Search
-
The Not-So-Fab-Five: Foods That Increase Stroke and Heart Disease Risk
Did you know that 80 percent of all strokes are preventable? Learn which foods should be eaten in moderation to reduce your family's risk of stroke. Stroke is the fifth leading cause of death in the nation and a major cause for disability, killing 130,000 people each year. But did you know that 80 percent of all strokes are preventable, according to the American Stroke Association? Several stroke risk factors -- high blood pressure, smoking, diabetes, physical activity level, obesity, high cholesterol and heart and artery disease -- can be controlled, treated and improved, right down to the foods we choose to consume each day. Diets high in sodium can increase blood pressure, putting you at greater risk for stroke. A high-calorie diet can lead to obesity -- another risk factor. And foods high in saturated fats, trans fat and cholesterol will raise your blood cholesterol levels causing blood clots, which -- you guessed it -- can lead to a stroke. The “not-so-fab” five foods listed below play a large role in damaging your body and causing vascular disease, stroke and heart disease and should be avoided on a regular basis. However: Moderation is the key to life, in my opinion. Sure, everyone is going to have a soda here and there or a steak off the grill, but keep it off the main menu. 1. Packaged and Fried Food Have you noticed foods like hot dog buns and bottled salad dressings rarely go bad? Ever asked yourself why? This is due to the use of hydrogenated oils, which are trans fats. Hydrogenated oils stay solid at room temperature and do not require refrigeration. Convenient? Yes. Healthy? No. Unfortunately, many frozen foods and meals also fall into this category, except for frozen fruits and veggies. So here’s the lowdown on trans fats: They’re considered by many experts as the worst type of fat you can consume, raising your LDL (“bad”) cholesterol and lowering your HDL (“good”) cholesterol. While some meat and dairy products contain small amounts of naturally occurring trans fat, most dietary sources are formed through an industrial process adding hydrogen to vegetable oil, causing the oil to solidify at room temperature. The FDA is in the process of restricting or possibly banning trans-fats from food in the U.S. A study published in JAMA Cardiology compared data from counties with and without trans-fat restrictions and the findings were substantial: There was a 6 percent decline in hospitalizations for heart attack and stroke in counties with trans-fat restrictions. Bottom line: Ideally no processed food should pass your lips, but realistically, aim for less than 2 grams of trans fat per day. Skip the store-bought treats at the office and fries at lunch. Also avoid crackers, regardless of what you are dipping them in. Choose to eat fruits to satisfy your sweet cravings and veggies and hummus to satisfy the savory. 2. Lunch meat Processed meats, including bacon, smoked meats and hot dogs, are all on the DNE (Do Not Eat) list, unless you want to play with fire. Processed meats are a no-go if you want to keep your arteries clear of plaque buildup. So what is the alternative to your salami sandwich? Try a healthy alternative like a tuna sandwich with avocado (a great alternative to mayo) or a veggie sandwich. 3. Diet soft drinks First of all, when a drink is sweeter than a candy bar but it contains zero sugar and zero calories, buyer beware. Many consumers think because a soda is labeled “diet” it’s a better choice, but studies have linked diet soft drink consumption with an increased risk of stroke and vascular disease. In a nine-year study of more than 2,500 people, those who drank diet soda daily were 48 percent more likely to have a heart attack or stroke or die from those events, compared with those who rarely or never drank soda. What else are you supposed to drink? If you must drink soda, break the everyday habit and drink it on special occasions; otherwise water rules. And if you don’t like water, try flavoring your water with fruit slices. 4. Good-old red meat So is there ANY good meat out there you ask? The answer is yes, but it’s not red. In the journal Stroke, an article showed women who consumed large servings of red meat regularly had a 42 percent higher incidence of stroke. Red meat is high in saturated fat, which clogs arteries with plaque. The alternative to red meat is a heart-healthy protein like poultry or fish, or even non-animal products like beans, nuts and tofu. 5. Canned foods Steer clear of factory processed soups, beans and sauces. Canned items all have incredible amounts of sodium or MSG or baking soda/powder to maintain their freshness and shelf life. One study showed if you consume more than 4,000 mg of salt per day, you more than double the risk of stroke compared to diets with less than 2,000 mg. Another tip: When possible, plan and make meals from scratch. Making the wrong meal or snack choices is one of the biggest contributing risk factors for stroke and heart disease. Most people know what good food choices are, but they don’t realize the serious impact the bad choices have on overall health. Learn what is most beneficial to your body to consume. It will be a life changer – literally.
Read More About The Not-So-Fab-Five: Foods That Increase Stroke and Heart Disease Risk
-
Make Your Own Trail Mix: 4 Quick and Easy Recipes
Craving a snack with crunch, sweet flavor and a powerful nutritious punch? These healthy, homemade variants of this make-it-and-take-it super snack are sure to satisfy your sweet tooth and your healthy lifestyle. Who says healthy snacks and bland taste go together? We say you can have it all — nutritious and delicious snack foods that taste great and satisfy — and trail mix fits the bill. Your homemade batch can be as healthy as you like. The nuts provide fiber, protein and a whole lot of crunchy goodness; dried fruit and touches of chocolate infuse the mix with just the right amount of sweetness. We’ve compiled some simple-to-make and hard-to-resist recipes so you can easily pick up a few items from the grocery store’s bulk bins, or your kitchen cupboard, and put together a snack for your kiddos lunches or the office. Better yet, grab your mix and head out for a stroll or hike, or take along on your next road trip or adventure in Nevada’s rugged, desert locales.
Read More About Make Your Own Trail Mix: 4 Quick and Easy Recipes
-
Air Guard RN Makes an Impact in Community and Beyond
Everyday, Renown salutes its more than 150 active military and veterans on staff. Becca Gilbert, a Renown trauma nurse, is an example of the many outstanding service members at Renown who are serving both their country and their community. Becca Gilbert, BSN, RN, wears many uniforms. When she’s not wearing scrubs in her role as a trauma nurse in the intensive care unit of Renown Regional Medical Center, she’s wearing fatigues as a first lieutenant in the Nevada Air National Guard. “Service is huge,” says Becca Gilbert, RN, of her role in the Air Guard. “It’s something that is ingrained in me and a big part of who I am as a person. I find a lot of pride in being a part of something that is bigger than what is going on in my world.” Renown Health was named one of 15 recipients across the nation — and the only health system in the U.S. — for the Department of Defense’s highest employer award, the Secretary of Defense Employer Support Freedom Award, for exceptional support of its military employees. The Employer Support of the Guard and Reserves and Renown held a ceremony June 29 to recognize the award and to honor representatives of Renown who currently serve in the Guard and Reserves. With her Air Guard background, Gilbert is preassigned veteran patients at the Renown ICU. She says she’s able to relate to the veterans and their families and create a quick bond with them. “I’ve been assigned patients who are guard members with traumatic injuries — it’s good but hard,” Gilbert explains. “But I really love working with patients who are veterans.” Gilbert’s first career was as a veterinarian technician. Then enlisted in the Nevada Air National Guard in August 2008 — following in her father’s footsteps — and trained to serve as an EMT. While she was a medic, she went to nursing school for her second bachelor’s degree and was able to commission as an officer after graduation. Serving Our Community Gilbert says her work in the guard offers benefits that help with her job responsibilities at Renown, where she’s worked for four years. “At Renown, we are really a team and rely on each other to make sure there are good outcomes,” she says. “In the guard, officers are often put in charge, which teaches you a lot of things — organization, decision making and thinking of others. I think all of those things go hand-in-hand with my role as a nurse, especially in the ICU. People in the guard count on you as an officer and leader, and that is really important in the ICU when patients are counting on you for a positive outcome.” Gilbert’s responsibilities in the guard vary, including training for disaster relief missions and ensuring service members are fit and healthy enough to perform their jobs. “Training is a large part of the military — trauma training, physical fitness training and staying current on certifications,” she says. Locally she also leads the Self Aid Buddy Care program, a United States Air Force program that encompasses basic life support and limb-saving techniques to help wounded or injured personnel survive in medical emergencies until medical help is available. With the guard, Gilbert has also been involved in a bleeding-control program for volunteers in the community. She teaches community groups how to stop bleeding if they are a bystander to a car accident or other type of event, and is working with Renown trauma surgeon Marty Bain, M.D. to implement the program at Renown as well. Making a Difference Abroad In January, Gilbert was presented with an opportunity through the Nevada Guard State Partnership Program to travel outside the United States to the Kingdom of Tonga in the South Pacific and work at the Women and Children Crisis Centre, which assists families who are dealing with domestic violence. Gilbert praised the women who work at the center for their efforts towards change, as she says domestic violence is common in Tonga. “The women who work at the Women and Children Crisis Centre are pioneers,” she says. “They are trying to make changes by documenting what is going on and providing statistics to the lords and kings of Tonga. Some of it still isn’t accepted, but they continue to help the women and children of Tonga. They are helping so many people.” Renown Health salutes Gilbert for her tireless service to her country and her community here at home.
Read More About Air Guard RN Makes an Impact in Community and Beyond
-
The Journey Within: Helping Others Through Grief
Learn more about a Renown Health nurse who formed a nonprofit to help other families through loss. After the unexpected loss of her young husband, a Renown Health nurse turned her grief into helping other families navigate the loss of a family member. Jen Walker, RN, MSN, director of clinical excellence, lost her high school sweetheart and husband of eight years when he passed away in October 2015, while their two boys, age 7 and 9, lost their father. Walker, a nurse at Renown since 2003, was overwhelmed by the outpouring of support she received from the Reno community. It inspired her to want to help others in the same situation. “After Travis passed, the community did some amazing things for me,” Walker says. “I got really motivated to do the same thing and to give back, so that’s when I came up with starting The Journey Within.” The Journey Within organization provides support and resources for young families who have lost a close family member. Before officially starting her organization, Walker used some of the money she received after her husband passed and personally donated to three families. And with the help of four board members, Jen officially started The Journey Within in February 2017, and they have helped six families so far. One of the board members is her sister, Anny Goff. “She thought of creating this foundation in the darkest time of her family’s life,” Goff says. “She knew there would be other families that would need help and support and immediately wanted to help others. It showed incredible strength and courage to keep moving forward.” Nursing Careers at Renown Health Nurses at Renown Health demonstrate a commitment to patients and their families through the integration of care, clinical expertise, education, evidence-based practice and the pursuit of quality patient outcomes. Learn more about our mission, vision and values and the benefits of a career in nursing at Renown Health today. Explore Nursing at Renown Walker’s organization supports families through financial donations, which she funds through two yearly fundraisers. The Travy Tourney is a golf tournament held in memory of Travis, and the “Let’s Toast to Travis Fundraiser” event raffles prizes and merchandise. Along with financial support, The Journey Within helps families connect with other community resources, such as counseling and grief therapy services. Walker hopes to expand her nonprofit’s fundraising and support for families beyond the Reno-Tahoe community. Because of her outstanding work at Renown and in the community, Walker recently received a 20 Under 40 award from the Reno-Tahoe Young Professionals Network. She has also received a Women of Achievement award, a Leader of the Quarter award and has been nominated four times for Northern Nevada Nurses of Achievement. “She is strong and resilient and cares a lot about people,” says Jen Richards, chief nursing officer, acute care services. “She never settles for the status quo and is always pushing our team to do better.” In navigating her own loss and starting a nonprofit to give back, Walker has learned a lot about the community. “I’ve gained a tremendous amount of respect for the community as a whole, but especially for the young community,” she says. “Seeing the young people in the community who have been willing to give back and live really selflessly has been amazing to me.” As someone who lost her husband, helping young families who have gone through the loss of a close loved one can hit close to home for Walker, but that doesn’t stop her — it fuels her. “That’s one of the hardest parts about doing this — it takes you back a little bit,” she says. “But it’s just a very good reminder of ‘why.’ Because when I get to talk with these families, I realize that now I am that person who is there to listen. I just want them to know that they’re talking to someone who’s been through something similar.”
Read More About The Journey Within: Helping Others Through Grief
-
Caring for the Whole Family: Renown Nurse Helps Patient with Ailing Pet
Registered Nurse Tori Tembey (left) shared how her co-worker and fellow RN Jennifer Payne helped a patient with his pet's end-of-life arrangements. "It was such a selfless act that Jennifer took the time to do this for the patient.” Tembey says. Pets become members of our own family, and when they are ill or at the end of their lives, it can be devastating for their owners. During a hospital stay, a Renown patient was faced with the difficult decision to euthanize their terminally ill pet. A Renown registered nurse stepped in to help in some pretty remarkable ways. Back in high school, Jennifer Payne wanted to be a veterinarian. She worked in a veterinary hospital and planned to attend veterinary school, but struggled with some of the situations she faced. “I have a lot of compassion for animals,” Payne explains. “And some of the things I saw while working at the vet — like people bringing in their cat saying, ‘I’m moving, you need to put this cat down’ — wasn’t OK with me, and wasn’t what I wanted to do.” She changed course and went into nursing, but recently drew upon her early experiences working with pets and their owners to help a Renown patient in an extraordinary way. Payne now works in the trauma intensive care unit at Renown Regional Medical Center, where she recently observed a county animal control officer visiting a patient. The patient was visibly upset — they learned their dog was terminally ill and in poor health, and a veterinarian was recommending euthanasia. The patient had lost another dog just before Christmas. The patient hoped to have his ill dog similarly cremated, but animal control does not perform cremation. “I overheard all of this and thought, ‘this is the most horrible thing I’ve ever heard,’” Payne says. She offered to pick up the dog, have him cremated and bring the ashes to the patient. She also took up a collection with her Renown colleagues to pay for the cremation. The next day — her day off — Payne and her young daughter picked up the ashes and brought them to the patient at the hospital. “He couldn’t even talk because he was crying so much,” Payne says. “He said ‘I can’t thank you enough for all you’ve done. You’re a wonderful person.’ There was a friend in the room who asked what my daughter’s name was, and I said ‘Estelle.’ The friend said, ‘Estelle, your mother is an angel.’” Payne, who has a golden retriever of her own, says she knows what it’s like to have “fur babies,” and she could see how important this dog was to the patient. “It was great to be able to do this for him,” she says. Renown salutes nurses like Jennifer Payne, who are making a genuine difference everyday in the lives of patients and in the community.
Read More About Caring for the Whole Family: Renown Nurse Helps Patient with Ailing Pet
-
Make a Healthier Grilled Cheese Sandwich
Friday, April 12 is National Grilled Cheese Sandwich Day! So Let us help you create a healthier melt-in-your-mouth version to this popular cheesy sandwich. Ah, the grilled cheese. It’s the quintessential comfort food that not only pairs easily with a cup of soup, but it’s easy to whip together with just a few ingredients. There are many reasons to celebrate the gooey cheesiness of this toasted sandwich, but at nearly 700 calories, it’s definitely an occasional treat. But with just a few ingredient swaps — think light mayonnaise or toasting the bread in a toaster instead of slathering it in butter — you can remake your grilled cheese into a mouth-watering and nutritious meal. We’ve compiled a couple of easy substitutions, and some of our favorite healthy twists, so you can try a new variation of an old favorite. Be Choosy with Your Cheese It’s the star of your sandwich, but do you need to always grab the yellow slices? Try to opt for stronger flavors, like blue cheese or extra-sharp cheddar, to help you retain flavor while using less cheese on your sandwich. Better Bread Goes A Long Way Plain old white bread might be your toast of choice, but by choosing a whole wheat or multi-grain bread for your sandwich you’re not only adding in new crunch and flavor, you can also increase your fiber and nutrient intake. Hold the Butter Your mom, and maybe even your grandmother, probably spread a layer of butter on your grilled cheese throughout your childhood. But know this: It isn’t necessary. While butter helps crisp the crust, it doesn’t add too much in the way of flavor. Instead, brush the bread with olive oil, or try using a thin layer of reduced-fat mayonnaise or a creamy spread. Or skip grilling altogether by toasting your bread and then baking your sandwich open faced in the oven for a few minutes at 350 degrees. Healthier Options Looking for a new twist? Here are three incredibly tasty (and healthier) versions of the traditional grilled cheese sammy. 1. Baby Swiss And Tomato Grilled Cheese 2. Green Grilled Cheese 3. Spinach, Pesto & Havarti Grilled Cheese
-
11 Tips Caregivers Need to Know
Becoming a caregiver or playing a more active role in another’s healthcare is a big responsibility. At some point, almost all adults will support an aging parent or a loved one in need. Keeping track of their needs and wellbeing, while also prioritizing your own can become overwhelming. It’s important to know: you are not alone, and help is available. Read on for 11 tips to help you manage your time, your own wellbeing and your loved one’s care. Self-care comes first. When your main priority is the person in your life who needs care, it’s easy for your own needs to take the backseat. Give yourself time each day to focus on your personal wellbeing. It’s hard to give a loved one the care they need if your own needs are not met. Prioritize the Activities of Daily Living (ADL). Make a note of what ADLs your loved one can do alone, what they need help with and what activities require the most help. This will help you work through the day with them, as well as plan out how the day’s activities will go. Do a home safety audit. Do showers, bathtubs and steps have safety grab bars? Look around the house for additional tripping hazards, like rugs or electrical cords. If your loved one struggles with day-to-day navigation of the home, consider scheduling an occupational therapy appointment. This type of therapy helps a person develop or maintain the motions required to accomplish daily tasks. You might also qualify for a referral to in-home healthcare, such as Home Care. Have the hard conversation. The best time to discuss views about end of life care and to learn what choices are available is before a life-limiting illness or crisis occurs. With advance care planning, you can help reduce the doubt and anxiety related to decision making at the end of life. Completing an Advance Directive is a great tool to sort out all these decisions before they’re needed. Attend a free workshop to learn more and complete this important document. Identify when you need respite. Respite care involves receiving a short-term break from caregiving. Organizing in-home care for your loved one will allow you to step away and tend to your needs. By identifying what kind of respite care you are seeking, you can find the right person to provide you with that much-needed break. Don’t wait until you feel overwhelmed, plan ahead. Write down insurance contact information. Have a direct connection to the right insurance professional for support and advice. If your loved one is eligible Medicare, this is a good opportunity to review their current selections and if they would benefit from a Medicare Advantage Plan or Medicare Supplement Insurance. Seeking out expert advice or information on Medicare options is a great way to navigate this. Consider calling a broker, or attend a free educational seminar with Senior Care Plus. Gather legal and financial information. Make a list of all existing legal documents and financial accounts that your loved one has. These might include a will, advance directive, power of attorney, bank accounts or investment accounts. If you have questions about how to manage them, or need assistance in setting up additional framework, reach out to a lawyer, legal service, financial adviser or bank representative. Create an inventory of medical information. Identify where all of your loved one’s medical records are, as well as a list of providers or healthcare practices where they have received care. Consider if you should have your loved one give you Proxy Access in MyChart, which allows you to access all the features in MyChart on their behalf, including viewing upcoming appointments, viewing test results and emailing a doctor on their behalf. Make a list of what others can do. Think about all the little (and big) things that need to happen, and write down tasks that others could take care of you. When someone says “let me know what I can do” you’ll be ready with a pre-written list of items they may be able to assist with. Tasks could include tackling around-the-house repairs, scheduling lawn work, helping to walk the dog, taking a car for an oil change and cleaning. Find programs and events for social enjoyment. If and when possible, seek an activity outside of the home. Look for community centers that have programs for seniors, recreational activities or meals that you can patriciate in together. If leaving the home is not an option, arrange for visits or in-home activities, such as movie nights, card games or time to visit with family. Research long-term options. If you will be considering a nursing home or assisted living, make a list of amenities that you and the person you are caring for would like. Take this list with you when visiting potential locations to make sure you don’t forget to ask about each item.
-
Getting to Know Stephanie Kruse
There are a lot of impressive titles you can use to describe Stephanie Kruse: entrepreneur, marketer, philanthropist, leader, adventurer, nurse. And now with her planned gift to the Renown Health Nursing Excellence Endowment, she can add one more to the list: a member of the Renown Legacy Society – a group of visionary supporters who have chosen to make a lasting commitment to the future health and wellbeing of northern Nevadans. This generous planned gift comes on the heels of a significant cash gift made to the Nursing Education Fund last summer. Stephanie is an inspiring example of someone who has dedicated her life to helping others. The daughter of a nurse and a retired nurse herself, Stephanie knows the hard work, selflessness and dedication it takes to create a successful business and community. As Chair of the Renown Health Foundation Board of Directors, she also understands the importance of attracting and retaining nurses within a healthcare system. As a way to contribute to a cause near and dear to her heart, she decided to include the Renown Nursing Excellence Endowment as a beneficiary of her retirement plans. “I wanted to honor the memory of my mother, who was a registered nurse in a small-town hospital in Iowa.,” said Stephanie. “I was always very conscious of her passion for providing great care to her patients, and I wanted to provide funding for others interested in nursing.” Across the nation, health systems are facing a shortage of nurses and nursing-related professionals. Renown is proactively implementing programs to build our pipeline of potential future nurses and keep those already in the field. Stephanie’s generous gift will help the endowment provide programs such as training, scholarships, loan repayment and professional development to increase retention and recruitment of prospective nurses. “As nurses, we are entrusted with our patients’ lives,” said Melodie Osborn, Chief Nurse Executive at Renown Health. “We have the privilege of caring for people in their most vulnerable time and helping those who cannot help themselves. Stephanie’s generous gift to the Nursing Excellence Endowment Fund will help us develop new nurses for the future so we can continue to provide care to those in need for generations to come.” No Stranger to Healthcare Long before she found herself leading the Renown Health Foundation Board, Stephanie learned the ins and outs of healthcare. She graduated from nursing school and became a part-time nurse in a Sioux Falls, South Dakota nursing home while attending Augustana College to obtain a degree in journalism and a minor in theater. As part of her journalism program, Stephanie completed an internship in the public relations department of a Sioux Falls hospital, and that led to her accepting a position as director of public relations at a sister hospital. She later was recruited by Saint Mary's Hospital and moved to Reno to be the director of marketing in 1981. She stayed at Saint Mary's for almost 10 years before starting her own company in pursuit of her passion for marketing strategy. Since launching her brand, Stephanie has grown KPS3 to a multi-million-dollar firm with more than 60 staff members. Somehow, she is still able to find time to serve on six (!) volunteer boards, most of which are dedicated to improving access to better health and human services. “I have a soft spot in my heart for organizations who strive against all odds to help those with the greatest needs,” said Stephanie.
-
Beyond Jello A Healthier Approach to Hospital Food
Hospital food gets a bad rap and maybe it’s deserved. However, at Renown Health we strive to serve patients, visitors and staff meals that are both nutritious and delicious. In this video and blog post, Renown Health President and CEO, Tony Slonim, M.D., Dr.PH., FACHE, shares his thoughts on hospital food and modeling healthy lifestyles. Everyone knows that what we eat matters for almost every aspect of our health. Eating well can prevent chronic disease, control weight, improve our mood and even strengthen our bonds with loved ones as we come together to enjoy a family meal. Yet despite this knowledge, balancing work or school responsibilities, family life and everything in between can make eating healthy feel like an uphill battle. Recognizing this challenge, Renown Health invests in programming to help our community embrace healthy lifestyle habits – starting with our own employees. Knowing that people often look to their healthcare providers to model healthy behavior, we are deliberate in our efforts to help our employees and their families live well. We also provide healthy dining options in our on-campus restaurants and through our food and nutrition services team. We believe that providing nutritious, appetizing meals helps patients to recuperate from illness or injury, helps their families recharge, and helps our staff fulfill their promise of providing outstanding care. We hope that by serving as models of healthy behaviors, our employees will inspire others to join us in this journey. Dr. Slonim on Twitter | @RenownCEOTonyMD Interested in learning more of Dr. Slomin’s thoughts on health and healthcare? Engage with him on Twitter. Follow Tony
Read More About Beyond Jello A Healthier Approach to Hospital Food
-
Cancer Nutrition - Helpful Tips to Support Your Loved One to Eat Healthy
Eating healthy is a daily challenge for many, but for those with cancer it is an even harder struggle. A cancer diagnosis not only impacts those diagnosed, but family members and friends too. One key area of concern is making sure your loved one stays well by eating healthy food every day. Here are some essential cancer nutrition tips from Renown Health registered dietitians Jessica Blauenstein and Amy Laster. Help to Prepare Meals and Snacks for Daily Cancer Nutrition Make it grab and go. Easy-to-make meals help reduce the burden of having to cook and prepare food. Having easy to grab snacks on the counter or in the fridge can help ensure your loved one has access to those nutrients when needed. Sit outside of the kitchen. This allows your loved one to avoid cooking smells which can make them feel sick as a side effect of cancer treatments. Also try serving them cold foods such as sandwiches, cheese and crackers, or shakes which have a mild scent. Try drinkable meals. Some people with cancer find it easier to sip their calories over the course of 30 minutes to an hour. Consider smoothies or supplemental shakes such as Ensure Enlive or Boost Plus as snacks not meal replacements. A great foundation for a smoothie is a protein source (Greek yogurt, protein powder, nut butters or milk) with a carbohydrate (fruits, juice or berries). Add other ingredients as desired, such as spinach, kale, and ground flaxseed or chia seeds to give it more vitamins, minerals, and fiber. Snack Ideas for Those Undergoing Cancer Treatment The following ideas are both quick and easy to make for your loved one. Chicken or tuna salad with whole grain crackers or as a sandwich on whole grain bread Greek yogurt mixed with cereal, fruit and/or nuts Cottage cheese with banana, cinnamon and/or peanut butter Favorite fruit with 100% natural peanut or almond butter spread - Try peanut butter with bananas, apples, or even celery Their favorite veggies dipped in a salad dressing of your choice - For example, carrots with hummus or ranch dressing Cheese and whole grain crackers - Add tomato slices with a dash of oregano on top for more flavor Eggs scrambled with cheese, vegetables and/or salsa Peanut butter and jelly sandwich on whole grain bread A baked sweet potato with some favorite toppings Hard boiled eggs and/or egg salad with whole grain crackers, or as a sandwich on whole grain bread Oatmeal or cream of wheat prepared with milk, fruit and/or nuts Sometimes your loved one may not feel like eating or refuse to eat. If treatment side effects are impacting your loved one’s ability to eat, please visit the websites below containing recipes tailored to treat side effects. Cook for Your Life ELLICSR Of course you may also consult a registered dietitian and/or the patients care team, if you have more cancer nutrition concerns. No Appetite? Assisting with Cancer Taste Changes Taste changes are common during cancer treatment. Patients experiencing these changes may not feel like eating, which can negatively impact their nutrition. Help your loved one overcome taste changes with these cancer nutrition strategies: Metallic or bitter taste in food - add something sweet such as maple syrup, honey or jelly. You may also try adding fat, such as a nut butter, avocado or regular butter. Pickles or vinegar could help with this too. A taste like cardboard - try adding salt and extra flavor to foods with seasonings and spices. Some examples are onion, garlic, chili powder, basil, oregano, rosemary, tarragon, barbecue sauce, mustard, ketchup, or mint. Lemon juice, citrus, vinegar, or pickles may also help with this as well Food tastes too sweet - try adding six drops of lemon or lime juice. Add small amounts until the sweetness is gone. Very salty taste - try adding ¼ teaspoon of lemon juice. Try plastic utensils instead of metal, especially if your loved one is struggling with foods tasting metallic. Dipping small bites of food into either lemon juice or vinegar can have a “palate cleansing” feel and may improve taste perception. This helps avoid getting tired of the flavor after a few bites. Try marinating food or meats in sweet fruit juices, salad dressings, or sweet-and-sour sauce. Other “palate cleansing” foods are lime juice, orange juice, mangos, lemongrass, parsley, cilantro, mint, ginger, basil, and pickled foods. Use aroma to make foods appealing, avoiding any smells that may cause nausea. In particular, cinnamon, nutmeg, cloves, coriander, cumin, ginger, and black pepper can add an aromatic flavor. Also include herbs such as oregano, rosemary and thyme. Think texture. Consider trying wafers, crunchy nut butters, carrots, celery, cucumbers, chips, rice crispies, corn flakes, crackers, panko crumbs, nuts, or seeds if you are able to chew and swallow them safely. Remember that patience with your loved one's changing appetite and tastes can be the strongest form of support you can provide. Nutrition Tips for Cancer Survivorship and Beyond If eating large meals is difficult for your loved one, encourage them to snack throughout the day. Aim for 4-6 snacks or small meals per day. Focus on consuming 2-3 protein-rich foods each day such as lean animal meats, fish, eggs, soy or a protein supplement with 20-30 grams of protein per serving. Eat a variety of brightly colored fruits and veggies. Aim to make half of each meal fruits and vegetables. Eat less than 18 oz. (cooked weight) of red meat per week. Limit cold cuts, bacon, sausage, and hot dogs. Avoid excess salt and saturated fats. Cut back on simple carbs. (i.e. desserts, candies, white bread/pastas, french fries, packaged foods, chips) Drink in moderation- if at all- one drink per day for women, two for men. Get enough vitamin D (through diet and/or supplement) Avoid tobacco of any kind. Keep a healthy weight and stay up on exercise. Other Ways to Help a Loved One with Cancer Assist with Chores Allow your loved one to relax as you help take care of chores around the house, such as cleaning, cooking and grocery shopping. This may reduce overall stress and can be helpful for those that get tired after their treatments. Physical activity can still be beneficial, so be sure to do an activity together that they enjoy and is approved by their doctor. Be Patient It can be very difficult to see a loved one go through cancer treatment. Remember to be patient with your loved one. There may be things we want them to do or eat that we know would be good for them, however, meet your loved one with grace and understanding. It is ultimately their decision on what to do, just be there to support and assist them as they go through this challenging time. Additionally, Renown hosts free “Eating Well After Cancer Treatment” nutrition classes for cancer survivors. Our next cancer nutrition class series starts Thursday, June 3, 2021, and will be hosted virtually. It is open to anyone in the community. For more information or to register please click here.
Read More About Cancer Nutrition - Helpful Tips to Support Your Loved One to Eat Healthy
-
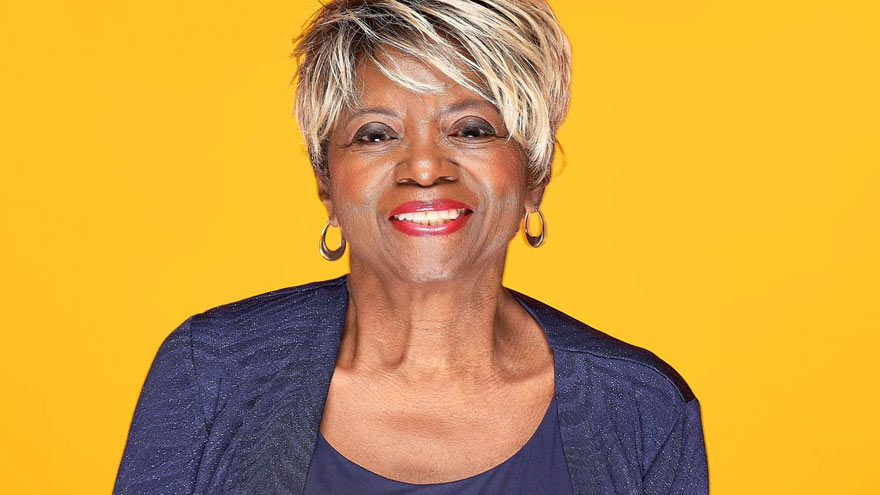
Simply Spectacular Sterling Silver Member Rhogenia
Whether watching a 4th of July celebration from her father’s boat on the Saint Johns River or sneaking a peek at a post-game display over Gator Bowl Stadium from her parents’ bedroom window, the fondest childhood memories of Sterling Silver Club featured member are of fireworks. “I love watching fireworks,” says Rhogenia. “And I get just as excited by them now as I did then.” Well, fireworks are certainly a fitting introduction to this Sterling Silver Club member who shines with a spectacular collection of accomplishments, adventures and interests. A Passion for Teaching Rhogenia remembers herself as a happy, carefree child “who read all the time” while growing up in Jacksonville, Florida with her younger sister, Rosemary, and her father and mother, who was a public school teacher. It’s easy to see how this natural enthusiasm for reading (and learning), along with her mother’s influence, would spark Rhogenia’s calling – and passion – for teaching. After earning her bachelor’s degree in education, Rhogenia spent the first 2 years of her career as a kindergarten teacher in a “one traffic light” town in her home state. She then moved to Oakland, California where she taught kindergarten and first grade classes at various schools for 4 years. The Biggest Little City in the World came next, and her stay there would last much longer. In Reno, Rhogenia added a master’s degree to her credits and found a home for her teaching career at Grace Warner Elementary School – where she taught first and second grade for 20 years! During that time, she also took on the additional role of adjunct professor, teaching graduate students for the University of Phoenix, College of Education. “A great teacher never stops learning,” explains Rhogenia. “I believe the art of teaching is the act of facilitating discovery, for students and also for myself.” In recognition of her efforts, Rhogenia received the Reno Gazette Journal’s Best of Education Award, the Washoe County Teachers Association Distinguished Performance Award, and was also awarded a grant from Learn and Serve America to help her support student programs that gave back to the community. Rhogenia’s favorite quote: “One hundred years from now it will not matter what my bank account was, the sort of house I lived in, or the kind of car I drove. But the world may be a little better, because I was important in the life of a child.” – Adapted from an essay by Forest Witcraft Commissions, Councils & Space Camp Life outside the classroom also kept Rhogenia busy – and inspired – throughout her career. In 1998, she was selected to participate in an educator externship, and in 1999, was chosen to be a teacher consultant to the Alliance Summer Geography Institute. These opportunities allowed Rhogenia to return to her students with exciting lessons to share about different types of industries and the importance of geography, respectively. In 2002, the governor appointed her commissioner for the state of Nevada’s Commission on Professional Standards in Education. And Rhogenia followed that up with an appointment to the National Council for Accreditation of Teacher Education in 2004. She also got to travel. Rhogenia was one of two teachers from Nevada chosen to participate in the Japan Fulbright Memorial Fund Teacher program on its 50th anniversary. Originally established in 1946 to foster mutual understanding between the U.S. and Japan, the trip allowed Rhogenia to represent her state, her country and her race to Japanese dignitaries, business people and students alike. For over three weeks, she toured schools, universities, factories, temples, art galleries and museums, and stayed in the home of a Japanese family for a few days – which she calls the highlight of her trip. Oh, and then there was the time she went to space camp! The Nevada Teacher in Space Program sent Rhogenia to join teachers from across the county at the out-of-this-world camp in Huntsville, Alabama. On “Team Endeavor,” she learned what it would be like to deliver payloads and perform experiments at the International Space Station, and took a seat in flight simulators and an antigravity chair. The goal of the program was to inspire teachers to help their students learn about the infinite possibilities of math and science. Time for What Matters These days, Rhogenia enjoys spending time on the things that matter most to her. Personally, that means diving into hobbies like genealogy, music, reading, writing, cooking and the occasional card or board game. She also continues to learn and broaden herself through Osher Life Long Institute (OLLI) classes and Retired Living Truth Series seminars. But her greatest joy comes from spending time with family – four generations of her own family, her church family, retired teachers from Warner Elementary and the many acquaintances and friends she’s come to know over the years. Other things worthy of Rhogenia’s time: Giving back to the community, rainbows, sunsets and sometimes, just watching the clouds roll by. Membership & Senior-ship What does Rhogenia think about being a Sterling Silver Club member and a senior? She told us. “Before COVID, it was the face-to-face club events that I liked most,” recalls Rhogenia. “At the Silver Stars Gala, I had such a wonderful time chatting with old and new friends… the fashions, decorations and the food were delightful.” Over the past year, she also found things to love about the club’s virtual events and regularly attends lectures, cooking and yoga classes and weekly meditation sessions – from her home! It Starts with Hello offers some of her favorite club events. “It reminds me of the television show, Cheers, where everybody knows your name!” she grins. “We meet at noon on Tuesdays and Thursdays. There are a variety of topics and guest speakers, and with the virtual events, I feel like the presenters are talking directly to me… I have the best seat in the house.” As far as being a senior goes, Rhogenia is living her best life and has some advice to help others do the same. “As a senior, I have the time to explore and take advantage of the many opportunities available out there,” she says. “I live life in the present and to the fullest. I make the most of each day because tomorrow, it will be the past.” Rhogenia feels that the biggest challenges for seniors today are health and isolation, and wants people to know there’s help if they need it. “Sometimes we need a little help to make everyday activities a little easier, or just need a person to talk with,” she explains. “My advice is never be too proud to ask for help with anything! Most people are glad to help or guide you to someone who will.” “Lastly, to seniors, I would like to say this: Love yourself and make peace with who you are and where you are at this moment in time,” Rhogenia continues. “And give yourself a big hug!” The Sterling Silver Club thanks Rhogenia for dazzling us with her story, her friendship and her collaboration – and we send her and all of our members a “BIG hug.”
Read More About Simply Spectacular Sterling Silver Member Rhogenia
-
Fall Recovery Gets Patient Back to Life and Movement
Standing at the top of the stairs to the basement Sharon Sturtevant was chatting with her grandson in the kitchen. Suddenly, Sharon stumbled and fell down the stairs. “The last thing I remember was my head hitting the floor before everything went black,” she recalls. Her grandson, Oliver, quickly called 911 and paramedics arrived on the scene, taking her by ambulance to Renown Regional Medical Center where she was diagnosed with a broken collarbone and a neck fracture that would require complex surgery involving fusion of her neck. Fall Recovery Begins After her surgery, Sharon was transported to the Renown Rehabilitation Hospital and her recovery process began. Sharon smiles as she describes the rehab hospital team “They are fabulous here, I learned so much about how my body moves, and the proper way to move it. At home I wouldn’t have known what to do,” she confesses. “They set me up for success to return home and not get injured again.” At Renown Rehabilitation Hospital, different therapists coordinated a custom plan to help Sharon recover from her injuries. Ultimately, the goal of her physical therapy was to help restore and improve her strength, reduce pain and increase her mobility for stamina and balance. Physical Therapy Key to Successful Treatment of Falls “My recovery after the operation was an eye-opener,” Sharon declares. “I had no idea how much went into regaining everyday moment.” During her rehabilitation hospital stay, she had to re-learn how to swallow, go up and down stairs, as well as successfully get in and out of a wheelchair, which involved transferring her body weight safely. Due to hormonal changes after menopause women are 50% more at risk for falls than men, according to research. Sharon now has a greater awareness of how to move her body and is significantly stronger than before entering her physical rehabilitation sessions. Not everyone knows that everyday mobility is impacted by four basic skills: stepping, trunk flexibility, upright posture and weight shifting. “I don’t know how I could have gotten this far without the wonderful therapists here,” she shares. “They are so thorough. Proper alignment was encouraged helping me to walk and stand correctly. They were all so nice and patient with me,” she states. “I actually had less pain because I didn’t hurt myself moving the wrong way.” Falls Are Common Among Aging Adults As we age balance becomes more important. Unfortunately falls are common among older adults with negative quality of life effects, even fatalities. According to the Centers for Disease Control and Prevention (CDC), one in four seniors fall each year in the U.S. A comprehensive physical therapy plan for sudden falls or chronic conditions is a safe, effective alternative treatment to medication such as opioids. Today Sharon is back at home with a new banister installed on the basement stairs. As a music lover she is enjoying her musical grandchildren Oliver and Eliana who play instruments. She looks forward to attending their upcoming school concerts. Sharon remembers the staff at Renown Rehabilitation Hospital fondly, “They were unfailingly patient, supportive, informative and understanding.” Her advice to those unexpectedly finding themselves in the rehabilitation hospital is, “Listen to your therapists carefully and follow their instructions.”
Read More About Fall Recovery Gets Patient Back to Life and Movement