Search
-
Prevent Osteoporosis: Take Control of Your Bone Health Today
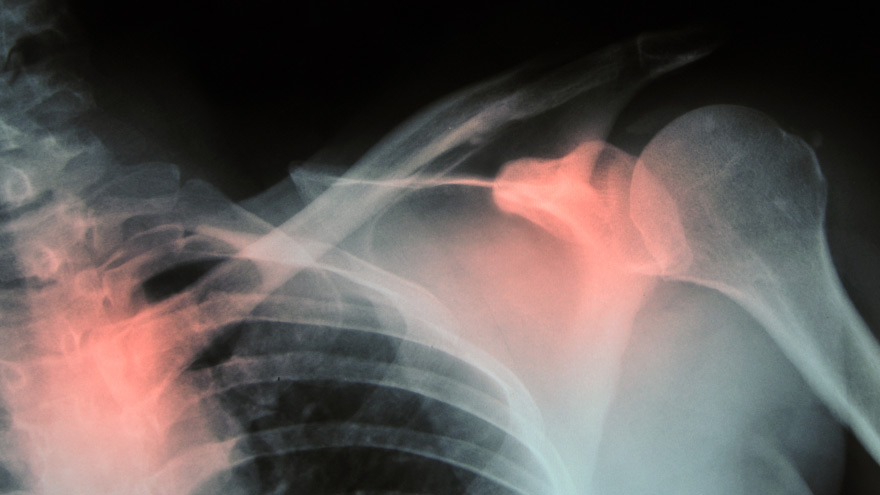
Some risk factors associated with osteoporosis are out of your control. But you’re in luck, because some can be lessened by following simple tips. Below, Orthopedic Nursing Manager Katie McCarthy discusses the signs, symptoms and preventive measures. By Katie McCarthy, BSN, RN, ONC, Orthopedic Nursing Manager, Renown Health Osteoporosis is often called the silent disease, because it develops gradually for years with no clear signs or symptoms. And while some bone loss is expected as we age, osteoporosis is not a normal part of aging. So it’s important to start thinking about your bone health early. Bone is not just a lifeless scaffold for the body. It is living tissue that regenerates continually. Once we reach peak bone mass around age 25, we begin losing more bone than we produce, increasing the risk of developing osteoporosis — which literally means porous bone and points to a loss in bone density. In severe cases, normal everyday activities or movements, like hugging, can cause a fracture. After the first fracture you’re at higher risk for more, which can lead to a life of chronic pain and immobility. Bone fractures in the spine or hip are the most serious. Hip fractures can result in disability and even death — especially in older adults. Spinal fractures can even occur without falling. The vertebrae weaken to the point that they simply crumple, which can result in back pain, lost height and a hunched-forward posture. Osteoporosis: Uncontrollable Risk Factors Women are at greater risk of developing osteoporosis than men, and white and Asian women are at higher risk than black and Hispanic women. Other uncontrollable risk factors include: age; a family history of osteoporosis; certain genetic conditions; medications and medical treatments; eating disorders; a low body weight and small, thin frame; ethnicity; menopause: In fact, the lack of estrogen produced during menopause is largely responsible for a woman’s increased risk. Poor diet, tobacco use, excessive alcohol consumption, lack of exercise and an unhealthy weight also contribute to bone loss. Fortunately, those risk factors are in your control. Without symptoms, you can’t know if you’ve developed osteoporosis unless you get a bone density test or suffer a fracture. If you fall into a high-risk group, are over age 50 or have any concerns about your bone health, consult your doctor and find out if you need to be evaluated. Additionally, if either of your parents sustained hip fractures, you experienced early menopause or took corticosteroids for several months — a steroid often prescribed to relieve inflammation and arthritis — you’ll want to talk to your doctor about your bone health. If you test positive, your doctor will devise a treatment plan to match your needs, which will include lifestyle changes surrounding diet and exercise to build and strengthen weak bones. Medication to slow bone breakdown and build new bone may be prescribed, depending on the severity of your bone loss. If you’ve sustained a spinal fracture that is causing severe pain, deformity or is not responding to non-surgical treatment, your doctor may recommend surgery. Reduce Your Risk of Osteoporosis You can strengthen your bones now to prevent osteoporosis from starting. Here are some tips: Eat a diet rich in fruits and vegetables and low in caffeine, sodium and protein. Avoid soda, and talk to your doctor to make sure you’re getting enough calcium and vitamin D. Don’t smoke — it directly correlates with a decrease in bone mass. Smokers also take longer to heal from a fracture. Limit alcohol to two to three beverages per day. It interferes with the production of vitamins needed to absorb calcium and the hormones that help protect bones. Exercise three to four times each week — it’s key to healthy bones. Weight-bearing exercises like jogging, hiking and especially weight lifting build bone mass and density. There are aspects of the aging process we can’t control, but we can do something about bone loss and osteoporosis. Find out your risk, and show your bones a little TLC — you’re going to need them. This story was also published in the Reno Gazette-Journal’s Health Source on April 24, 2016.
Read More About Prevent Osteoporosis: Take Control of Your Bone Health Today
-
A True Joint Effort: Exercises to Prevent Knee Pain
Experiencing knee pain during exercise or while undertaking daily activities? The knee is the largest joint in our body, so it goes without saying a lot hinges on its functionality. Here are a few exercises to help. Is exercise a real pain in the knee for you? Does getting up in the morning require a few minutes for your knees to adjust to walking around? As it turns out, knee pain is common, and it can result from injury, overuse or the breakdown of cartilage over time. Often, this pain is a result of faulty mechanics in your body, according to Jessica Ryder, a physical therapist with Renown Physical Therapy and Rehab. “We see weakness at the hips causing a lot of stresses at the knee,” she says. Exercises that Alleviate Knee Pain Try these three exercise to strengthen your glute muscles and maintain proper alignment in your knees. Hip Lift Lie flat on your back with your knees bent and feet flat against the floor. Lift your hips into the air until your body is in a neutral position, then lower your hips back down. Repeat this motion several times until you feel a gentle burn in your glute muscles. Step Down Stand with one foot on a stair or step. Slowly bend your knee and drop the other foot toward the floor. Slowly extend back up to your starting position. While doing this exercise, it’s important to move slowly, maintain control and ensure that your knee is in line with your toes. Do as many reps as needed until you feel a small fatigue in your muscles. Repeat this exercise on the opposite leg. Side Step with Exercise Band Place an exercise band around your ankles. Stand in a slight squat and then take several steps to the side until you feel a small fatigue on the outside of your hips. While doing this exercise, keep your upper body still and focus the exercise to your hips. The band will try to move your knees toward each other Repeat in both directions. Hometown Health and Renown Health are proud to be the official insurance plan and healthcare partners of the Nevada Wolf Pack. Renown Physical Therapy and Rehab | 775-982-5001 Through outpatient physical, occupational and also speech therapy, Renown Physical Therapy and Rehab gives patients hands-on, individualized treatment. Our therapists use evidence-based methods to help patients return to an active, productive lifestyle. Learn More About PT
Read More About A True Joint Effort: Exercises to Prevent Knee Pain
-
Learn How to Spot Asthma in Children and How It Is Treated
Sometimes, children’s asthma masks itself in symptoms that can be similar to other common respiratory problems. Dr. Shipra Singh of Renown Medical Group – Pediatrics discusses some diagnoses and treatments for asthma in children. Adults can easily recognize when we are out of breath or struggling to breathe, but what if you noticed this regularly happening to your infant or child during their daily play? Would you think they might have asthma? It may be difficult to tell if your small child has asthma because the symptoms can be similar to other common respiratory problems (bronchitis, croup, pneumonia) or even allergies. Read on to learn how to spot and manage asthma in your infant or child with advice from Shipra Singh, M.D., MPH, Pediatric Pulmonologist at Renown Medical Group – Pediatrics. According to the Centers for Disease Control, asthma in children is a leading chronic illness and cause of school absenteeism in the U.S. Asthma is a multi-factorial disease. Smoking during pregnancy or a family history of allergies or asthma has been linked to a greater chance of developing childhood asthma. Asthma is usually on a spectrum and not a single disease. It can range from mild to severe. Because an infant’s or toddler’s airway is smaller than in older children and adults, even a slight blockage caused by mucus or a restricted airway due to swelling can make breathing hard for them. In children five and younger, one of the most common causes of asthma symptoms is a respiratory virus, which narrows the airways in the lungs. These include a cold, the flu, bronchitis, pneumonia and other illnesses. How can I tell if my child has asthma? Unfortunately small children are unable to describe their symptoms, making asthma difficult to diagnose. Your child may even be active, playing and smiling, although they are experiencing chest tightness or labored breathing. Observe your child and let the child’s doctor know if: Your child’s breathing behavior has changed (coughing, wheezing, rapid breathing) Your child’s breathing pattern changes (day vs. night, with rest or activity, inside vs. outside) You have a family history of asthma or allergies Your child’s breathing is triggered by any foods or allergies With your help, your child’s doctor can make the best diagnosis to determine if your child has asthma. A pediatric pulmonologist (lung specialist) or pediatric allergist may also have to be consulted for special testing. Tests may include lung function testing, allergy tests, blood tests and X-rays for an accurate diagnosis. What is the treatment for infants and toddlers? Young children can use many of the same medications as older children and adults, although the way they take them and the dosage will differ. A nebulizer (or breathing machine) creating a medicated mist for your child to breathe through a mask may be used. An inhaler with a small spacer tube connected to a mask is also common to help your child breath medication into their lungs. Either of these options are effective. Asthma in children is treated with both fast-acting and long-term medicines to open up airways quickly for easy breathing and also to lessen asthma symptoms over time. Communicate with your child’s medical providers to create a personalized asthma management plan for them. How can I manage my child’s asthma? Recognize your child’s breathing habits and be aware of worsening symptoms. Consult with your child’s doctor on a daily asthma action plan to recognize worsening symptoms and track medications. (Here’s an example of an asthma action plan provided by the U.S. Department of Health and Human Services’ National Institutes of Health). Be consistent with the plan and talk to your doctor before changing it. Have an emergency plan in case of a serious asthma attack. Know where the closest ER is and know who can take care of your other children. Also know what the medical treatment coverage is under your insurance plan. We asked Dr. Singh about asthma in children: “Discussing asthma with your child may be a difficult subject. Some kids find the subject frightening or confusing. Others, especially the older kids, may be resentful of the treatment and may not be interested in doing the treatment. Talk to your doctor about advice to build an open and trusting relationship regarding your child’s asthma care.” What can I do to reduce my child’s asthma? Know your child’s asthma triggers (dust, pets, pollen, etc.) Follow your asthma action plan Keep your child away from smoke Can my child outgrow their asthma? Asthma symptoms change day to day and year to year. An older child can better recognize and manage their symptoms, so asthma episodes may lessen. However asthma is a life-long condition of the airways, so it is important to always have an asthma action plan, even with occasional asthma events. Renown Health Pediatric Care | Same-Day Appointments: 775-982-KIDS Our team of pediatricians, specialists and nurse practitioners have specialized training in children’s healthcare needs. We see children from birth to age 18 for the following pediatric needs: Wellness and preventive visits Sick visits Immunizations Behavioral health Allergy Asthma Common cold Diabetes Asthma resources for parents: Asthma and Allergy Foundation of America Centers for Disease Control and Prevention
Read More About Learn How to Spot Asthma in Children and How It Is Treated
-
Virtual Visits – Healthcare You Need At Home
Virtual visits are basically secure, video conferencing visits with your health provider. Of course if you are sick, you want to avoid going outside of your house. With Renown Health’s virtual visit program, you can now see a provider from the comfort of your own home. As we work to keep all of our patients home and healthy, we’re here for any ongoing healthcare needs you have. There are two easy ways to access a virtual visit with Renown Health. If you need an urgent care visit, you can get in line using your MyChart account You can make a virtual visit with some Renown Health providers you see currently Virtual Urgent Care from a Renown Provider By using MyChart, you can now login and request to “Talk to a Doctor.” After filling in some information and confirming your healthcare concern, you will be put into a virtual line. The healthcare team will notify you by text or email when a provider is ready to talk to you virtually. Virtual urgent care visits are available for all ages. Get To Know MyChart Virtual urgent care visits are available for all ages, and can address: Common cold and cough symptoms Muscular, tendon or joint pains not caused by injury Allergy or sinus symptoms Pink eye Urinary discomfort Diarrhea without vomiting Rashes or skin sores Backache Nail problems Screening examination for sexually transmitted illness (without symptoms) Medication refills (not controlled substances) Symptoms for In-Person Urgent Care Visits Shortness of breath Chest pain Abdominal pain Numbness or weakness of any location that is new Traumatic injuries (including eye injuries or something in the eye) Severe pain of any other body location Dizziness or confusion Bleeding from any location High fever (greater than 102 degrees for all ages) Persistent vomiting Loss of vision Ear pain Substance abuse or psychiatric problems Virtual visits are open 9 a.m. through 6 p.m. Monday-Friday and 10 a.m. to 4 p.m. Saturday and Sunday for Nevada residents. Renown Provider Virtual Visits Many primary and specialty care appointments for adults and children are now available virtually. If you have a provider with Renown Medical Group, call 775-982-5000 to see if you can have a virtual appointment from the comfort of your home. MyChart Assistance If you need assistance with your MyChart account, please call 775-982-6686. For all other questions about scheduling and appointments, please call 775-982-5000.
Read More About Virtual Visits – Healthcare You Need At Home
-
Stay Inside When Skies Are Smoky
Even when fires burn outside our area, the air quality in the region can reach dangerous levels. Our expert explains how to maintain your lung health when fire season strikes. It’s a sight we know all too well as northern Nevadans — a hazy or thick layer on the horizon when smoke rolls in from nearby fires. Sometimes the smoke is more evident than others, but it’s important to remember, even when the smoke may not be as visible across the valley, it still impacts our air quality. The last week or so, our air quality has been in the “unhealthy for sensitive groups” range, which can be dangerous for people who are sensitive to air pollution. Air Quality Changes: Who’s at Risk? Renown Pediatric Pulmonologist Sonia Budhecha, M.D., explains certain people are especially at risk when smoke moves in: Older people, whose lungs are not as healthy as they used to be Young children, whose lungs are still developing People with heart and lung disease including asthma, COPD and emphysema “Smoke and haze from fires carry particulates that can get into your respiratory system and eyes, which can be a danger for all ages,” Dr. Budhecha says. How You Can Protect Yourself Until the smoke clears and the air returns to the “good” range, it is best to follow these tips to protect yourself and your family: Stay indoors and keep windows closed Turn on the air conditioning to recirculate clean air Drink plenty of fluids to help your body flush out any toxins you inhale Additionally, all community members should reduce their physical activity and try to prevent heavy exertion outside. If you or a loved one has a heart or lung disease, avoid physical exertion altogether because smoke can aggravate these conditions. “People with heart disease may experience shortness of breath, chest pain, palpitations or fatigue,” Dr. Budhecha says. “People with lung disease may also have shortness of breath, chest discomfort, wheezing, phlegm or a cough.” Smoky Signs and Symptoms Smoke can also impact healthy people — irritating your eyes, nose or throat. And in some cases, inhaling smoke can lead to bronchitis. When haze moves into our area, keep an eye out for these symptoms: Burning or stinging eyes Runny nose Cough or scratchy throat Headaches Wheezing Shortness of breath Difficult taking a full breath Chest heaviness Lightheadedness Dizziness If experiencing any of the above symptoms, seek medical attention or call your doctor for advice. Sometimes, these symptoms do not appear for as long as 24 to 48 hours after smoke inhalation. For those that have pre-existing lung or heart conditions, consult with a health care provider on action or management plans. To schedule an appointment Visit Renown Pulmonary Medicine, or call 775-982-5000. Understanding Our Air Quality The Air Quality Index (AQI) is broken down by large (PM10) and small (PM2.5) particulates. According to Dr. Budhecha, large particulates are usually ones that can be seen and smelled. They can damage your eyes and nose but don’t often get deep in the lungs or blood vessels. “The more dangerous ones are PM2.5, which can’t always be seen or smelled,” Dr. Budhecha says. “Any time the AQI is above 51, children with lung or heart disease should not be outdoors.” For the latest air quality update in your area, visit AirNow.gov or call (775) 785-4110.
-
What You Need To Know About Cold Water Drowning
Northern Nevada is home to some of the most gorgeous and pristine lakes in the country — but also some of the most unforgiving. Lake Tahoe water temperatures average 50 degrees in the summer, making the danger of hypothermia real and always present. Here are the signs, symptoms and ways to prevent cold water drowning. When we think of air temperature at 50 degrees Fahrenheit, it’s not all that cold. But when it comes to water that’s 50 degrees, there is no comparison. Immersion in cold water is life threatening and can happen within a minute. Taking the right precautions before entering the water can save your life. The 4 Phases of Cold Water Drowning 1. Cold Shock Response: This response affects breathing and happens within the first minute. An automatic gasp reflex occurs in response to rapid skin cooling. If the head goes below water, water may be breathed into the lungs, resulting in drowning. A life jacket will help keep your head above water during this critical phase. Additionally, hyperventilation, like the gasp reflex, is a response to the cold and will subside. Panic will make this worse, so the key is to control breathing. 2. Cold Incapacitation: This response occurs within the first five to 15 minutes in cold water. In order to preserve core heat, vasoconstriction takes place decreasing blood flow to the extremities to protect the vital organs. The result is a loss of movement to hands, feet, arms and legs. Unless a life jacket is being worn, the ability to stay afloat is next to impossible. 3. Hypothermia: Important to note, it can take 30 minutes or more for most adults to become hypothermic. So there’s time to take action and survive. Keeping panic at bay is critical, as you have more survival time than you think. Symptoms include: Shivering Slow and shallow breathing Confusion Drowsiness or exhaustion Slurred speech Loss of coordination Weak pulse 4. Circum-rescue Collapse: This experience can happen just before rescue and is not well understood. Symptoms range anywhere from fainting to death. Some experts believe an abrupt drop in blood pressure may cause this final stage of cold water drowning, post-rescue. Additional Cold Water Drowning Safety Tips and Helpful Resources Always wear a personal flotation device as well as a wetsuit or drysuit. Your personal flotation device is the most important piece of water safety gear. Try not to panic as the first phases will subside. Controlled breathing is to staying calm. Research suggests the body can withstand the cold longer than we think. The Heat Escape Lessening Posture (HELP) is a position which helps conserve energy if you’re wearing a personal flotation device. By hugging your knees to your chest, this posture helps maintain body heat for some time.
Read More About What You Need To Know About Cold Water Drowning
-
Tips for Coping with Smoke-Related Health Problems
Millions of people across the west live in areas where air pollution can cause serious health problems. In addition, local air quality can affect our daily lives. Who is Affected? Kouros Farro, MD, a physician with Renown Urgent Care, advises that certain people are more likely to be affected when fine particle pollution reaches an unhealthy level. People who have asthma or other breathing conditions like chronic obstructive pulmonary disease (COPD). People who have heart disease or high blood pressure. Children and older adults. People of all ages who are doing extended or heavy physical activity like playing sports or working outdoors. “Everyone should take precautions when the air quality is unhealthy. Air pollution can aggravate heart and cardiovascular disease as well as lung diseases like asthma and COPD. When the air quality is unhealthy, people with these conditions may experience symptoms like chest pain, shortness of breath, wheezing, coughing, or fatigue. If you are experiencing any of these symptoms, use your inhalers as directed and contact your health care provider,” says Dr. Farro, who is board certified in family medicine and practices at Renown Urgent Care at 975 Ryland St. in Reno. “If you do not have a health care provider, there is a Renown Urgent Care office on almost every corner, with providers ready to see you.” Dr. Farro advises the following: Take it easy and listen to your body. Limit, change or postpone your physical activity level. If possible, stay away from local sources of air pollution like busy roads and wood fires. If you have asthma or other breathing conditions like COPD, make sure you have your relief/rescue inhaler with you. People with asthma should review and follow the direction in their written asthma action plan. Make an appointment to see your health provider to be sure you have an asthma action plan. Getting Same-Day Care Renown Urgent Care provides same-day treatment for a wide range of minor injuries, illnesses and medical concerns that are urgent but not life-threatening. Avoid the long wait times and high emergency room prices at 11 convenient sites, including Reno, Sparks, Carson City, USA Parkway, Fallon and Fernley. You can walk in or book ahead online. Make an Urgent Care Appointment Community Health Resources The Washoe County Health District offers online health information on its Smoke Smart website, including fire information, daily air quality information, fire and smoke maps and how to protect yourself. In addition, an online subscription page allows you to sign up for EnviroFlash, notifying you about air quality.
Read More About Tips for Coping with Smoke-Related Health Problems
-
Bone Fractures in Children Honest Expert Advice
Michael Elliott, MD, head of the Department of Pediatric Orthopedics and Scoliosis, answers some common questions about bone fractures. Is there a difference between broken bones and fractures? No, these are two different names for the same injury. Of course the common term is a broken bone. Using either name will describe your concerns. Medical personnel typically describe a broken bone as a fracture to a specific bone. For example, a broken wrist is also a fractured distal radius. To clarify, this describes the injured bone and the precise location. How do I know if my child has broken their bone? Many times children will fall and complain of their arm or leg hurting. In most cases the pain goes away and the child will return to their activities. When there is a deformity to the limb (curve in arm) and the child is complaining of pain, it is probably a fracture. If the arm or leg looks straight, look to see if there is any swelling or bruising. Both are signs of a possible fracture. Finally, if the limb looks normal but the child continues to complain, gently push on the bone. Likewise if it causes the same pain, then they likely have a fracture and should have an x-ray. My child fractured their growth plate, what does this mean? Growth comes from this area of the bone. In detail, these are located all over the body but typically at the end of the bones. With this in mind, fractures to these areas can result in the bone growing abnormally. Because of potential shortening of the arm or leg, or bones growing crooked, it is important to follow fractures closely (up to 1-2 years or longer). It is better to identify a problem early. Small problems can be treated with small surgeries. What if the bones of the x-ray do not line up? Because children are growing, unlike adults, their bones will remodel and straighten with growth. The amount of remodeling occurring depends on a child’s age, the bone fractured and the location. In many cases an angled bone will grow straight over the course of a year. For this reason, someone with experience in caring for children needs to follow bone growth. How long does it take fractures to heal? Factors deciding when a cast can come off include: Child’s age. Bone fractured. Fracture location. Young children heal faster than teens, teens heal faster than young adults, who heal faster than older adults. In young children most fractures heal in 4-6 weeks. However, teens generally take 6 weeks to heal, and adults can take much longer. Although your child is out of their cast, it may not be healed completely to return to all activities. Placing a splint is during this time is common. This typically gives them added protection for several weeks after their cast is removed - in case they forget their limitations. What if my child is still limping? Whether a child is in a walking or non-weight bearing cast, removing it often leaves them stiff and sore. Therefore many children will walk as though they still have a cast in place. In most cases this resolves in about three weeks. Regardless, if your child is still limping or walking abnormally after three weeks, contact the treating doctor. They may benefit from physical therapy or a repeat evaluation. (This article was original published in the July 2019 issue of South Reno Kids & Sports.)
Read More About Bone Fractures in Children Honest Expert Advice
-
Take Charge of Your Sexual Health
Much like general physical and mental health, sexual health is an essential aspect of your overall well-being. Therefore, educating yourself on your sexual health is an important piece regarding your overall wellness. Secure & Private Virtual Visits Did you know that many sexually transmitted disease appointments can happen virtually, in the privacy of your own home? Our providers can perform a screening examination for sexually transmitted illness (without symptoms) when it’s convenient for you. This is a great option if the topic makes you uncomfortable during an in-person visit, or if you can’t find time to visit your primary care provider or local urgent care. After the telehealth appointment, your provider will determine the next steps for you. Remember, in-person visits are always an option as well. Here’s how you can take charge of your sexual health: Get Comfortable with Getting Tested Surprisingly, some people with STDs don't show symptoms, meaning they may not even know they have an STD unless they get tested. Even if an STD shows no symptoms, the result of non-treatment can be serious. Bret Michael Bellard, MD, with Renown Medical Group, shares that it’s important for people to get tested for STDs because if left untreated, they can cause the following health problems: Loss of fertility Pregnancy complications Other health issues When to Visit Your Primary Care Provider Who should get tested and how often? “The recommendations are that everyone from ages 13 to 64 should get tested at least once for HIV. All sexually active adults should also be tested for other STDs once a year, and all pregnant women should be tested at the start of their pregnancy,” says Dr. Bellard. Some STDs, like syphilis, can be passed from mother to baby, so it's important for women to get tested as soon as they know they’re pregnant. Dr. Bellard recommends going to your primary care provider for testing. “They can also give advice on prevention and other health topics.” If you don’t have a primary care provider, this is a great reason to get established with one. Women with an established OB/GYN can have STD testing done simultaneously with their annual pelvic exam. The providers in Renown's network care for patients of all ages and specialize in family medicine, internal medicine, pediatrics and OB/GYN. Practice Safe Sex STDs are preventable. Practicing safe sex and getting tested routinely are your best defenses against all types of STDs. For many, the conversation about sexually transmitted diseases is awkward and many avoid it. To lower your risk of contracting an STD, don’t wait until you’re “in the moment” to have the conversation with your partner about the last time you were both last tested. If you haven’t gotten tested in-between new partners, use latex condoms every time you have sex until you are both confirmed negative of STDs. Condoms are not 100% effective at preventing disease or pregnancy. However, they are extremely effective if used properly. To establish Primary Care, visit renown.org/virtualvisits or call 775-982-5000
-
What is Dry Drowning?
Whether you're a parent, grandparent, caregiver or sibling, you should know drowning is the second leading cause of death among children. Yet, while we are vigilant about protecting children from water accidents and drowning, a condition known as dry drowning or delayed drowning can go unnoticed. In fact, most people aren't even aware it exists. Dry drowning defined Dry drowning is a side-effect of a near-drowning experience and includes spasms of the vocal cords and larynx — known as a laryngospasm. This occurs when the body attempts to shut down the passage of any liquid into the lungs. Unfortunately, it can also shut down the passage of air into the lungs and force fluid into the stomach and lungs. Often the condition is not discovered until it's too late — severe cases can cause death within one to 24 hours after a water incident occurs. Who is susceptible? Novice or first-time swimmers are at increased risk, as are children with asthma and known breathing issues. In addition, children who have had pneumonia or experienced acute respiratory distress syndrome are also at greater risk. To reduce these factors, caregivers should be exceptionally watchful of inexperienced swimmers. According to Leland Sullivan, MD, of Northern Nevada Emergency Physicians, children under the age of 5 are most susceptible to drowning and often drown in residential swimming pools. Infants less than 1-year-old most often drown in bathtubs. What are the signs of a dry drowning episode? If your child has a near-drowning incident, a few moments of coughing until they calm down is normal. However, you should know the more severe signs and symptoms to watch for during the 24 hours following the incident, including: Persistent coughing Difficulty breathing and/or shortness of breath Chest pains Extreme fatigue and/or lethargy Change in typical behavior Face becomes pale What is the treatment and prognosis for dry drowning? Dr. Sullivan recommends that all victims of near-drowning incidents seek medical attention, even if they have no symptoms. If caught early, dry drowning can be treated. If you think your child is experiencing a dry drowning episode, go to the nearest emergency room as quickly as possible — do not attempt treatment at home. Healthcare professionals will work to supply oxygen to your child's lungs to restore and regulate breathing.
-
10 Things You Might Not Know About Urgent Care
Visiting a Renown Urgent Care location is an excellent option when you have a non-severe condition, such as a skin rash or sore throat, can't get in to see your primary care provider in a timely manner or if you need an appointment after regular business hours. To learn more about the ins and outs of Urgent Care, we spoke to David Lemak, MD, Division Chief Urgent Care, who let us know some reasons to visit Urgent Care, how to make your visit as efficient as possible, and more. Remember, for a life-threatening emergency, call 911 immediately! Urgent Care is similar to a Primary Care provider Urgent Care providers can do most of the things your Primary Care provider can do, with visits billed the same as an office visit. If you could put the word “severe” in front of your reason for visiting Urgent Care, please go to the emergency department right away For a list of what is an appropriate visit for Urgent Care click here. Also, we recommend that babies 2 months old and younger should go to the Renown Children’s Emergency Department, not Urgent Care. Renown Health has 10 Urgent Care locations across northern Nevada There are five locations in Reno, two in Sparks, one in Carson City, one in Fernley and one in Fallon. For a complete list of Renown Urgent Care locations, click here. Many of your Urgent Care needs can be accomplished via a virtual visit, from the comfort of your home or office Conditions Appropriate for a Virtual Visit Included: - Common cold and cough symptoms - Muscular, tendon or joint pain not cause by injury - Allergy or sinus symptoms - Pink eye - Urinary discomfort - Backache - Sexually transmitted illness screening - Rashes or skin sores - Medication refills (no controlled substances) Some conditions are not appropriate for a virtual visit. They include: - Chest or abdominal pain - Shortness of breath - Traumatic injuries - Dizziness or confusion - Bleeding - High fever - Persistent vomiting - Loss of vision - Substance abuse or psychiatric problems Book ahead for shorter wait times, but remember walk-ins are always available. Click here to make your appointment. This booking page conveniently shows the next available appointment at each location. Typically, mornings and late afternoon (right before dinner time) have the shortest wait times if you plan on walking in. You will be asked to wait in your car when you arrive at a Renown Urgent Care facility. While you wait (or even before you arrive), patients are encouraged to complete all registration paperwork and co-pay information online. Urgent Care is great for visits such as back-to-school physicals, camp physicals, commercial motor vehicle exams and more. Sometimes you cannot get in to see your primary care provider to meet the last-minute deadlines for certain school or work-related physicals. Many of these appointments can be completed at Urgent Care; we just recommend you call ahead and confirm that our facility offers what you need. An Urgent Care provider can virtually order a PCR COVID-19 test. Whether you have a possible exposure, are not feeling quite like yourself or need a negative test for upcoming travel, a COVID-19 test can be ordered for you. The cost for a visit to Urgent Care is dependent on your benefits, but the visit is billed the same as a standard office visit. If you don’t have insurance, a basic visit to a Renown Urgent Care will cost $125.
Read More About 10 Things You Might Not Know About Urgent Care
-
Pulmonary and Sleep Medicine
Pulmonary Medicine Our expert pulmonary medicine team diagnoses and cares for patients with lung and breathing challenges. Serious breathing problems and long-term conditions, such as COPD and emphysema, are treated by our extensively trained providers. Our board-certified care team has the experience and clinical judgment to ensure the strongest possible patient outcomes. If you have a chronic lung condition diagnosis, you may also benefit from Renown Pulmonary Rehab. Conditions We Treat Asthma Bronchitis (acute and chronic) Chest infections Chronic obstructive pulmonary disease (COPD) Cystic fibrosis Emphysema Lung cancer Lung transplant Pulmonary fibrosis Pulmonary hypertension Pulmonary tuberculosis (TB) Other chronic lung diseases Pulmonary Services