent care providers can treat everything from cuts and burns to fevers and allergic reactions and appointments can be booked ahead of time online. If no appointments are available, you may also walk into any of our various urgent care facilities. Conditions and injuries treated at urgent care include: Cuts Fractures Burns Sprains Fevers Allergic reactions Animal bites Rashes Sore throats Does Renown Offer In-Home Care Options on Holidays? If you’d like to see a healthcare provider without leaving the house and exposing others to illness, consider a Virtual Urgent Care Visit. This convenient video conference service allows you to see an urgent care provider from the comfort of your home using a cellphone, computer or tablet with video capabilities. Providers are available for video chat from 9 a.m. to 6 p.m. Monday through Friday, and 10 a.m. to 4 p.m. Saturday and Sunday. Scheduling a Virtual Visit is easy directly through MyChart. Login to MyChart and click on the "Talk to a doctor" video icon within the portal to get started. Before scheduling, be sure your illness or injury is included on the following list to ensure a healthcare provider can assist you virtually: Common cold and cough symptoms Muscular, tendon or joint pains not caused by injury Allergy or sinus symptoms Pink eye (no trauma or something in the eye) Urinary discomfort Diarrhea without vomiting Rashes or skin sores Backache Nail problems Screening examination for sexually transmitted illness (without symptoms) Medication refills (not controlled substances) When Should I Go to the Emergency Room? Urgent care and Virtual Visits are great options when experiencing minor illness or injury and it’s too urgent to see your primary care provider. Renown Emergency Rooms are designed to treat patients who need immediate attention for emergencies, such as: Burns Allergic reactions Broken bones Stitches Skin infections Heart attack Stroke Rashes Venomous stings and bites Asthma attacks Choking or poisoning Fainting, dizziness or confusion Head injuries Seizures Severe bleeding Difficulty breathing Severe headache Eye injuries Severe pain Renown Emergency Rooms are open 24 hours a day, 7 days a week, 365 days a year. For life-threatening emergencies, always call 9-1-1 immediately. We know there is nothing jolly about getting sick or injured during the holidays, but we hope you can find some comfort knowing that Renown Health is here with the care you need, when you need it most.
-
Smart Watch Notification Saves a Life
In sailing, when you encounter rough seas, you can’t change the wind pattern, but you can adjust your sails. The same rings true for life. We confront unpredictable circumstances daily, but how we react to them can make all the difference. For Renown patient and avid sailor Robert (Dan) Seifers, recent events make this mantra reign true. A Concerning Alert Monday, Aug. 22, started out just like any other day for Dan. He was on a walk with his dog, enjoying the sunshine, when suddenly he felt a wave of dizziness and a buzz on his wrist. His Apple Watch alerted him that his heart rate had dropped to dangerous levels. Returning home immediately, he notified his wife, Carol. Doing their best not to panic, the couple confirmed the reading with their at-home blood pressure machine. The watch was right – Dan’s heart rate was in the low 30s. After taking some time to see if Dan’s heart rate would return to normal, the couple decided it was time he sought medical help. Conveniently, Carol had a lab appointment scheduled next door to Dan’s primary care physician, Dr. Bonnie Ferrara. The couple headed out the door, not realizing what the rest of the day would bring. The Next 48 Hours Upon arrival at the office, Dan calmly approached the front desk to explain his situation. With no delay, staff members sprang into action, quickly showing Dan to a patient room and notifying Dr. Ferrara. Before he knew it, Dan was receiving an electrocardiogram (EKG). Following a review of the results, Dr. Ferrara returned to let Dan know he needed to get to the hospital immediately. The rest of the afternoon moved quickly for the couple. Dr. Ferrara had already notified the Renown Regional Medical Center Emergency Room staff, who were on standby for the couple’s arrival. “Gee, this must be serious,” thought Dan, who at the time was experiencing no other alarming symptoms other than the low heart rate indicated on his watch. Several doctors and nurses began their analysis, including a chest x-ray, blood test and additional EKG. Confirming Dr. Ferrara’s results, a Renown cardiologists, Dr. Christopher Rowan and Dr. Shining Sun, joined Dan’s care team. Within two hours of checking into the hospital, Dan was admitted, monitored overnight and prepped for surgery to receive a pacemaker the next day. Tracking Your Heart Health Following the purchase of their Apple Watch devices, Dan and Carol were unaware of these heart health features. Like many others, they were looking forward to the next best tech gadget that would help them stay connected with their friends and family. Now, the couple says they will use their experience to spread the word about the importance of ensuring these settings are enabled. According to Apple, you can turn on these notifications from the Heart Rate app on your Apple Watch (Series 1 or later) to alert you to high or low heart rates and irregular heart rhythms. If you receive a notification, an irregular rhythm suggestive of atrial fibrillation (A-Fib) or a low or high heart rate has been identified and confirmed with multiple readings. In Dan’s case, the signal from his watch was the result of a heart block, a condition where the electrical signal that controls your heartbeat is partially or completely blocked. Dizziness and low heart rate are common symptoms of a heart block. But this was not the first time the couple had experienced this type of alert from their watch. More than a year and half ago, Carol’s watch notified her of an irregular heart rhythm that was suggestive of A-Fib. She immediately made an appointment with Dr. Danish Atwal, the lead cardiologist at Renown’s Helaine Greenberg Women's Heart Center. Thanks to medication prescribed by Dr. Atwal, Carol now lives a healthy, active life while managing her A-Fib, continuing to wear her Apple Watch, which can also help track her A-Fib History. “I’ll share our story with anyone who will listen and encourage them to get a smart watch. I consider myself an unofficial spokesperson,” said Carol with a chuckle. A Thankful Heart The Senior Care Plus members could not be more amazed at the way Dan was treated by the staff at Renown. “I wish I could personally thank them all. I will highly recommend Renown to all I come in contact with,” said Dan with his Apple Watch still proudly strapped to his wrist. “I was closely monitored and treated like royalty.” Quick action to medical emergencies like Dan’s is just one of the many reasons why collaboration is part of our four key values at Renown. The open line of communication between our primary care facilities and hospitals helped Dan get the prompt care he needed, right when he needed it. A month post-op, Dan is doing well and back to enjoying the things he loves during his retirement, including playing the harmonica in the Grumpy Old Man Band, exploring the northern Nevada backroads in his jeep and working on his swing at the golf course. Dan can rest assured that while enjoying the winds of life, if his heart begins to beat too slowly again, the pacemaker will send a signal to correct the beat. “The prompt attention to my heart block undoubtedly saved my life,” said Dan in what he calls his 6-star review of Renown Health. “Thank you from the bottom of my heart, which is happily beating at 60 beats per minute.” This article is not sponsored by or affiliated with Apple, Inc. For more information on the Apple Watch and it's features, visit apple.com.
-
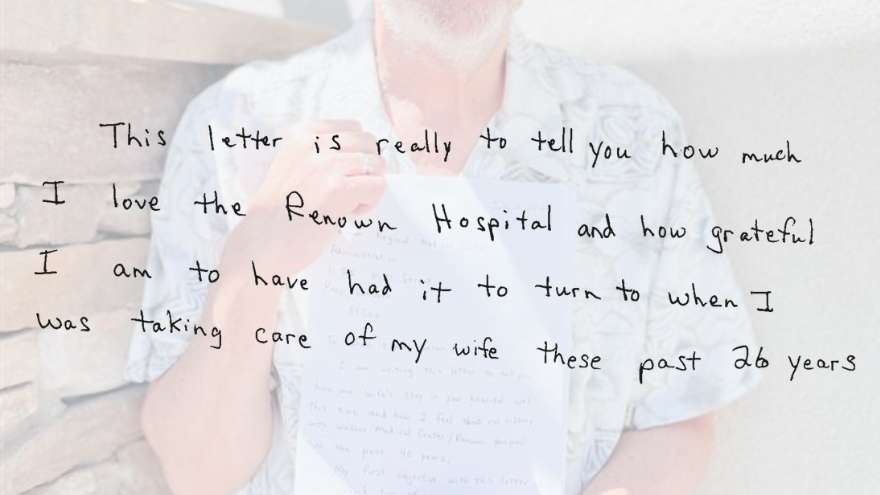
40 Years of Exceptional Care
“In sickness and in health” are words we often hear when celebrating the momentous occasion of marriage with our friends, families and loved ones. For James Breckenridge, these words were the foundation of the love and commitment he and his wife Carolyn showed to each other during their 30 years of marriage. In health, James and Carolyn shared a love of traveling. Hopping in their van, driving across the continental United States and enjoying the views along the way will be a memory James cherishes forever. Unfortunately, their excursions would be cut short when Carolyn fell ill, rerouting to their local hospital, Renown Health. Carolyn has spent more time at the hospital than the average person – including recovering from COVID-19 at Renown South Meadows Medical Center. However, hospital admittance for Carolyn meant the same for James, providing support to his wife during her stay. Following more than 40 years of exceptional experiences with Renown and their most recent discharge from the hospital, James wrote a letter recognizing the efforts of the team members and healthcare providers who not only cared for Carolyn but also James. To Whom It May Concern James began his letter by applauding two Renown Regional nurses they got to know well during their recent visit. Tiffany and Ashley went the extra mile to care for Carolyn attentively. From simple tasks like gathering requested supplies to answering James’ questions in detail, they helped provide a comfortable environment for the couple. To these nurses, these tasks may have felt like another day at work. Still, James’ letter commends them for their acts of service, reminding us that every interaction we have with a patient can be a memorable one. Tiffany and Ashley weren’t the only team members who received recognition in James’ testimonial. He also took a moment to recognize the various nurses, certified nursing assistants, therapists and doctors they encountered during their care journey. All provided the excellent and helpful experience we aim for at Renown. Healing Memories James first brought Carolyn to Renown Regional Medical Center, formerly known as Washoe Medical Center, in 1980, but it was 1996 when things changed for him. Carolyn was admitted to the hospital for a procedure they originally anticipated would come with a difficult prognosis. To their surprise, doctors found the opposite. It was in that joyous moment that James’ perspective of hospitals shifted, now viewing them for what they truly are – a place people go to get better. “Every time I walk around Renown Hospital, I remember all the times Carolyn was healed there,” James wrote in the latter half of his letter. Healing Isn't Just for the Patient James took advantage of the many support resources accessible to family members during their time at Renown. These donor-funded hospital initiatives are a valuable mental health resource in difficult circumstances. Whether it was an afternoon stroll with his wife through Fianna’s Healing Garden or quiet time alone in the Spiritual Center, James never hesitated to turn to these resources in his time of need. “Although I know the Tahoe Tower is the modern, state-of-the-art part of Renown, I prefer the Sierra Tower because that is where most of my memories are.” Even a simple daily walk to the on-campus Starbucks was a notable part of his day – grabbing a cup of coffee for himself and often a treat for Carolyn. An Inspiration in Healthcare When asked to describe Renown in one word, James chose “inspirational.” His collective experiences with Renown, James said, “helped him to be a better healthcare advocate” when his wife received care at other hospitals. As a healthcare leader, we challenge ourselves to go above and beyond for the health of our entire community. Collaborating with our patients and their families is at the center of everything we do at Renown. Positive reviews mean the absolute world to us, and something about this handwritten letter feels even more special. We could not be more appreciative to James for sharing how our vision to inspire better health in our community was reflected in his 40 years of experience with Renown. We were saddened to hear of Carolyn’s passing during a recent meeting to thank James for his letter. We take solace hearing James’ beautiful memories of his wife and knowing that Renown Health was there in times of sickness and health. We offer our sincere condolences to James, Carolyn’s children and their family members.